When primary abdominal wall closure has not been possible or after open abdominal decompression, the definitive abdominal wall closure can pose surgical problems that are difficult to resolve. Full-thickness abdominal wall defects caused by musculoaponeurotic and skin retraction, whose dimensions impede primary closure after a few days of maintaining an open abdomen open, make it necessary to search for different reconstructive strategies.1–3
We present the case of 3 patients with large full-thickness abdominal wall defects secondary to open abdominal decompression due to abdominal compartment syndrome (ACS). Definitive closure involved omentoplasty in order to isolate the abdominal viscera, reinforced with polypropylene (PP) mesh anchored on the oblique muscles retracted to the supra-aponeurotic position. In some cases, treatment included a partial skin graft.
Patient 1The patient is a 79-year-old male with a history of obesity and cholangitis who underwent laparoscopic cholecystectomy for cholelithiasis. He presented diffuse peritonitis secondary to a bile leak 48h later. Laparotomy was indicated; the cystic duct was sutured and peritoneal lavage performed. During the postoperative period in the intensive care unit (ICU), the patient developed ACS that was refractory to medical treatment, at which time open abdominal decompression was necessary. Afterwards, the patient showed progressive clinical improvement.
On the sixth postoperative day, abdominal wall reconstruction was performed. The full-thickness defect measured 20cm transversal (t) and 15cm longitudinal (l). A portion of the greater omentum was sutured to the musculoaponeurotic edge, which was reinforced with polypropylene mesh anchored on the retracted aponeurosis. During post-op, the patient required abdominal vacuum therapy for 5 weeks, and progressive mesh integration as well as wound granulation were obtained. Definitive reconstruction of the defect with a partial skin graft was suggested, but the patient preferred secondary intention with epithelialization, which was completed in 6 months. After 5 years of follow-up, he has presented no further complications.
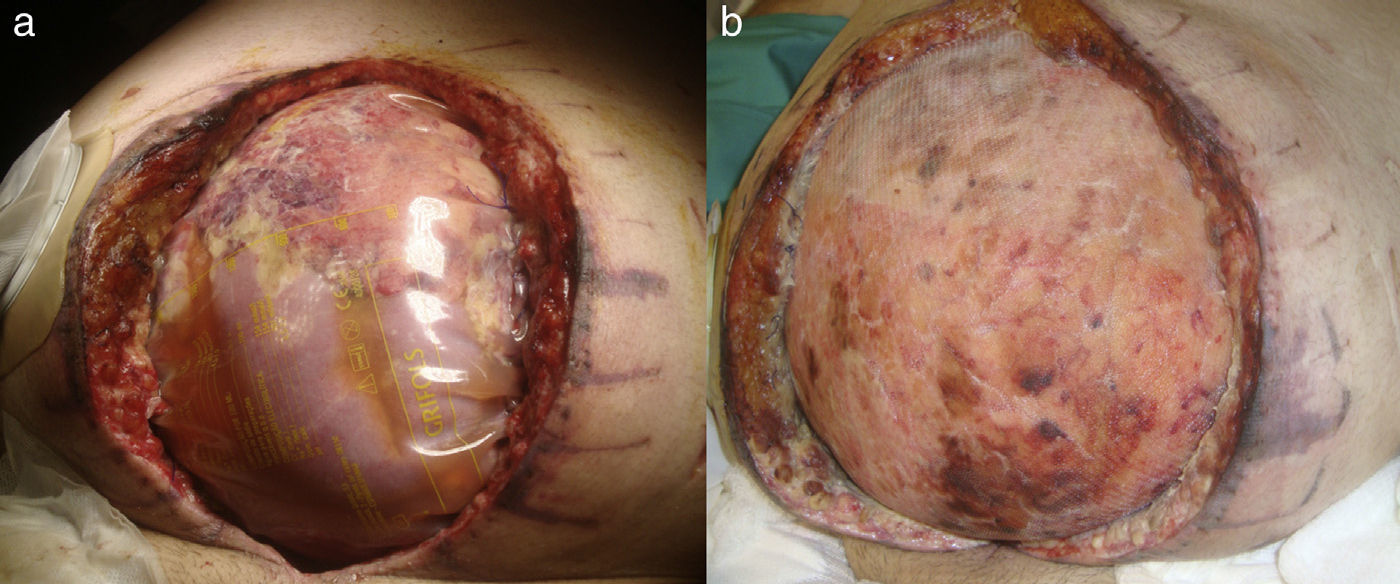
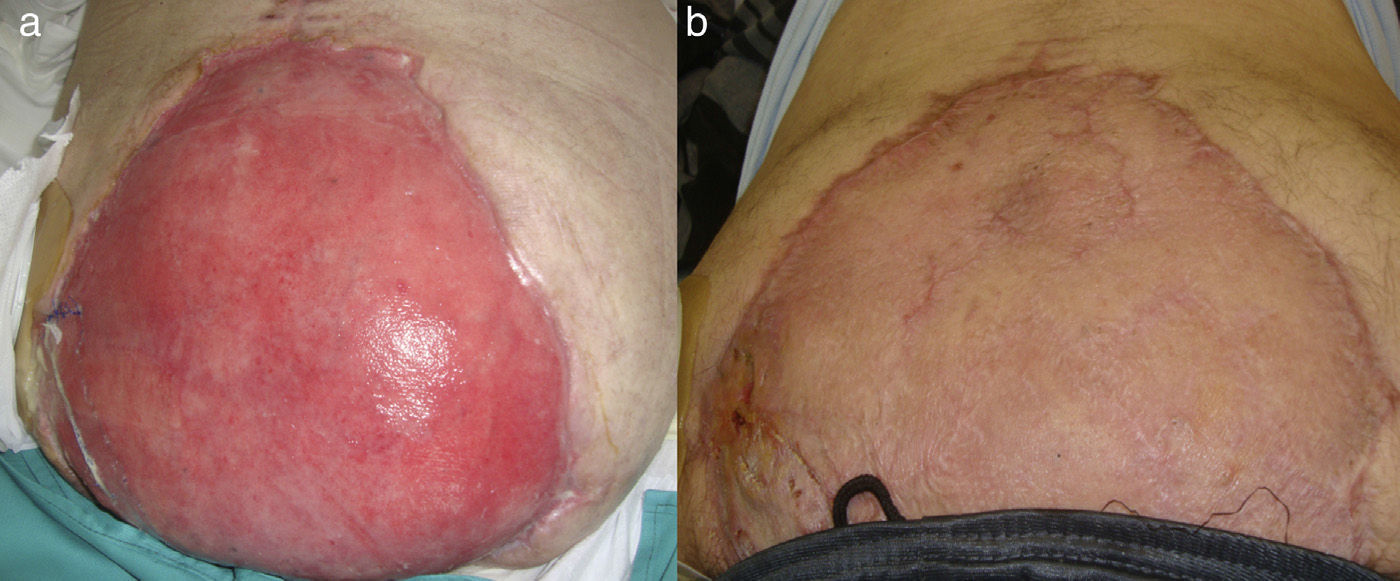
Patient 2The patient is a 67-year-old male with a history of morbid obesity, chronic obstructive pulmonary disease (COPD) and obstructive sleep apnea syndrome. During the postoperative period after radical cystoprostatectomy, he presented prolonged paralytic ileus with abdominal distension and evisceration. The patient was treated with primary closure, after which he developed ACS that required open abdominal decompression (Fig. 1A). After hemodynamic and ventilatory recovery, the abdominal wall defect measuring 32 (t)×22cm (l) was closed using an omentoplasty that was reinforced with supra-aponeurotic polypropylene mesh (Fig. 1B). During post-op, vacuum therapy was initiated, which achieved mesh integration and wound granulation (Fig. 2A) after 6 weeks of treatment. Afterwards, a partial skin graft over the skin defect achieved epithelialization in 40 days (Fig. 2B). The patient has not presented any complications after 10 months of follow-up.
