Preoperative blood ordering is frequently used in elective colon surgery, even for procedures that rarely require blood transfusion. Most often this procedure is performed without proper analysis of the real needs. The aim of this study was to evaluate the patients who receive transfusion and to determine their associated factors.
MethodsRetrospective study of all consecutive patients scheduled for elective colon surgery was carried out at 2007–2012. Several clinico-pathological and surgical variables were analysed and predictive blood transfusion indices such as the cross-matched/transfusion ratio (C/T ratio), transfusion index and transfusion probability were calculated. Patients were divided into 2 groups accordingly whether they have received perioperative surgical transfusion or not.
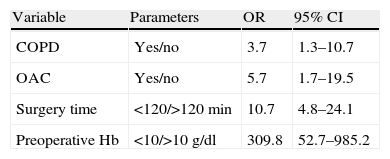
ResultsThere were 457 surgery patients. A total of 171 blood units, in 74 patients were perioperatively transfused. Overall cross-matched transfusion ratio was 5.34, the transfusion probability 162%, and the transfusion index 0.18. Variables that were significantly associated with receiving blood transfusion in a multivariable analysis were a preoperative haemoglobin level less than 10g/dl (OR: 309.8; 95% CI: 52.7–985.2), chronic pulmonary obstructive disease (OR: 3.7; 95% CI: 1.3–10.7), oral anticoagulant therapy (OR: 5.7; 95% CI: 1.7–19.4) and surgical time over 120min (OR: 10.7; 95% CI: 4.7–24.1).
ConclusionsLikelihood of receiving perioperative transfusion in elective colon surgery is very low. Among their associated factors, the haemoglobin level less than 10g/dl is the one with strongest association. Those patients with such low preoperative haemoglobin level should not be scheduled for elective colon surgery until they received specific treatment.
La solicitud de sangre preoperatoria en cirugía programada de colon es una norma frecuente, incluso en aquellos procedimientos con escasa probabilidad de transfusión. El objetivo de este estudio es evaluar la proporción de pacientes que reciben transfusión peroperatoria y determinar sus factores asociados.
MétodosEstudio retrospectivo de pacientes consecutivos en cirugía electiva de colon en el periodo 2007-2012. Se analizan variables clinicopatológicas, quirúrgicas y se calculan la ratio sangre «en reserva»/sangre transfundida (ratioC/T), la probabilidad de transfusión y el índice transfusional. Los pacientes se dividen en 2 grupos en función de haber recibido o no transfusión peroperatoria.
ResultadosSe contabilizan 457 pacientes, transfundiéndose 171 unidades sanguíneas en 74 pacientes, siendo la probabilidad de transfusión del 16,2%, la ratio C/T de 5,34 y el índice transfusional de 0,18. Las variables que se han asociado significativamente a recibir transfusión sanguínea tras el análisis multivariable son: la cifra preoperatoria de hemoglobina inferior a 10g/dl (OR: 309,8; IC 95%: 52,7-985,2), enfermedad pulmonar obstructiva crónica (OR: 3,7; IC 95%: 1,3-10,7), anticoagulación oral (OR: 5,7; IC 95%: 1,7-19,4) y tiempo quirúrgico superior a 120min (OR: 10,7; IC 95%: 4,7-24,1).
ConclusionesLa probabilidad de necesidad de transfusión en pacientes a los que se les realiza cirugía electiva de colon es baja. Entre los factores asociados, la cifra de hemoglobina preoperatoria inferior a 10g/dl es el que presenta una mayor fuerza de asociación. Los pacientes con dichas cifras de hemoglobina preoperatoria no deberían ser intervenidos en cirugía electiva de colon hasta haber recibido tratamiento apropiado.
The routine ordering of cross-matched blood for elective colon surgery is a widely established procedure. However, there are very few surgical procedures which entail a high risk of perioperative haemorrhage and thus require blood transfusion.1–4 Therefore the routine preparation of cross-matched blood is an inefficient use of resources and places a burden (in terms of time and cost) on hospital blood bank personnel.4
Furthermore the association between perioperative blood transfusion and a higher morbimortality rate is widely accepted.5–11
Patients need to be optimally prepared preoperatively and a series of intraoperative measures are implemented by anaesthetists and surgeons to avoid perioperative blood transfusion and minimise its adverse affects in elective surgery of the colon.5,6,10,12
Different factors need to be defined that could be indicative of the need for perioperative transfusion, and protocols should be established for preoperative blood ordering which are relevant to each surgical procedure and serve as guidelines for more “rational” and efficient use of blood transfusion. These programmes attempt to link the number of cross-matched blood units with the real number of blood units transfused.1,2
We present a retrospective study of 457 consecutive cases of patients who underwent elective colon surgery in order to determine whether cross-matched blood ordering meets the real requirements for perioperative transfusion and to identify predictive factors.
