The true short esophagus is an entity of controversy among surgeons. Studies have been published about its diagnosis and laparoscopic treatment, without existing to date, publication of the treatment with robotic approach. We present, as a case report, our experience in robotic surgery for hiatal hernia with true short esophagus treated with Collis gastroplasty and Toupet fundoplication. Robotic surgery on the true short esophagus can facilitate mediastinal dissection and allow a more accurate suture technique. Studies are needed to compare the long-term results of this surgical technique between the conventional laparoscopic approach and the robotic approach.
El verdadero esófago corto es una entidad que causa mucha controversia entre los cirujanos. Se han publicado estudios acerca de su diagnóstico y tratamiento laparoscópico, sin que a día de hoy existan publicaciones del tratamiento con abordaje robótico. Presentamos, en forma de caso clínico, nuestra experiencia en cirugía robótica de hernia de hiato con verdadero esófago corto tratada con gastroplastia de Collis y fundoplicatura de Toupet. La cirugía robótica en el verdadero esófago corto puede facilitar la disección mediastínica y permitir una técnica de sutura más precisa. Son necesarios estudios para comparar los resultados a largo plazo de esta técnica quirúrgica entre el abordaje laparoscópico convencional y el abordaje robótico.
The true short esophagus is an intraoperative diagnosis defined as an intraabdominal esophageal portion, without tension, less than 2–3cm between the gastroesophageal junction and the diaphragmatic hiatus after an extensive mediastinal dissection of 7–10cm.1–3
The incidence between 3% and 20% of true short esophagus have been described in patients undergoing antireflux surgery.1,4