The patient is a 68-year-old male with a history of obesity, heart failure and chronic bronchitis, who was hospitalized due to intestinal obstruction secondary to bezoar impaction that required segmental intestinal resections with primary anastomosis. In the postoperative period, he presented respiratory failure requiring ventilatory support and corticosteroid treatment. Reoperation was necessary due to anastomotic dehiscence with diffuse peritonitis and evisceration; intra-abdominal hypertension syndrome was observed, which required the abdomen to be left open. Six days later, he was reoperated for abdominal closure of a complete abdominal wall defect measuring 22 (t)×15cm (l), which was reconstructed with omentoplasty and reinforced with polypropylene mesh as in the two previous cases. The patient's progress was satisfactory, and vacuum therapy was applied for 3 weeks. The patient is currently in the waiting list for a partial skin graft over the granulation tissue.
In our setting, the use of biomaterials for the repair of abdominal wall defects began at the end of the 1980s. Clinical experience shows evidence that polypropylene mesh has good tolerance to infection4 as well as to the formation of intestinal fistulas, whose incidence was significantly reduced when the omentum was interposed between the mesh and intestine.5
The greater omentum has well-known immunologic and angiogenic properties,6,7 and it is been shown to be useful for the repair of large abdominal defects.8 However, there are few references about its capacity for granulation through PP mesh exposed to the exterior. Sandwich techniques have been described (from the inside out: absorbable mesh, polypropylene mesh and omentum), with good results.9 The isolating property of the omentum prevents the creation of fistulas, and it has shown satisfactory results in abdominal wall closure thanks to its capacity to integrate the PP, even in infected areas.10
Due to the dimensions of the wall defects, the PP mesh was left exposed, although this was not a problem for its integration and granulation. This may have been favored by the use of vacuum therapy.
Even though only one of the cases has a long follow-up (5 years), our limited experience leads us to conclude that the treatment of large full-thickness abdominal wall defects using this technique is a procedure to be considered in situations similar to those we have presented.
FundingThe authors declare that they have received no funding for the preparation of this manuscript, and it has not been presented at congresses or other publications.
Conflict of InterestsThe authors declare that they have no conflict of interests.
Please cite this article as: Muñoz Muñoz E, Pardo Aranda F, Camps Lasa J, Rodriguez Alsina X, Veloso Veloso E. Cierre de grandes defectos de pared abdominal mediante plastia de epiplón y malla de polipropileno sustitutoria en pacientes con laparostomías descompresivas. Cir Esp. 2015;93:204–206.