Materials and MethodsA retrospective, observational, epidemiological study including 457 patients treated consecutively by elective colon surgery, during the period from January 2007 to September 2012. Pretransfusion tests were requested for all the patients for the preparation of two units of preoperative cross-matched packed red blood cells (914 units in total). The patients were divided into two groups depending on whether or not they had received a transfusion of, at least, one unit of packed red cells during surgery and in the first 24h following surgery. The study variables were divided into three groups: the first included the gender and age, preoperative diagnosis (classified as benign or malignant disease), and the anatomical location in the colon (right colon, left colon and entire colon); a second group comprising the preoperative variables and comorbidities of the patient, such as previous abdominal surgery, preoperative haemoglobin count (Hb) of less than or exceeding 10g/dl, arterial hypertension (HTA), diabetes mellitus (DM), heart disease (CARD), chronic renal failure (CRF), chronic obstructive pulmonary disease (COPD) and administration of corticosteroids (CORT), oral anticoagulants (OAC) and anti-platelet agents (APA); and finally a third group including operative variables including operation time exceeding or less than 120min, and the surgical technique used, summarised in terms of resection and primary anastomosis techniques (R+A), and other techniques.
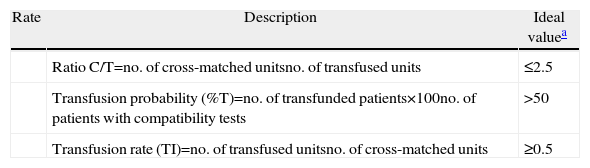
The following transfusion rates were calculated (Table 1): cross-match-to-transfusion ratio compatibility tests (C:T ratio), transfusion probability (%T) and transfusion rate (Ti). The descriptive analysis was undertaken using means and standard deviation for the quantitative variables, and absolute and relative frequencies (percentages) for the categorical variables. Univariable statistical analysis comparing transfusion/non-transfusion groups was performed using the Student's t test for continuous variables and the chi-square test for categorical variables. Multiple logistic regression analysis, step-by-step maximum likelihood method, was used to assess the factors associated with receiving a blood transfusion after adjusting possible confounding effects. The dependent variable was blood transfusion (yes/no), whereas the independent variables included were the significant variables in the univariable analysis or with biological plausibility. The results are presented in odds ratio (OR) and 95% confidence interval (95% CI). The receiver operating characteristic curve (ROC curve) was calculated to obtain the sensitivity/specificity for each probability value, selecting the best overall value as the cut-off point. The value of the area under the curve and its 95% confidence interval are presented (95% CI).
Calculated Transfusion Rates.
| Rate | Description | Ideal valuea |
| Ratio C/T=no. of cross-matched unitsno. of transfused units | ≤2.5 | |
| Transfusion probability (%T)=no. of transfunded patients×100no. of patients with compatibility tests | >50 | |
| Transfusion rate (TI)=no. of transfused unitsno. of cross-matched units | ≥0.5 |
The accepted level of statistical significance was P≤.05. The data were analysed using the statistical programme SPSS, version 15.0.
ResultsOf the 457 patients included in the study, 239 were males (52.3%) and 218 females (47.7%), the average age of the patient was 69.6±12.4 (range 21–94). As per the diagnosis, 78 patients had benign disease (17.1%) and 379 cases had malignant disease (82.9%). The benign diagnoses were: adenomas (33), ulcerative colitis (3), Crohn's disease (1), diverticular disease (37), lipomas of the colon (2) and one patient had sigmoid volvulus. The diseases classified as malignant were 374 cases of adenocarcinoma, one neuroendocrine carcinoma, one Gardner's syndrome, one Lynch syndrome and two cases of high grade appendicular mucinous tumours. The anatomical location was: right colon (191 cases: 41.8%), left colon (242 cases: 53.0%), and entire colon (24 cases: 5.3%).
