Outpatient surgery is currently the standard procedure in 60%–70% of the most prevalent surgical procedures. Minimally invasive models in health care have improved basic aspects such as postoperative pain and hospital stay, but there are few publications related to perceived quality shown by patients, such as the need for informal care at home or delay before surgery. The aim of the study was to determine the global satisfaction perceived by patients undergoing abdominal wall hernia repair.
MethodsAn ad hoc split questionnaire has been completed on satisfaction after a week and postoperative quality a month after intervention by 203 patients operated on for abdominal hernia in a year. Variables included postoperative pain, need for informal care, surgical delay, information supplied, professional management and overall satisfaction.
ResultsA total of 48.28% of patients needed informal care at home. They were largely attended by women, wives or daughters, for a few days. In 45.81% they were discharged on the same day, and 53.2% in less than 72h. Overall satisfaction in the programme of day surgery and short hospital stay was 94.6%.
ConclusionsThe overall process of satisfaction was not related to age, sex or educational level of patients, while there was an inverse relationship between satisfaction and days of hospitalisation and days of pain that required analgesia at home.
La cirugía ambulatoria es el procedimiento estándar en el 60-70% de los procesos quirúrgicos más prevalentes. La cirugía poco invasiva ha mejorado aspectos fundamentales tales como el dolor postoperatorio y la estancia hospitalaria, pero hay pocas publicaciones relacionadas con aspectos de calidad y satisfacción de resultados percibidos por los pacientes, como la necesidad de cuidados informales a domicilio o la demora preoperatoria. El objetivo del estudio fue conocer la satisfacción global percibida por los pacientes intervenidos de hernia de pared abdominal.
MétodosUna muestra de 203 pacientes intervenidos de hernia en un año ha cumplimentado un cuestionario de satisfacción, una semana o un mes después de la intervención. Las variables incluyeron dolor postoperatorio, necesidad de cuidados informales, demora quirúrgica, adecuación de información recibida, trato dispensado y satisfacción global.
ResultadosEl 48,28% de los pacientes precisaron cuidados informales a domicilio, que fueron atendidos mayoritariamente por familiares durante pocos días. En un 45,81% se dio el alta el mismo día, y en el otro 53,2% antes de 72h. La satisfacción global en el programa de cirugía de día y corta estancia fue del 94,6%.
ConclusionesLa satisfacción global no estuvo relacionada con la edad, el sexo ni el nivel de estudios de los pacientes, pero existió una relación inversa entre el grado de satisfacción y los días de ingreso hospitalario y días de dolor que precisaron analgesia domiciliaria.
Day surgery has increased notably in recent decades, and it is now the usual procedure in 60%–70% of the most common surgical operations. The percentage of patients operated on in major outpatient and short stay (MO/SSS) surgical programmes currently allows a very high proportion of patients to recover from surgery at home. However, there is no precise information about the suitability of postoperative pain treatment or other factors in patient satisfaction and perceived quality over the medium term.1
The results of satisfaction studies have been published for MO/SSS programme patients, to evaluate the quality of care. The study by Carvajal2 stands out, as it evaluated the satisfaction of patients operated using laparoscopic cholecystectomy, covering aspects such as perceived waiting time, the coordination between the care services involved, the technical and human skills of healthcare personnel, the information given to patients during the process, pain control, well-being and the instructions given at discharge.
Repair of hernia of the abdominal wall is, after cataracts, one of the surgical procedures that are usually treated in MOS programmes. Given its clinical frequency and suitability for the inclusion criteria,3–12 it was selected as the objective of this study.
The main aim of this study is to discover the most important aspects for the perceived quality and degree of satisfaction with treatment in MO/SSS programmes among patients operated for primary hernia of the abdominal wall in the Cuenca healthcare catchment area.
MethodsThe study was designed to be observational and transversal.
