Superior mesenteric artery syndrome (SMAS) or Wilkie syndrome (WS) involves compression of the third part of the duodenum by the aortomesenteric angle, which can be caused by anatomical malformations or losses of perivascular adipose tissue after periods of hypercatabolism or malnutrition. Symptoms include postprandial pain, feeling of fullness, nausea with or without vomiting, and consequent weight loss. The initial treatment is conservative with hygienic-dietary measures and weight gain, although bypass surgery should be indicated in the event of failure.
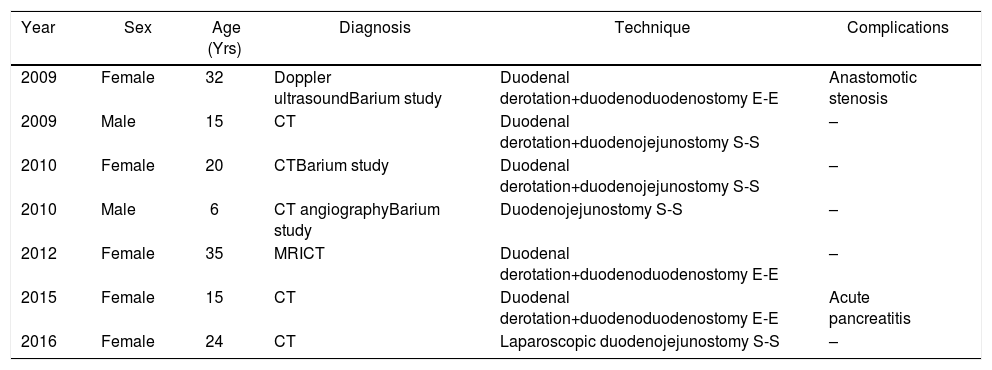
We present a series of patients with SMAS who were treated surgically (Table 1).
Patients Treated Surgically for SMAS.
| Year | Sex | Age (Yrs) | Diagnosis | Technique | Complications |
|---|---|---|---|---|---|
| 2009 | Female | 32 | Doppler ultrasoundBarium study | Duodenal derotation+duodenoduodenostomy E-E | Anastomotic stenosis |
| 2009 | Male | 15 | CT | Duodenal derotation+duodenojejunostomy S-S | – |
| 2010 | Female | 20 | CTBarium study | Duodenal derotation+duodenojejunostomy S-S | – |
| 2010 | Male | 6 | CT angiographyBarium study | Duodenojejunostomy S-S | – |
| 2012 | Female | 35 | MRICT | Duodenal derotation+duodenoduodenostomy E-E | – |
| 2015 | Female | 15 | CT | Duodenal derotation+duodenoduodenostomy E-E | Acute pancreatitis |
| 2016 | Female | 24 | CT | Laparoscopic duodenojejunostomy S-S | – |
ECO: ultrasound; MRI: magnetic resonance imaging; SMAS: superior mesenteric artery syndrome; CT: computed tomography.
Between 2009 and 2018, 7 patients were treated. In 5 (71.4%), duodenal derotation and anastomosis were performed (3 by duodenoduodenostomy and 2 by duodenojejunostomy), while duodenojejunostomy was performed in another 2 (28.5%) without derotation, and one of them laparoscopically.
All patients had a history of postprandial pain that improved after vomiting, as well as low body weight. The persistence of pain, difficult weight maintenance and risk of inadequate growth, despite dietary treatment, were indications for surgery.