In terms of preoperative data and prior clinical history: 43 patients (9.4%) were identified with Hb levels lower than 10g/dl, 165 patients (36.1%) had a history of previous abdominal surgery.
Comorbidities recorded were: HTA (202 cases: 44.2%), DM (86 cases: 18.8%), CARD (74 cases: 16.2%), CRF (13 cases: 2.8%) and COPD (49 cases: 10.7%). Patients on oral CORT medication (6 cases: 1.3%), OAC medication (29 cases: 6.3%) and APA medication (43 cases: 9.4%) were also identified.
Two groups of surgical procedures were defined: R+A (423 patients: 92.5%) and other procedures (34 patients: 7.5%). Two groups of patients were established in terms of duration of surgery: those with a surgical time of less than 120min (401 patients: 87.7%), and those with a longer duration of surgery (56 patients: 12.3%).
74 patients received a transfusion (16.2%), with a total of 171 units (an average of 2.3 units per patient). The total preparation time by blood bank personnel was 286h, with an average 38min per patient.
The overall cost, taking into account only the pretransfusion compatibility tests, came to 18,654.82 €, with an average of 40.82 € per patient.
The transfusion rates calculated were: C:T ratio=5.34; %T=16.2% and Ti=0.18.
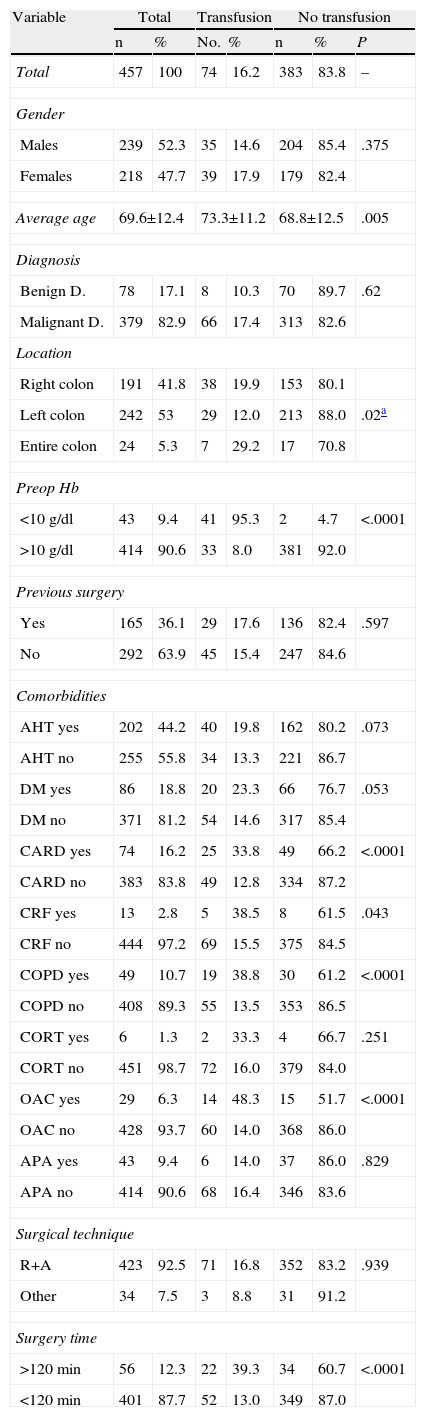
The results of the univariable analysis are shown in Table 2. There are significant differences with regard to age and the group which had received a transfusion being older (73.3±11.2 compared to 68.8±12.5 years of age; P=.005).
Univariable Analysis.
