In oncological patients who present solid hepatic lesions, it is necessary to rule out liver metastases of their primary neoplasm. A small number of these patients may have developed other very uncommon tumours, and reaching a correct preoperative differential diagnosis becomes very complex. We present the case of a patient with multiple nodular regenerative hyperplasias (NRH) of the liver associated with oxaliplatin.1–5 We also discuss the secondary hepatic effects of oxaliplatin and the clinical management of these patients.
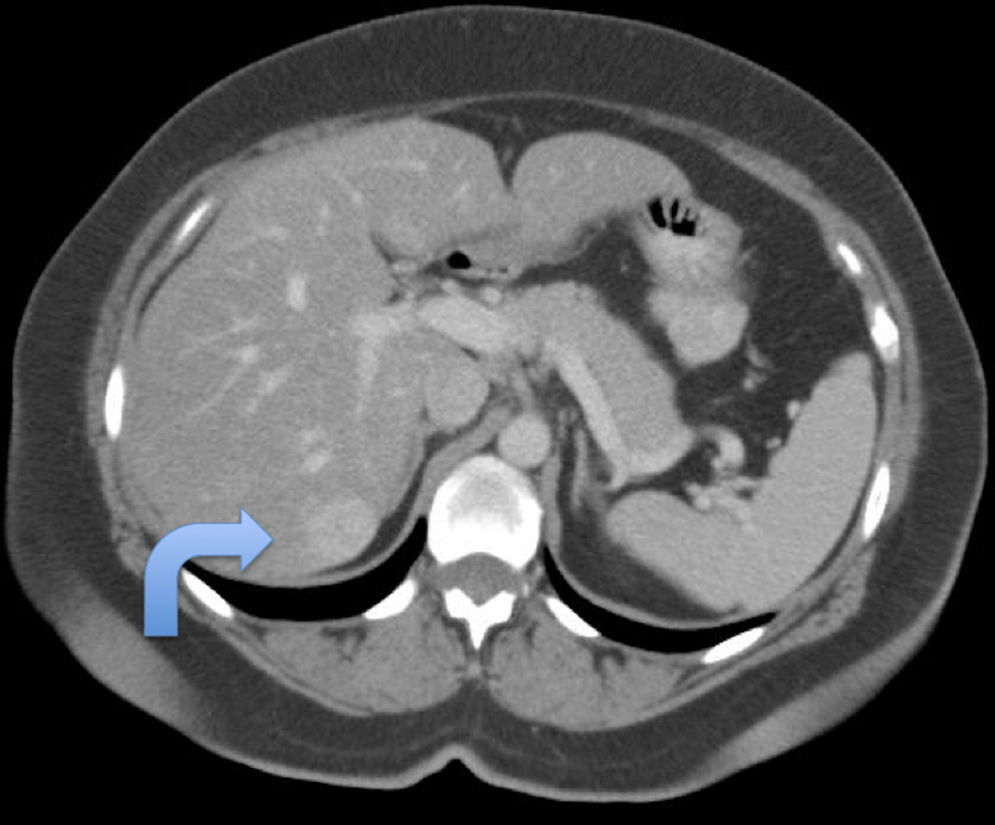
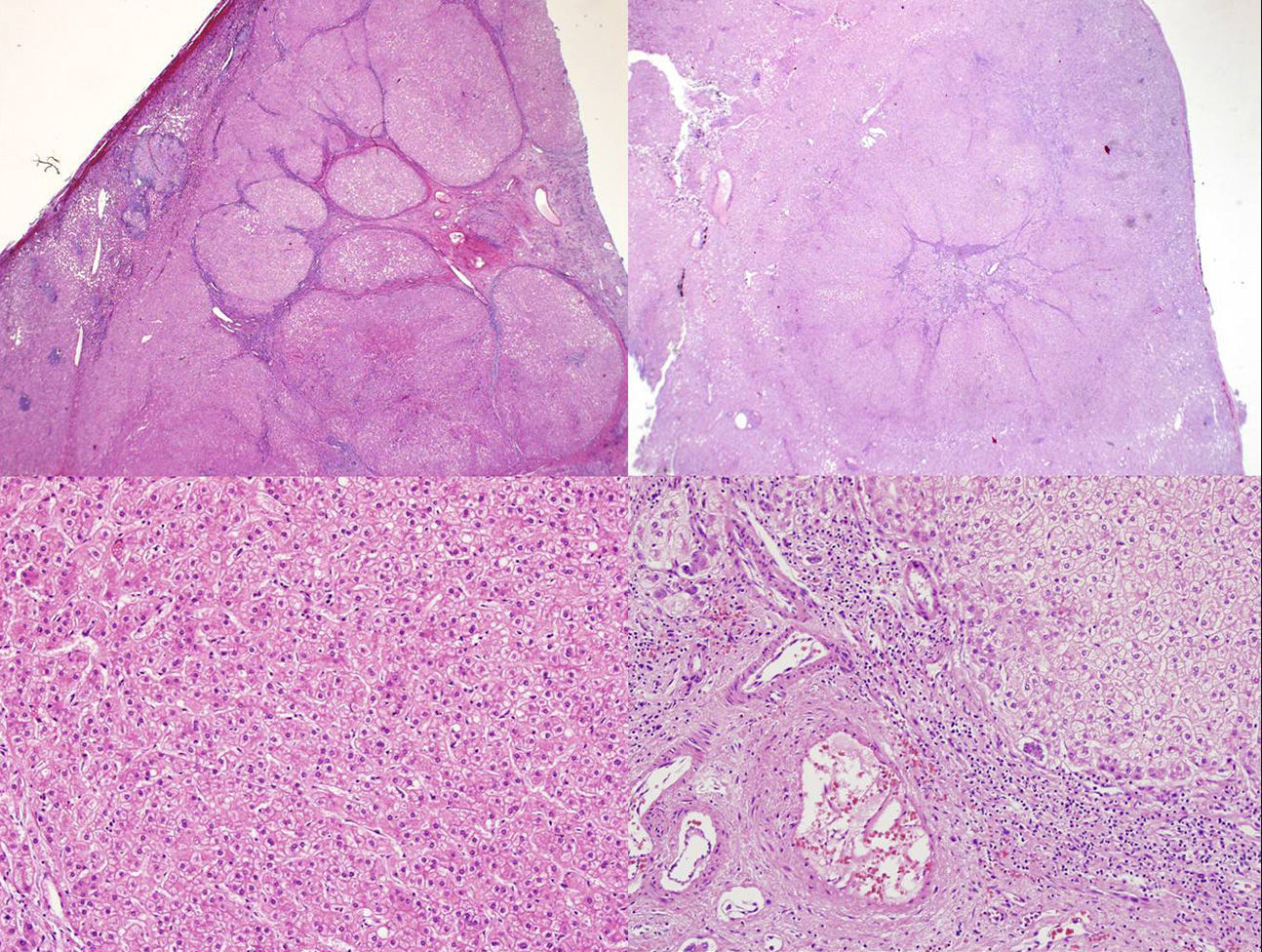
The patient is a 49-year-old woman with a history of left laparoscopic hemicolectomy in 2010 due to a 3cm well-differentiated adenocarcinoma of the colon, pT3N0M0, with perineural invasion. She was treated with XELOX (oxaliplatin 130mg day 1 and Xeloda® 1000mg/m2/12h for 14 days, every 21 days) for 6 months. Other conditions in her medical history included: ovarian cysts, obesity (BMI: 36), non-insulin-dependent diabetes mellitus, dyslipidaemia and multinodular goitre; Premm Model 1.2; hereditary nonpolyposis cancer risk 7%; negative phenotype for instability microsatellite (positive MLH1, MSH2, MSH and PMS2). Thirty months after surgery, a CT scan detected hepatic steatosis, a new focal hypervascular lesion measuring 30mm×20mm between segments VI and VII, another 8.5mm lesion in segment IVshowing enhancement in portal phase l, and mild mesenteric fat stranding compatible with mesenteric panniculitis, but no signs of portal hypertension (Fig. 1). Haemogram, hepatic biochemistry and tumour markers (CEA and CA19-9) were normal. PET demonstrated the liver lesions with no uptake; the area of panniculitis had an SUV of 3.2. Given these inconclusive findings, we decided to perform exploratory laparotomy. We observed the lesion in segment VII and 2 lesions measuring 2–3mm in segments II and III. Intraoperative ultrasound detected 5 other intraparenchymal lesions measuring 3–8mm, one of which was the observed lesion in segment IV during the CT scan. The ultrasound appearance of the lesions was not conclusive. We decided to resect the 2 accessible peripheral lesions in segments II and III as well as atypical resection of segment VII.The patient was discharged on the 3rd day post-op. The histological study showed that the 3 lesions were comprised of non-encapsulated liver tissue with a central scar, from which fibrous tracts emerged towards the periphery, and very dilated vascular structures compatible with NRH (Fig. 2). The patient no longer received oxaliplatin, and no nodules were detected in the liver in the radiological follow-up after 12 months.
