Sagliker syndrome (SS) was first described in 2004.1 This unique and uncommon entity occurs in patients with chronic kidney disease (CKD) in the course of inadequately treated secondary hyperparathyroidism (SHPT).2 The incidence of SS is estimated to be 0.5% of hemodialysis patients.1 SS is an exaggerated manifestation of renal osteodystrophy that combines advanced CKD, uncontrolled SHPT, and deformed facial features together with the appearance of brown tumors.3 After kidney transplantation, facial deformity is not reversible and this affects the quality of life of these patients.4–6
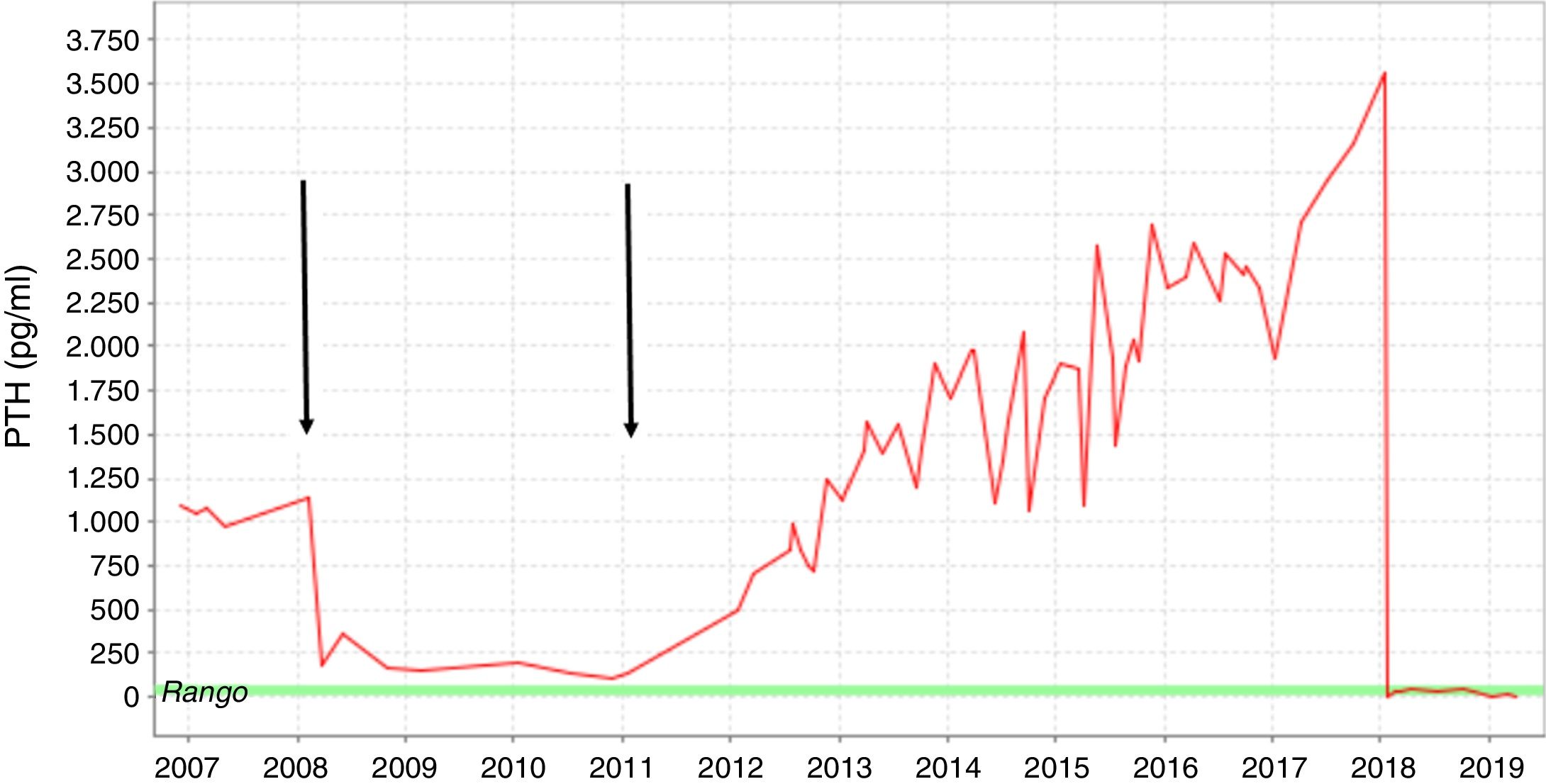
We present the case of a 35-year-old man with CKD secondary to glomerulosclerosis on dialysis for 9 years, who reported unusual changes in his facial features in recent years. Complete loss of residual renal function occurred in 2007. One year earlier, a progressive increase in parathyroid hormone (PTH) levels was detected. The patient received calcimimetics, phosphate binders and vitamin D; however, PTH levels continued to rise. In 2008, the patient received a cadaveric renal transplant. During this period, PTH values fell to near-normal levels. In 2010, a decrease in kidney graft function was observed due to poor adherence to immunosuppressive therapy. Initially, the patient refused to enter the hemodialysis program, although in 2012 he finally rejoined the program. At that time, PTH levels had risen to 1000 pg/mL (Fig. 1).