| Variable | Total | Transfusion | No transfusion | ||||
| n | % | No. | % | n | % | P | |
| Total | 457 | 100 | 74 | 16.2 | 383 | 83.8 | – |
| Gender | |||||||
| Males | 239 | 52.3 | 35 | 14.6 | 204 | 85.4 | .375 |
| Females | 218 | 47.7 | 39 | 17.9 | 179 | 82.4 | |
| Average age | 69.6±12.4 | 73.3±11.2 | 68.8±12.5 | .005 | |||
| Diagnosis | |||||||
| Benign D. | 78 | 17.1 | 8 | 10.3 | 70 | 89.7 | .62 |
| Malignant D. | 379 | 82.9 | 66 | 17.4 | 313 | 82.6 | |
| Location | |||||||
| Right colon | 191 | 41.8 | 38 | 19.9 | 153 | 80.1 | |
| Left colon | 242 | 53 | 29 | 12.0 | 213 | 88.0 | .02a |
| Entire colon | 24 | 5.3 | 7 | 29.2 | 17 | 70.8 | |
| Preop Hb | |||||||
| <10g/dl | 43 | 9.4 | 41 | 95.3 | 2 | 4.7 | <.0001 |
| >10g/dl | 414 | 90.6 | 33 | 8.0 | 381 | 92.0 | |
| Previous surgery | |||||||
| Yes | 165 | 36.1 | 29 | 17.6 | 136 | 82.4 | .597 |
| No | 292 | 63.9 | 45 | 15.4 | 247 | 84.6 | |
| Comorbidities | |||||||
| AHT yes | 202 | 44.2 | 40 | 19.8 | 162 | 80.2 | .073 |
| AHT no | 255 | 55.8 | 34 | 13.3 | 221 | 86.7 | |
| DM yes | 86 | 18.8 | 20 | 23.3 | 66 | 76.7 | .053 |
| DM no | 371 | 81.2 | 54 | 14.6 | 317 | 85.4 | |
| CARD yes | 74 | 16.2 | 25 | 33.8 | 49 | 66.2 | <.0001 |
| CARD no | 383 | 83.8 | 49 | 12.8 | 334 | 87.2 | |
| CRF yes | 13 | 2.8 | 5 | 38.5 | 8 | 61.5 | .043 |
| CRF no | 444 | 97.2 | 69 | 15.5 | 375 | 84.5 | |
| COPD yes | 49 | 10.7 | 19 | 38.8 | 30 | 61.2 | <.0001 |
| COPD no | 408 | 89.3 | 55 | 13.5 | 353 | 86.5 | |
| CORT yes | 6 | 1.3 | 2 | 33.3 | 4 | 66.7 | .251 |
| CORT no | 451 | 98.7 | 72 | 16.0 | 379 | 84.0 | |
| OAC yes | 29 | 6.3 | 14 | 48.3 | 15 | 51.7 | <.0001 |
| OAC no | 428 | 93.7 | 60 | 14.0 | 368 | 86.0 | |
| APA yes | 43 | 9.4 | 6 | 14.0 | 37 | 86.0 | .829 |
| APA no | 414 | 90.6 | 68 | 16.4 | 346 | 83.6 | |
| Surgical technique | |||||||
| R+A | 423 | 92.5 | 71 | 16.8 | 352 | 83.2 | .939 |
| Other | 34 | 7.5 | 3 | 8.8 | 31 | 91.2 | |
| Surgery time | |||||||
| >120min | 56 | 12.3 | 22 | 39.3 | 34 | 60.7 | <.0001 |
| <120min | 401 | 87.7 | 52 | 13.0 | 349 | 87.0 | |
OAC, oral anticoagulants; APA, anti-platelet agents; CARD, heart disease; CORT, corticosteroids; DM, diabetes mellitus; D, disease; COPD, chronic obstructive pulmonary disease; AHT, arterial hypertension; CRF, chronic renal failure; R+A, resection and anastomosis techniques.
With regard to preoperative diagnosis, there was no significant difference in the comparison between benign and malignant diseases. In the distribution of diseases according to their anatomical location in the colon, we can see that the group which behaved differently to the other two was the left colon group, i.e., a greater risk of requiring a blood transfusion was found in the right colon group compared to the left colon group (19.9% compared to 12.0% respectively), and in the entire colon group compared to the left colon group (29.2% compared to 12.0% respectively). The differences in the right colon and the entire colon compared to the left colon are statistically significant (P=.02).
There are also significant differences in terms of preoperative Hb level, in that 41 patients (95.3%) with an Hb lower than 10g/dl were transfused compared to 33 patients (8%) with an Hb above 10g/dl (P<.0001). There are no significant differences with regard to a history of previous surgery (17.6% compared to 15.4% transfused patients, respectively).