Failure to perform a correct mediastinal dissection that allows evaluation of the real intraabdominal esophageal portion may entail an overdiagnosis of the true short esophagus. An insufficient dissection can also lead to an increase in the recurrence of hiatal hernia after surgical treatment, caused by migration of fundoplication to the mediastinum.1
The treatment of hiatal hernia associated to a true short esophagus is still a matter of controversy among surgeons.5–7 Although Bellevue et al.8 did not find, in a case-control study, efficacy differences between patients treated with Hill's esophagopexy combined with Nissen fundoplication and patients treated with Collis gastroplasty associated with an antireflux technique; most of the current publications support Collis gastroplasty associated with an antireflux technique (Nissen, Toupet...) as the treatment for symptomatic hiatal hernia.1–3,5,9
Currently, there are multiple publications on laparoscopic treatment of true short esophagus, but there are no publications on the robotic approach. Our team in Center Hospitaliere of Luxembourg, which has an extensive experience in the field of minimally invasive surgery, wants to provide a case of management and treatment of true short esophagus with a robotic approach of a classic technique. Robotic surgery allows accuracy and safety in this specific technique.
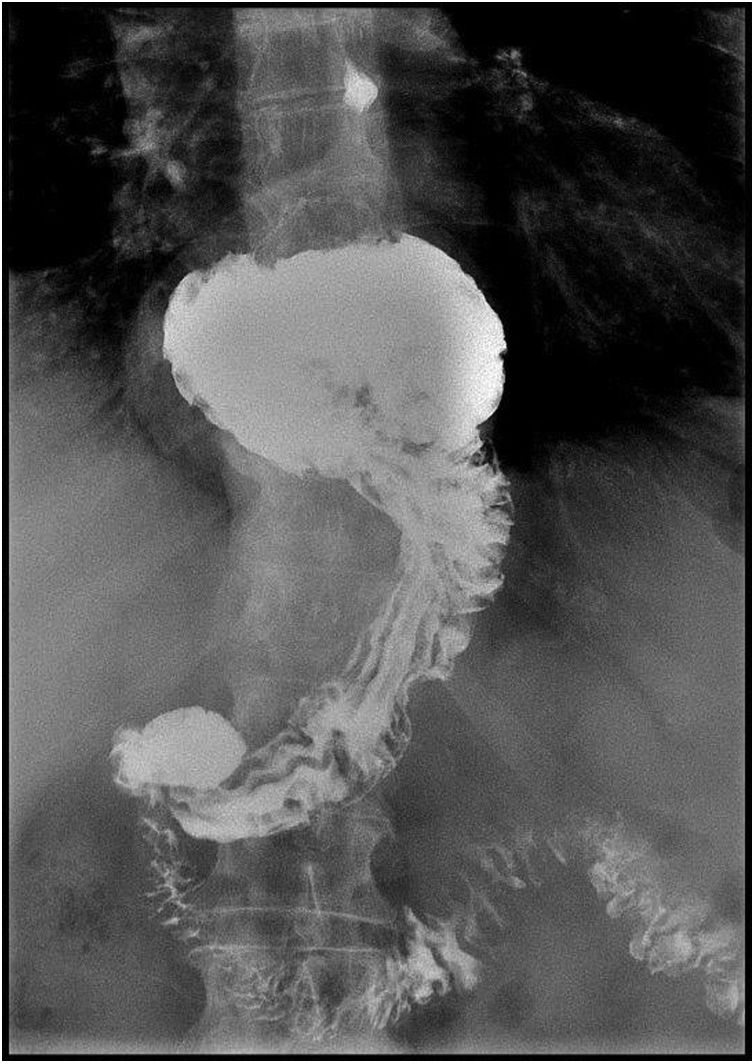
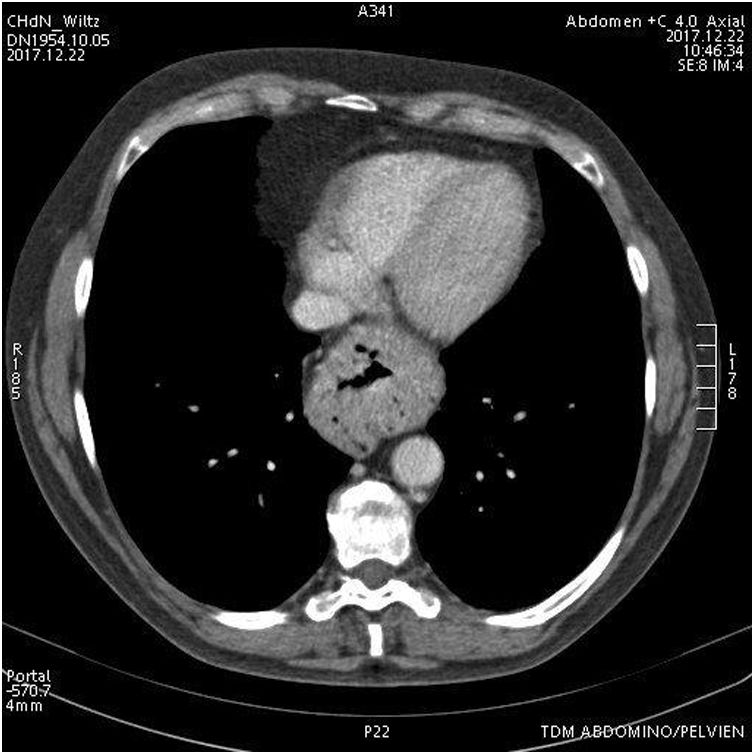
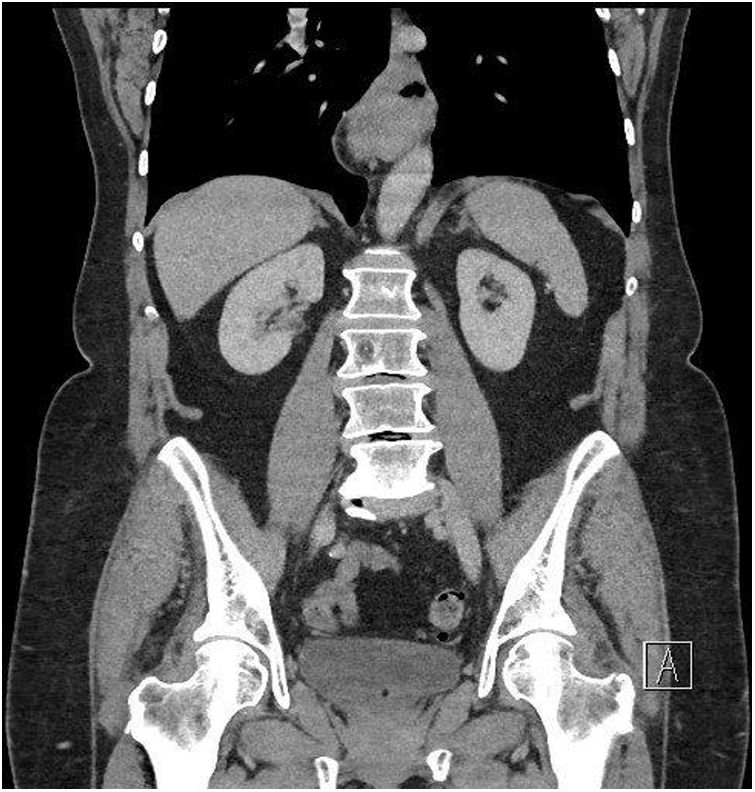
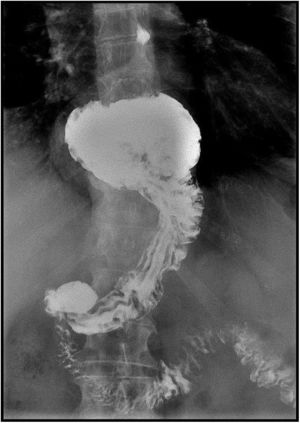
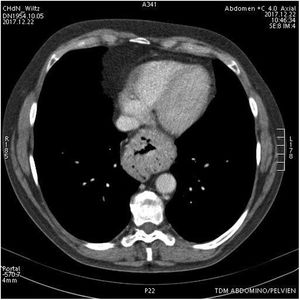
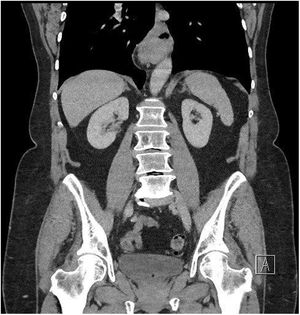
Case ReportWe present a 65 year old patient diagnosed with a symptomatic hiatal hernia of 2 years of evolution. Despite conservative treatment, postural and dietary recommendations, and the use of proton pump inhibitors (PPI), the patient presents worsening of gastroesophageal reflux symptoms. The radiological control shows a 4cm increase in the size of the hiatal hernia (from 2 to 6cm) (Figs. 1–3).