Fluctuation in PTH levels from 2007 to 2019. The arrows indicate kidney transplantation performed in 2008 and the acute renal graft rejection before reinitiating the hemodialysis program. Pharmacological preparations for SHPT (calcimimetics, phosphate binders and vitamin D) were used over the course of dialysis.
During the following 6 years, PTH levels continued to rise from 1000 to 3500 pg/mL despite intensive treatment including sevelamer (3200 mg/8 h), paricalcitol (9 µg/IV/3 times a week) and cinacalcet (90 mg/8 h).
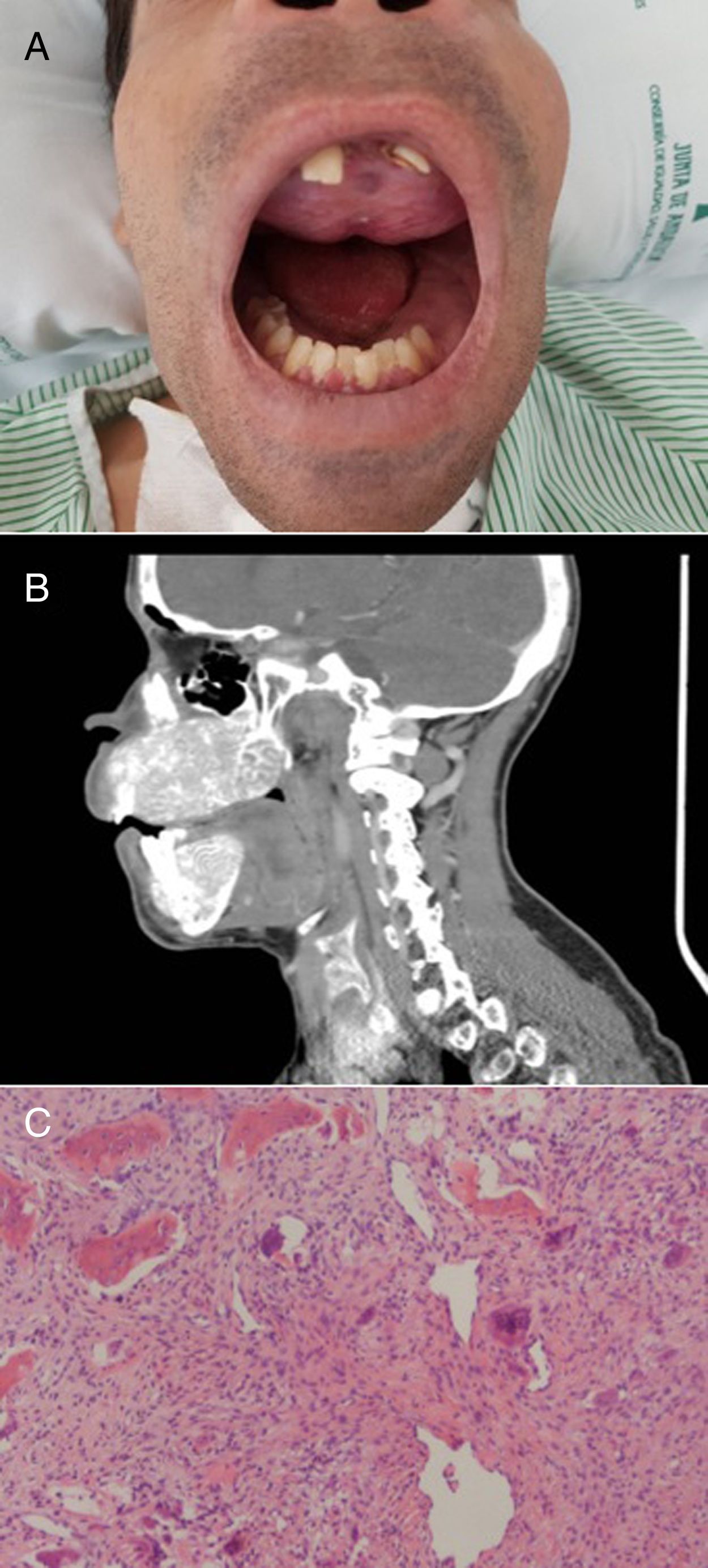
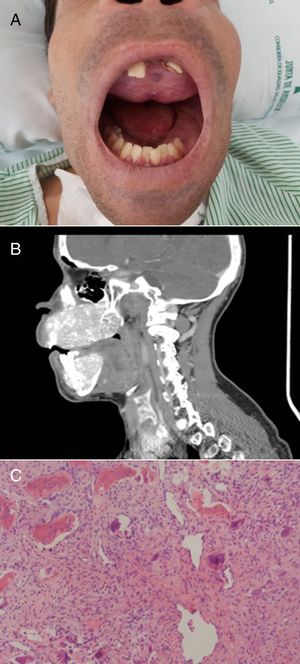
The patient reported headache, fatigue, joint pain and changes in the tips of the fingers. His face showed a notable frontal protrusion and obvious deformities of both the maxilla and the mandible. Both bones had expanded noticeably with a loss of normal architecture, causing the teeth to move into an irregular arrangement (Fig. 2A). Cranial computed tomography showed diffuse involvement of the cranial base and vault (Fig. 2B). Cervical ultrasound revealed 2 extrathyroid nodular lesions below the lower pole of the right thyroid lobe and the lower pole of the left thyroid lobe. On SPECT/CT scan, the only finding was pathological retention of the radiopharmaceutical over the lower end of the left thyroid lobe, suggestive of parathyroid adenoma.
A) Deformity of the maxilla and mandible. Brown tumor on the upper palate. B) CT scan of the skull showing diffuse bone disease characterized by obvious deformity of the upper and lower jaw, demineralization of the axial skeleton, and extensive lytic-appearing lesions. C) Mesenchymal and multinucleated giant cells, typical of brown tumor (H&E, ×50).
In 2017, after biopsy of the upper palate, the presence of a brown tumor was confirmed (Fig. 2C). The characteristic deformities of the face together with the appearance of a brown tumor confirmed the diagnosis of SS.
The patient underwent total parathyroidectomy with autotransplantation of a fragment of one of the glands and thymectomy. During the postoperative period, the patient presented hypocalcemia that was difficult to control, requiring calcitriol, oral calcium carbonate, and intravenous calcium gluconate for 5 days. After one year of follow-up, his calcium level remained stable and his PTH level was 14 pg/mL. The patient reported feeling subjectively better and a slight improvement in his facial features, although he was unable to close his mouth.