A sample of 203 (50.75%) were included of the 400 patients operated for hernia from January 2009 to February 2010 in the healthcare catchment area of Cuenca, and who answered all of the questionnaire.2 The questionnaire used to evaluate satisfaction in the case of patients operated for cholecystectomy was adapted and used. We replaced the questions about hospitalisation with others about recovery at home for patients treated using hernioplasty in the MOS-CE programme. This study offers the new data regarding the evaluation by patients one month after their surgery, not only in terms of the quality of the care in the hospital itself, but also with respect to their perceived well-being during postoperative recovery at home.
The questionnaire was presented during the postoperative check-up visit. It includes a total of 23 multiple choice questions divided into 2 parts: one with 5 sociodemographic questions, 12 about satisfaction with use of the MOS unit and 6 other questions, followed by a final question about overall satisfaction with the process, including postoperative complications (Appendix A) (available online).
The data in clinical histories on complications following discharge and unplanned readmissions were also taken into account.
The questionnaire was presented as follows: the first part on the evaluation of the MOS unit was applied one week after the operation; and the second part, on postoperative experience in the home, was applied during the check-up 30 days after the operation, in a face-to-face interview. Patients were asked to fill out the questionnaire anonymously, and the purpose of the study was explained to them. Only those questionnaires that were fully completed were included.
The questionnaire used (Appendix A, annex 1) is based on other pre-existing ones that were published in other studies.2,13–15 It is currently awaiting validation. It was adapted to the type of surgical operation (hernioplasty) used in our cases, together with the type of patients in our sample, and it is suitable for their expectations and experiences. The most important items and the most relevant questions16,17 have been shown, as well as the data which interviewees thought important to express. It was applied divided into 2 parts: one after a week and the other one month after the operation,18 which was filled out after the postoperative check-up.
The main variable of the overall level of satisfaction was shown as a multiple choice question on a scale of 0–10 in which these extremes represented the least and highest levels of satisfaction, respectively. Each patient was offered the possibility of awarding a score to express their degree of satisfaction in whole values and decimals, and the results were grouped in a scale of whole values to facilitate statistical analysis. This main variable was compared with the variable presented (willingness to recommend the MOS unit).
Patient opinions for variables relating to their time in the Unit were evaluated (comfort during their stay and how they were treated by staff), together with those connected with their subjective postoperative experience in their home (informal care in the home, the need for analgesics) and their opinion of delay in surgery.
Inclusion criteria were that all cases had to be over the age of 16 years old, with a diagnosis of primary abdominal wall hernia, with elective surgery operated in the day surgery programme (ASA I and II risk patients, with local anaesthesia and sedation) or short hospital admission during 3 days or less (patients with a prior ASA III risk and regional or general anaesthesia). All emergency cases were excluded, together with those diagnosed with incisional hernia. Paediatric patients were also excluded, as well as those patients who did not answer at least a part of the satisfaction questionnaire.
The cases at the greatest previous risk (ASA III-IV) were operated under general anaesthetic. The others were assigned regional or local anaesthesia with sedation depending on their preferences.
Statistical analysis of the data was undertaken using version 19.0 of SPSS in Spanish, using frequency and proportion analysis as well as chi-square statistics for categorical variables and logistic regression studies in multivariable analysis. The relationships between binary variables were also evaluated using odds ratio (OR) association measures and prevalence ratios (PR).
Both parts of the questionnaire were subjected to reliability and validity analysis by evaluation of previous applicability (the KMO test and Bartlett's test of sphericity), reliability (Cronbach's alpha) and internal consistency (analysis of the main components).
ResultsThe 203 patients included in the study answered the second part of the questionnaire, and 85 answered the first part.
The reliability and validity of the satisfaction questionnaire (the first part) were analysed, with the following result; Cronbach's alpha 0.621 (CI: 0.491–0.730) while perceived quality (the second part) scored 0.326 (CI: 0.162–0.467) with an explained variance of 66.2% and 63.9%, respectively.