Endoscopy is performed, as a preoperative test, reporting an important gastritis and esophagitis but absence of Barrett's esophagus and neoplasia. With the diagnostic of symptomatic hiatal hernia as well as a suspected diagnostic of short esophagus surgical treatment is indicated.
With a robotic approach the reduction of the hiatal hernia and mediastinal dissection is performed and the diagnostic of true short esophagus is obtained. A Collis gastroplasty and a Toupet fundoplication are performed
In the absence of perioperative complications the patient is discharged 48h after the intervention, with complete oral tolerance and completely asymptomatic.
Surgical TechniqueAfter a year of experience in robotic surgery, with numerous interventions in bariatric surgery, colorectal surgery, pancreatic surgery, esophageal surgery and gastric surgery our team wants to add as a part of the learning curve a case of diaphragmatic hernia.
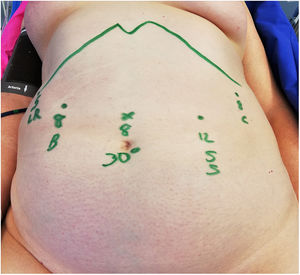
PlacementAfter the induction, the patient is placed in reverse Trendelenburg (30°), legs in abduction, and flexion (15°), as well as arms in complete adduction.
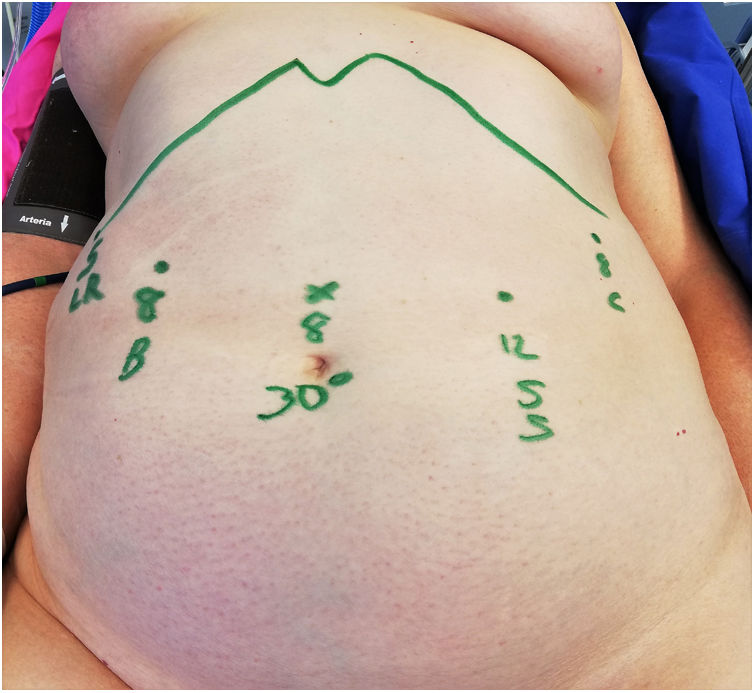
Five trocars are necessary, which are placed after the creation of a pneumoperitoneum with Veress needle, inserted in the upper left quadrant of the abdomen.
Following the scheme in Fig. 4, an 8mm trocar is placed for the 30° camera in the supraumblical midline (20cm from the xiphoid). From right to left of the patient and under direct vision; a 5mm trocar is placed at the level of the right subcostal anterior axillary line for the liver retractor that will remain fixed throughout the surgery, a 8mm trocar in the right middle clavicular line for the bipolar forceps, a 12mm trocar in the left clavicular middle line for the stapler and the scissors, and finally an 8mm trocar at the left anterior axillary line for the forceps.
The robot will be placed at the left of the patient.