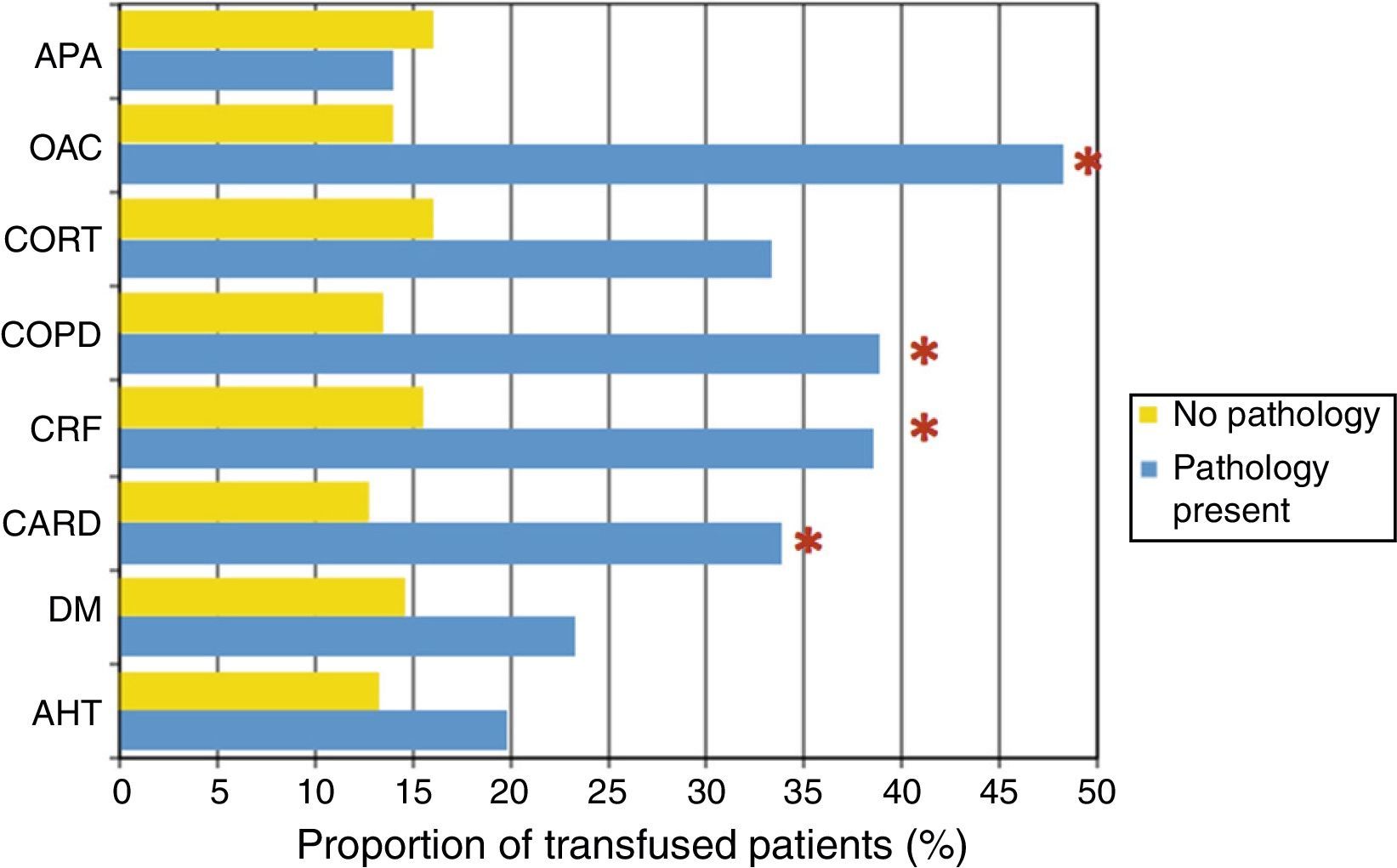
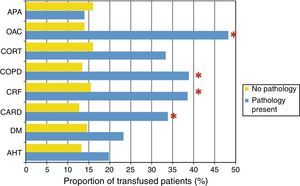
When studying the proportion of transfused patients according to comorbidities, it can be observed that patients with DM (P=.005), CARD (P<.0001), CRF (P=.043), COPD (P<.0001) or receiving OAC treatment (P<.0001) received more transfusions than those who did not have the illnesses diseases or who did not need the medication (Fig. 1).
Proportion of transfusions according to comorbidity. OAC: oral anticoagulants; APA: anti-platelet agents; CARD: heart disease; CORT: corticosteroids; DM: diabetes mellitus; COPD: chronic obstructive pulmonary disease; AHT: arterial hypertension; CRF: chronic renal failure.
*There are statistically significant differences between patients with the disease and patients without the disease (P<.05).