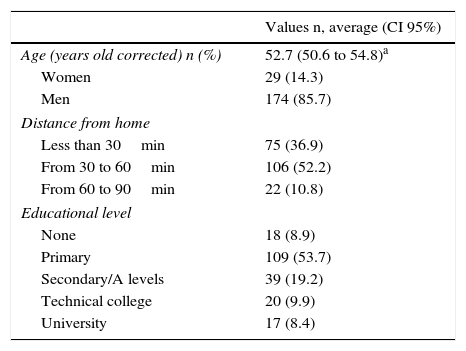
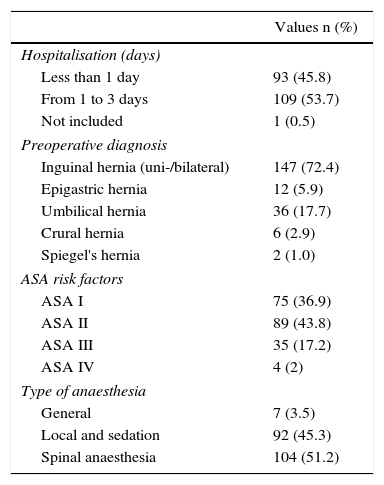
The results describing the demographic data are shown in Table 1, while the clinical data are given in Table 2. The complications that arose immediately after the operation were moderate, at around 13.8%. The most frequent one was transitory haematoma in the surgical wound, followed by temporary urinary retention. The other complications were, in order of frequency: pressure cephalalgia attributable to spinal puncture and general complications (disorientation, thoracic pain). Of all the cases operated on, 195 (96.1%) were primary hernias and 8 (3.9%) were recurrent hernias.
Sociodemographic Description and Hospitalisation.
| Values n, average (CI 95%) | |
|---|---|
| Age (years old corrected) n (%) | 52.7 (50.6 to 54.8)a |
| Women | 29 (14.3) |
| Men | 174 (85.7) |
| Distance from home | |
| Less than 30min | 75 (36.9) |
| From 30 to 60min | 106 (52.2) |
| From 60 to 90min | 22 (10.8) |
| Educational level | |
| None | 18 (8.9) |
| Primary | 109 (53.7) |
| Secondary/A levels | 39 (19.2) |
| Technical college | 20 (9.9) |
| University | 17 (8.4) |
Admission, Diagnosis, Risk Factors and Anaesthesia.
| Values n (%) | |
|---|---|
| Hospitalisation (days) | |
| Less than 1 day | 93 (45.8) |
| From 1 to 3 days | 109 (53.7) |
| Not included | 1 (0.5) |
| Preoperative diagnosis | |
| Inguinal hernia (uni-/bilateral) | 147 (72.4) |
| Epigastric hernia | 12 (5.9) |
| Umbilical hernia | 36 (17.7) |
| Crural hernia | 6 (2.9) |
| Spiegel's hernia | 2 (1.0) |
| ASA risk factors | |
| ASA I | 75 (36.9) |
| ASA II | 89 (43.8) |
| ASA III | 35 (17.2) |
| ASA IV | 4 (2) |
| Type of anaesthesia | |
| General | 7 (3.5) |
| Local and sedation | 92 (45.3) |
| Spinal anaesthesia | 104 (51.2) |
Surgical repair was by tension-free hernioplasty, using Lichtenstein's technique in the groin, a femoral plug and a surgical mesh in all other anatomical locations.
Regarding the time needed for care every day, in general patients required help every day during periods of one hour or less in 193 cases (95.1%) during a period shorter than 7 days. Of these, 105 patients (51.7% of the total) did not require home care of any kind in their everyday activity (except for work).
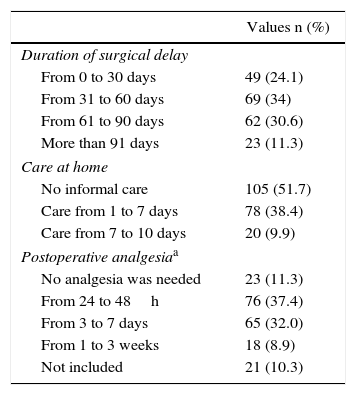
Table 3 shows the results of the home care, postoperative analgesia and surgical waiting time (number of cases and relative frequency). The individuals supplying care were women (wife, mother or sister) in the majority of cases (87; 88.77%). In the satisfaction questionnaire, 139 patients awarded an overall score of 9/10 points, 50 7/8 and 14 5/6. The average overall level of satisfaction was 8.94. Of all the interviewees, 192 (94.6%) would recommend the MO/SSS programme to a family member or acquaintance.