DissectionThe fixed hepatic retractor allows us to see the diaphragmatic hiatus, without having to use one of the arms of the robot and without requiring laparoscopic assistance.
Dissection begins, using bipolar and scissors, at the right pillar of the esophageal hiatus, it is necessary to locate the vena cava and the branches of the vagus nerve. One of the arms of the robot, the 3rd or 4th, performs caudal traction of the stomach exposing the hernial sac. The dissection will follow an anterolateral direction until a complete exposure of His angle and gastric fundus is obtained. Carefully lysis of possible spleen adhesions is important in order to avoid bleeding that may interfere with the dissection. The 360° dissection is finished with the posterior part, being the most difficult one due to the difficulty of exposure, and the proximity of the aorta.
Once the entire esophageal circumference is dissected a loop is placed allowing uniform caudal traction. The dissection continues cranial 3–4cm, Type I dissection,1 toward the mediastinum. If a 2cm portion of tension-free intra-abdominal esophagus is not obtained, as in the case described, we continue dissecting the mediastinum up to 7–10cm, type II dissection. If, as in the case presented, despite this dissection, the tension-free intra-abdominal esophageal portion is still less than 2cm, a diagnostic of true short esophagus is achieved.
In some centers, intraoperative endoscopy is performed to determine the exact location of the gastroesophageal junction (Video 1: dissection).3,4,8,10
Plasty ManufactureIt is not possible to perform fundoplication without tension with short esophagus diagnostic, for this reason a Wedge-Collis gastroplasty1 is performed with Toupet fundoplication as an antireflux technique.11–14
A Wedge–Collis Gastroplasty as described for Terry et al.15 is performed. The liberation of the gastric fundus and the most cranial part of the greater curvature is performed with coagulation of the gastric short vessels. The diameter of the gastric plasty is determined with a 42 Fr orogastric tube. With a linear endo-stapler, introduced by the 12mm trocar, the stomach is sectioned. The section is performed from the greater curvature in a transverse direction an afterwards in a longitudinal direction taking into account the diameter of the orogastric tube, allowing an elongation of the esophagus of 3–4cm.
Once the gastroplasty is completed, the diaphragmatic pillars are approached from the posterior side creating a discrete angulation of the plasty, we use a nonabsorbable barbed suture (Video 2: plasty manufacture).
FundoplicationMaintaining the orogastric tube, a Toupet fundoplication is elaborated and fixed with non absorbable barbed suture. Finally, the closure of the defect is completed with the anterior approach of the pillars.
After reviewing the abdominal cavity, the surgical piece is removed, and the incisions are closed (Video 3: fundoplication).
DiscussionTaking into account that the diagnostic of the true short esophagus is intraoperative, the hiatal hernia should be treated by a team capable of modifying the surgical technique according to the findings seen during surgery.
In the case presented, the surgical technique was chosen according to the recommendations of the current literature,1–3,5,9 deciding to perform a Collis gastroplasty for esophageal lengthening because it is the technique that has less hiatus hernia recurrence and equal morbidity. Regarding to antireflux technique, there are no differences in efficacy between Nissen and Toupet fundoplication,11,14 but Toupet has less incidence of postoperative dysphagia.10–12
A primary approximation of the pillars without prosthetic material is chosen since there is currently no evidence that the prosthesis offers advantages involving risk of adhesions and dysphagia.10,16
At the time, we know that the conventional laparoscopic approach, compared to the laparotomy approach, offers the same incidence of recurrence of hiatal hernia with less morbidity and less hospital stay.17 Despite the rise of robotic surgery, there are no publications about robotic Collis gastroplasty. A meta-analysis done by Markar et al.18 composed by 5 randomized studies that compare Nissen fundoplication with laparoscopic technique and with robotic approach do not find differences in hospital stay, dysphagia or need for reoperation.
Our perception is that the robotic approach allows a more complete mediastinal dissection and a more precise suturing technique thanks to a better sense of depth offered by 3D vision, greater articulation of the robotic instruments and abolition of the tremor of the operator and the camera. Horgan et al.19 suggest, after analyzing 34 surgeries performed with Da Vinci (among which there is a Nissen and a Toupet fundoplication), that there is an improvement in accuracy and safety of the surgeon with the robotic approach obtained by better eye-hand coordination, 3D vision and abolition of tremor. Further studies are necessary to rule out possible differences in efficacy between the conventional laparoscopic approach and the robotic approach.
FundingWe declare no funding for this article.
Conflict of InterestWe declare that we have no conflict of interest.
We appreciate the help of the medical service for general and visceral surgery at the Luxembourg hospital as well as the great work done by the nursing team.
Please cite this article as: Vidal Piñeiro L, Pascotto B, Azagra Soria JS. Gastroplastia de Collis robótica. Cir Esp. 2020;98:288–291.