The mechanisms by which certain CKD patients develop SS are unknown. Some authors suggest that it may be due to a genetic alteration that is triggered during dialysis. An international study suggested that mutations in the GNAS1 gene could promote the genesis of SS.4 Evolved SHPT and inappropriate treatment may play an important role in the appearance of SS.3,4 In our patient, the lack of adherence to treatment that led to graft rejection and his refusal to undergo hemodialysis could have triggered the disease.
Facial changes in hyperparathyroidism are exclusively associated with patients who have advanced CKD, and their degree of association depends largely on the severity of the disease and its duration.1 Our patient developed deformities in his skull and jaw despite being exposed to maximum doses of cinacalcet. Cinacalcet is an extremely expensive drug, and, in patients whose parathyroid glands show nodular hyperplasia and a volume >500 mm3, it seems to be associated with resistance to treatment,3 as occurred with our patient.
According to the Kidney Disease Improving Global Outcomes (KDIGO) clinical guidelines, patients who present moderate deterioration of kidney function (G3a) to kidney failure (G5d), with significant secondary hyperparathyroidism that does not respond to medical treatment, should undergo parathyroidectomy.7 The postponement of parathyroidectomy for years clearly contributed to the appearance of the functional and cosmetic alterations of his face and hands, and to the presence of difficult to control hungry bone syndrome with a prolonged postoperative stay.
Therefore, in those patients with CKD and SHPT who are inadequately treated,2 parathyroidectomy should be performed without delay, before the onset or signs of SS.
Please cite this article as: Rubio-Manzanares Dorado M, Pino Díaz V, Fontillón Alberdi M, Padillo Ruíz J, Martos Martínez JM.Síndrome de Sagliker. Cir Esp. 2020;98:414–416.