Focal nodular hyperplasia (FNH) is the second most common solid benign hepatic tumour.6–8 FNH are usually small, peripheral, and asymptomatic; 10% are multifocal.6–8 Correct preoperative diagnosis is not always feasible.7,8 There is one published case of positive PET in FNH.9
NRH, also known as focal nodular hyperplasia regenerative lesions, are lesions that have a variable size that ranges from 1mm to 5cm; they can form nodules that are radiologically visible.2 The most widely accepted aetiology for NRH is variation of the liver flow with altered arterial/portal flow balance and increased hepatic arterial flow. They are observed in several situations: chronic Budd–Chiari syndrome, transplanted patients, arterial or venous thrombosis, after portacaval shunting, systemic diseases (Felty syndrome, amyloidosis, rheumatoid arthritis, etc.), or treatment with certain medications.2,10 Histologically, it is a proliferative process in which the regenerative nodules substitute the normal liver architecture without fibrosis.2,10 The hyperplastic hepatocytes compress the surrounding parenchyma, which show congestion and sinusoidal dilatation.10 Clinically, they can be asymptomatic or run their course with symptomatic portal hypertension.2,3,10
Different types of chemotherapy can cause induced non-tumour liver lesions or specific hepatic toxicity.3,5,6 The spectrum of lesions that occur in the liver parenchyma caused by oxaliplatin are complex and heterogeneous, caused by the changes in intrahepatic flow due to the portal damage at the sinusoidal level, finally resulting in sinusoidal obstructive syndrome.1,10 NRH is the highest degree lesion caused by oxaliplatin and it occurs in 15% of patients who receive this treatment.1,4,6,10 The existence of different sizes of NRH can reflect several types of vascular flow alterations.2 With NRH, the morbidity of liver resection and recurrence rates seem to increase, although no conclusive facts have been drawn in published series.1,3–5
The appearance of multiple NRH nodules induced by oxaliplatin visible on imaging tests is very uncommon as they are usually either very small or only visible histologically.1,6,10 Radiologically-observable NRH lesions are hypodense on CT without contrast material; with contrast, their enhancement is homogeneous in the arterial phase and slightly hyperdense in the portal phase.2 A central scar is sometimes observed. On MRI, NRH are hyperintense in T1 and isointense in T2.2 The few published cases of NRH share a series of characteristics: multiple lesions, no previous chronic liver disease, and normally negative PET and tumour markers.6,10 The existence of a negative PET, although important, cannot be considered key because the efficacy of PET decreases in a high percentage of patients treated with chemotherapy.6 Spontaneous regression of the lesions has been described after oxaliplatin use is discontinued, and there are reports of a certain protective effect of bevacizumab.6
In conclusion, the appearance of new liver lesions in oncology patients treated with oxaliplatin that do not present typical radiological characteristics, should make us consider the possibility of NRH caused by oxaliplatin.
Please cite this article as: Ramia JM, de la Plaza R, Perna C, Adel F, Kuhnhardt A. Hiperplasia nodular regenerativa hepática múltiple asociada a oxaliplatino. Cir Esp. 2016;94:52–54.