The surgical technique used did not show results of statistical significance in the analysis of both groups. On the contrary, the patients with a surgery time exceeding 120min represented 39.3% cases of transfusion, compared to 13.0% of cases in the group of patients with a surgery time of less than 120min; the difference is statistically significant (P<.0001).
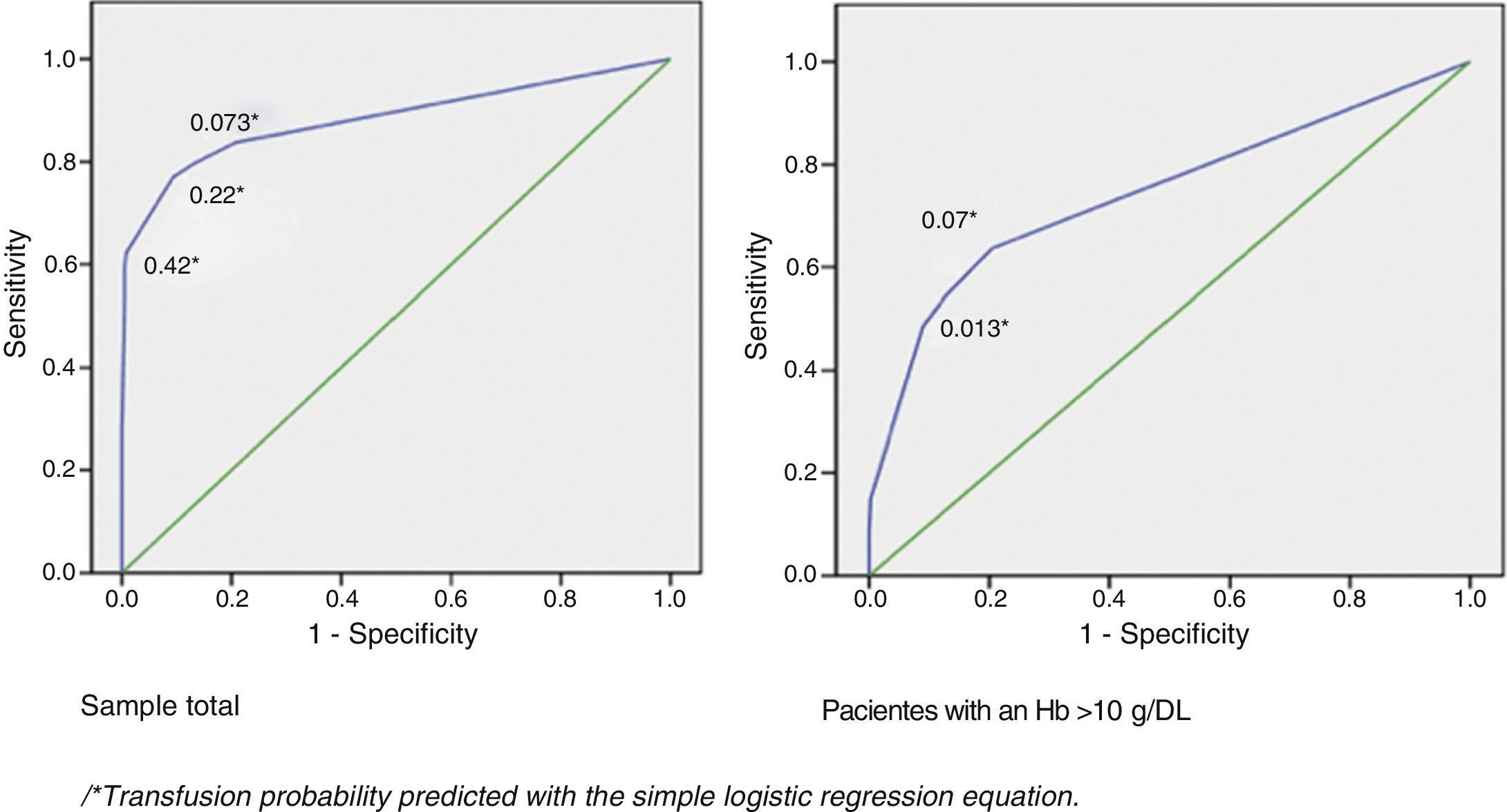
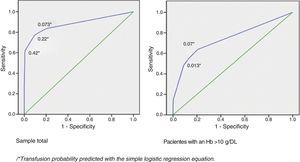
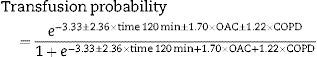
The results of multiple logistic regression analysis are shown in Table 3, the significant variables were: Hb levels<10g/dl, a history of COPD, receiving OAC treatment and surgery of a duration exceeding 120min. The prediction equation of the probability of receiving a transfusion from the values of these factors is included in the table. Fig. 2 presents the ROC sensitivity curve for predicted probability. Therefore the cut-off point with the best overall value is predicted probability of 0.2, which presents 77% sensitivity and 90.6% specificity. The area under the curve was 0.88 (95% CI: 0.83–0.94; P<.0001).