Delay in Surgery, Postoperative Care and Analgesia in the Home.
| Values n (%) | |
|---|---|
| Duration of surgical delay | |
| From 0 to 30 days | 49 (24.1) |
| From 31 to 60 days | 69 (34) |
| From 61 to 90 days | 62 (30.6) |
| More than 91 days | 23 (11.3) |
| Care at home | |
| No informal care | 105 (51.7) |
| Care from 1 to 7 days | 78 (38.4) |
| Care from 7 to 10 days | 20 (9.9) |
| Postoperative analgesiaa | |
| No analgesia was needed | 23 (11.3) |
| From 24 to 48h | 76 (37.4) |
| From 3 to 7 days | 65 (32.0) |
| From 1 to 3 weeks | 18 (8.9) |
| Not included | 21 (10.3) |
Data on the need for postoperative analgesia are shown in Table 4. In 21 cases it was not possible to determine data on the need for this.
Satisfaction With Treatment in the MOS Unit and Perceived Quality of Postoperative Care and Surgical Delay.
| Variable | Average score (from 5) | CI 95% | |
|---|---|---|---|
| Comfort in the MOS Unit | 3.65 | 3.48 | 3.82 |
| Family opinion of the MOS Unit | 3.53 | 3.36 | 3.70 |
| Suitability of the information about the process | 3.60 | 3.49 | 3.71 |
| Treatment by administrative staff | 3.60 | 3.43 | 3.77 |
| Treatment by nursing staff | 3.71 | 3.60 | 3.82 |
| Treatment by medical staff | 3.73 | 3.63 | 3.83 |
| Experience of the anaesthesia | 3.53 | 3.38 | 3.68 |
| Variable | Average | CI 95% | |
|---|---|---|---|
| Informal care at home (days) | 2.87 | 2.28 | 3.46 |
| Informal care at home (min./day) | 13.33 | 8.92 | 17.74 |
| The need for analgesia (days) | 3.58 | 2.99 | 4.17 |
| Delay in surgery (days) | 59.26 | 54.03 | 64.49 |
| Degree of overall satisfactiona | 8.94 | 8.76 | 9.12 |
With respect to the time spent in the surgical waiting list (SWL) prior to the operation for the MO/SSS programme, this varied from 5 to 252 days, with an average wait of 59.3 days. This is 6 days shorter than the average wait for planned standard surgery in the General Surgery Department on the same dates.
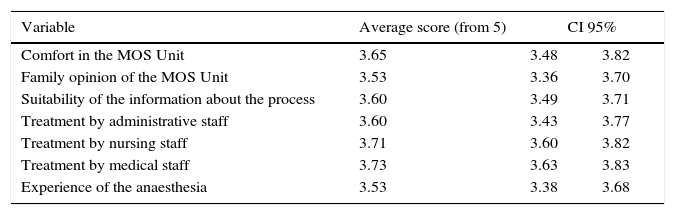
The evaluation by the patients of the questions in association with the variables which describe professional care, the information received and their impression of the infrastructure are shown in Table 5.
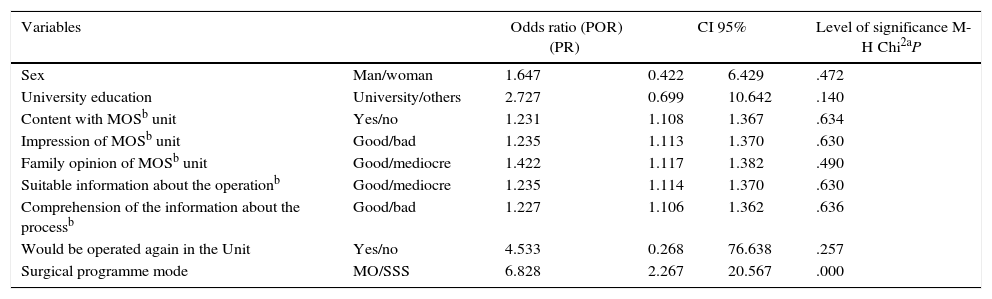
Level of Satisfaction (Stratified Analysis).