Multiple Logistic Regression Analysis.
| Variable | Parameters | OR | 95% CI |
| COPD | Yes/no | 3.7 | 1.3–10.7 |
| OAC | Yes/no | 5.7 | 1.7–19.5 |
| Surgery time | <120/>120min | 10.7 | 4.8–24.1 |
| Preoperative Hb | <10/>10g/dl | 309.8 | 52.7–985.2 |
Transfusion probability=e−3.36±5.7×preop Hb 10±2.38× time 120 min±1.75×OAC±1.29×COPD1+e−3.36+5.7×preop Hb 10+2.38×time 120 min+1.75×OAC+1.29×COPD.
OAC, oral anticoagulants; COPD, chronic obstructive pulmonary disease; Hb, haemoglobin; CI, confidence interval; OR, odds ratio.
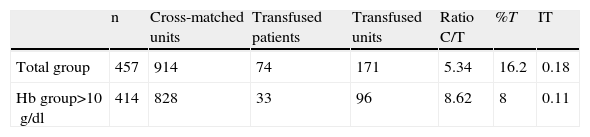
A subanalysis was made to evaluate which factors were associated with transfusion in patients with a HB above 10g/dl. In this group of 414 patients, only a total of 33 (8%) patients were transfused with a total of 96 units, which represent 56.1% of the total units transfused in the general group.
The transfusion rates calculated in this group of patients with preoperative Hb above 10g/dl were: C:T ratio=8.62; %T=8% and Ti=0.11.
The transfusion rates of the two groups of patients, total group and group with preoperative Hb>10g/dl, are shown in Table 4.
Transfusion Rates; Group Ratio.
| n | Cross-matched units | Transfused patients | Transfused units | Ratio C/T | %T | IT | |
| Total group | 457 | 914 | 74 | 171 | 5.34 | 16.2 | 0.18 |
| Hb group>10g/dl | 414 | 828 | 33 | 96 | 8.62 | 8 | 0.11 |
Tr, transfusion rate: recommended value≥0.5; C:T ratio, ratio cross-matched units to transfused units: recommended value≤2.5; %T, transfusion probability: recommended value>50%.
The variables significantly associated with having received a transfusion in this subgroup were: having heart disease (15.5% compared to 6.7%; P=.033); receiving oral anticoagulant therapy (25% compared to 7.2%; P=.015); and a surgery time exceeding 120min (32% compared to 4.3%; P<.0001). A history of COPD shows an association close to statistical significance (16.7% compared to 7.1%; P=.055). The results of multiple logistic regression analysis show that the independent variables significantly associated with having received a transfusion are: duration of surgery exceeding 120min (OR=11.3; 95% CI: 4.7–25.8), having a history of COPD (OR: 3.9; 95% CI: 1.3–12.3) and receiving treatment with OAC (OR: 6.3; 95% CI: 1.9–18.0). Fig. 2 shows the ROC sensitivity curve for predicted probability according to the equation obtained:
Thus, the cut-off point of best overall value has a predicted probability of 0.13, presenting 55% sensitivity and 87.1% specificity. The area under the curve was 0.74 (95% CI: 0.64–0.85; P<.0001).
DiscussionRequesting preoperative cross-matched blood is routine practice in elective surgery, even for surgical procedures with minimal perioperative blood %T.1,2,11,13,14 This preparation of cross-matched packed red blood cells goes beyond real needs. The first data published in this regard are the work of Friedman in 1973.15 In this study the ratio of cross-matched blood to transfused blood (C:T ratio), %T and Ti were used as indicators to demonstrate that requesting cross-matched blood preoperatively was unnecessary.