| Variables | Odds ratio (POR) (PR) | CI 95% | Level of significance M-H Chi2aP | ||
|---|---|---|---|---|---|
| Sex | Man/woman | 1.647 | 0.422 | 6.429 | .472 |
| University education | University/others | 2.727 | 0.699 | 10.642 | .140 |
| Content with MOSb unit | Yes/no | 1.231 | 1.108 | 1.367 | .634 |
| Impression of MOSb unit | Good/bad | 1.235 | 1.113 | 1.370 | .630 |
| Family opinion of MOSb unit | Good/mediocre | 1.422 | 1.117 | 1.382 | .490 |
| Suitable information about the operationb | Good/mediocre | 1.235 | 1.114 | 1.370 | .630 |
| Comprehension of the information about the processb | Good/bad | 1.227 | 1.106 | 1.362 | .636 |
| Would be operated again in the Unit | Yes/no | 4.533 | 0.268 | 76.638 | .257 |
| Surgical programme mode | MO/SSS | 6.828 | 2.267 | 20.567 | .000 |
PR: prevalence reason.
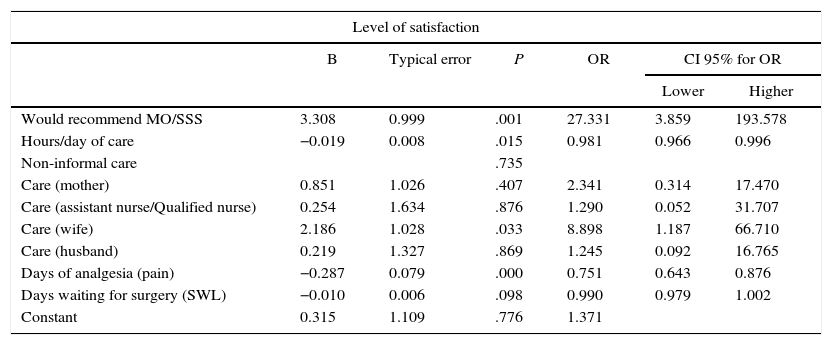
Table 6 shows the results of multivariable analysis between overall degree of satisfaction and a positive recommendation to use the MOS Unit, as well as the most important factors that influenced both variables.
Level of Satisfactiona (Multivariable Analysis).
| Level of satisfaction | ||||||
|---|---|---|---|---|---|---|
| B | Typical error | P | OR | CI 95% for OR | ||
| Lower | Higher | |||||
| Would recommend MO/SSS | 3.308 | 0.999 | .001 | 27.331 | 3.859 | 193.578 |
| Hours/day of care | −0.019 | 0.008 | .015 | 0.981 | 0.966 | 0.996 |
| Non-informal care | .735 | |||||
| Care (mother) | 0.851 | 1.026 | .407 | 2.341 | 0.314 | 17.470 |
| Care (assistant nurse/Qualified nurse) | 0.254 | 1.634 | .876 | 1.290 | 0.052 | 31.707 |
| Care (wife) | 2.186 | 1.028 | .033 | 8.898 | 1.187 | 66.710 |
| Care (husband) | 0.219 | 1.327 | .869 | 1.245 | 0.092 | 16.765 |
| Days of analgesia (pain) | −0.287 | 0.079 | .000 | 0.751 | 0.643 | 0.876 |
| Days waiting for surgery (SWL) | −0.010 | 0.006 | .098 | 0.990 | 0.979 | 1.002 |
| Constant | 0.315 | 1.109 | .776 | 1.371 | ||
Overall degree of satisfaction was not significantly related to age or sex, although it was with other variables (days of pain, SWL). With respect to the days of informal care at home and days admitted to hospital, this showed an inverse relationship between degree of satisfaction and the incidence of both. The degree of satisfaction recorded at the end of the process was significantly influenced above all by 2 variables: the number of days that it was necessary to take analgesics at home after the operation, because this has a major effect on reintegration into normal life (which determines postoperative well-being), and the time spent in the waiting list before surgery, which if prolonged may lead to disappointment regarding the expectation of a prompt and dynamic process. These data agree with those observed by other authors in the study of other populations.19–26
The patients expressed quite a high level of approval of the information, professional attention and anaesthesia they received, and they were generally satisfied with these aspects. Within the results, the high scores awarded for the work of the administrative, nursing and medical professionals involved stand out, as do those for the information received about the process, the comfort of the Unit where they prepared for and recovered from the operation, as well as their acceptance of future operations in the same programme. On the contrary, less favourable scores were awarded for their experience of the anaesthesia and, above all, for the opinion of their family of the Unit, the suitability of the process and the prevention of family disturbance.