Kozarzewska et al.2 state that the values which justify ordering cross-matched blood preoperatively are a C:T ratio≤3, a %T≥30% and Ti≥0.5. However, their results were a C:T ratio=9, a %T=10.9 and a Ti=0.27, very far from real needs.
Other studies have been published in recent years which attempt to provide information on the disparity which exists between preoperatively cross-matched blood units and those which are eventually transfused for each surgical procedure. This routine preparation imposes a real burden on blood banks, both in terms of time and financial resources.4,11,13,16–18
Singh and Singh17 encountered a %T=14% in patients scheduled for colorectal surgery, with a C:T ratio=3.7 and a Ti=0.26. Similar data were obtained by Palmer et al.,18 finding a transfusion percentage of 16%.
The observational retrospective study we present all the identified 457 consecutive patients who underwent elective colonic surgery, two units of cross-matched blood having been routinely requested for each preoperatively (914 units in total), of which only 171 units were transfused in 74 patients (16.2%). This study attempts to identify the factors associated with perioperative blood transfusion which justify preoperatively requesting and preparing cross-matched packed red blood cells.
Rather than making an analysis by diagnosis or surgical procedure, the diagnoses were divided into two groups, benign disease and malignant disease (83% adenocarcinoma), and surgical procedures into resection and anastomosis techniques and other surgery. Similarly, the only preoperative analytical datum in the study were the plasma Hb count, but classifying the patients as to whether the count was higher or lower than 10g/dl, rather than using mean values for each group as in other studies.11 In this way the results were simplified.
In this regard, the preoperative Hb variable was the factor with the greatest strength of association with the probability of having received a transfusion (OR: 309.8; 95% CI: 52.7–985.2), as 95.3% of patients with an Hb lower than 10g/dl were transfused compared to 8% of patients with an Hb above 10g/dl. Since practically all of the patients with an Hb lower than 10g/dl received a transfusion, this in itself would be an indication for reserving blood, as long as it was not possible to resolve this prior to surgery by the appropriate treatment of the patient. Other factors independently associated with receiving a transfusion were a surgery time exceeding 120min, a history of COPD and receiving OAC therapy. The probability predicted by the equation has significant predictive capacity.
We decided to study the subgroup of patients with an Hb above 10g/dl to look for predictive factors for transfusion in these patients, which are the same as we found in the total sample: surgery time exceeding 120min, a history of COPD and receiving OAC therapy.
The need to evaluate predisposing factors for a blood transfusion in patients recommended for elective surgery was initially published by Ayantunde et al.11 in patients who were candidates for oesophagectomy due to cancer. The study concluded that the predictive factors for a blood transfusion are age and the presence of comorbidities. Other predictive factors were low preoperative Hb counts, being female and type of surgery.1,19,20
There is some work which attempts to formulate guidelines in which the ratio between requesting cross-matched blood preoperatively and the blood eventually transfused (C:T ratio) should not exceed 2.11,21 Indicators such as the Maximum Surgical Blood Ordering Schedule (MSBOS) and its subsequent amendment, and Mead's criteria22–24 attempt to predict the preoperative risk of blood transfusion for each surgical procedure.1,11,18
There are two objectives: not to overexploit the system's resources and to minimise the risks of transfusion.25 Due to the immunomodulation induced by blood transfusion, there is a greater risk of postoperative infection, deep vein thrombosis, and a higher rate of anastomotic dehiscence and neoplasic recurrence in oncological patients.26–30
The authors are exposing the habit of excessive preoperative ordering of cross-matched blood beyond real needs, which places a burden on the health system. It is essential to rationalise cross-matched blood ordering and establish the number of blood units which should be ordered for each surgical procedure.2,18
ConclusionsRoutine preoperative ordering of cross-matched blood is not justified in elective colon surgery and is an inefficient use of health resources. Predictive factors for transfusion must be identified for selective ordering of cross-matched blood in line with these factors. In our case, the abovementioned high risk factors for transfusion are a history of COPD, treatment with OAC and a predictable duration of surgery exceeding 120min. Patients with a preoperative plasma Hb count lower than 10g/dl should not undergo elective colon surgery unless their anaemia has been treated to increase their Hb count.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Feliu F, Rueda JC, Ramiro L, Olona M, Escuder J, Gris F, et al. Solicitud de sangre preoperatoria en cirugía programada de colon: ¿necesidad o rutina? Cir Esp. 2014;92:44–51.