50.75% of the total sample completed the questionnaire, indicating a high incidence of total or partial failure to answer the questions in the test. This may also be due to patient absence, if they did not attend the check-ups for which they had appointments. These results are in agreement with those of other authors on answering questionnaires a posteriori.16,27
Hospital admission was prolonged in 7 unplanned cases (3.8%), all of which were due to surgical causes (local complications with the wound) or anaesthesia (regional anaesthesia). This data agrees with published percentages caused by surgery or anaesthesia.28,29
One month after the operation, the majority of patients had regained their independence in everyday activities and work. 48.28% had required informal help at home, generally for less than a week and for an average of less than 60min per day. More than half of the patients had not needed help at home for their everyday activities. Nor did they need to take analgesics for very long: they had been supplied with medication for 48h, and 37.4% took analgesics during the first 2 days, as prescribed at discharge, while 18% required analgesia for 1–3 weeks. The level of satisfaction with the process as a whole was high in 86.2% of cases, and 94.6% would recommend inclusion in the future in the MOS programme.
The results of our study agree quite closely with those of publications that link degree of satisfaction with information and hospital care,17 although it also offers a different viewpoint that centres on estimations based on clinical management, in which patients evaluate the quality of care in connection with degree of accessibility (waiting for surgery) and the quality of care (days of admission, postoperative pain) and the efficiency of the system (acceptance of a MO/SSS programme).
The chief limitations of this study stem from its medium-sized sample and ad hoc questionnaire taken from previous studies and adapted for the surgical procedure of hernioplasty, but without previous validation. Due to this the results have to be evaluated in the light of their limitation, and subsequently compared with those of other future studies with larger samples. The questionnaire used has yet to be validated for abdominal wall hernia, so that it would be of interest to continue this line of research, given the level of interest which we believe subject arouses in medical staff and managers, as well as among those who are affected by this complaint.
Authors- 1.
Study concept and design. Data gathering. Data analysis and interpretation: Ricardo de Miguel Ibáñez.
- 2.
Study concept and design. Data analysis and interpretation: Francisco Escribano Sotos (Francisco.ESotos@uclm.es).
- 3.
Data gathering: Saif Adeen Naban al Saied, Javier Alonso Vallejo.
- 4.
Approval of the final version for publication: Ricardo de Miguel Ibáñez, Francisco Escribano Sotos, Saif Adeen Naban al Saied, Javier Alonso Vallejo.
The authors declare there are no conflicts of interests.
FinancingThis paper has not been published in other scientific journals and nor is it being evaluated at the present time by any scientific journal.
This paper was not supported by any grant or financial assistance.
We would like to thank Professor Francisco Escribano Sotos for his help with this work, as it would not have been possible without his tutelage.
Please cite this article as: de Miguel-Ibáñez R, Nahban-al Saied SA, Alonso-Vallejo J, Escribano Sotos F. Resultados de satisfacción y calidad de vida percibida en pacientes intervenidos de hernia primaria de pared abdominal. Cir Esp. 2015;93:658–664.