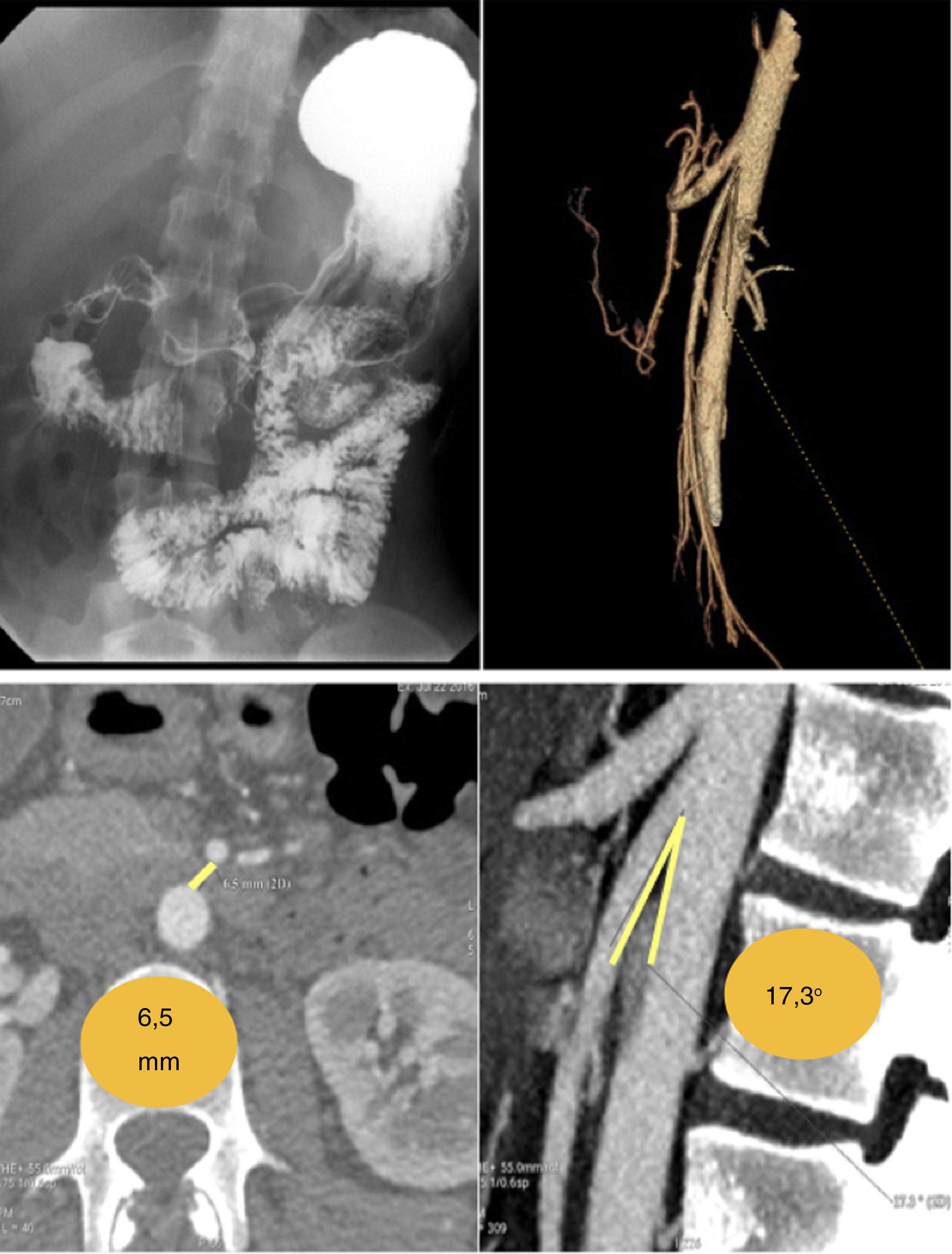
Diagnostic testing was variable. In 85.7%, CT scan with oral contrast was performed, in 14.2% Doppler ultrasound was used, and another 14.2% underwent MRI. Barium contrast studies were used in 42.8% to confirm the suspected compression of the SMAS on the duodenal segment.
Out of the 5 patients who underwent duodenal derotation, 2 presented complications with the need for reoperation: one postoperative pancreatitis that required necrosectomy, cholecystectomy and choledochoduodenostomy; and one stenosis of the anastomosis on the tenth postoperative day due to perianastomotic fibrosis, treated with adhesiolysis and balloon dilation through the jejunostomy.
WS or SMAS is a rare syndrome1 that is not often included in the differential diagnosis of recurrent abdominal pain. It should be considered in patients with malnutrition or hypercatabolism, postprandial abdominal pain and distension that characteristically improves with vomiting or reduced oral intake, as well as in food disorders that lead to low weight, like anorexia nervosa.2,3
The cause may be anatomical malformations4 and adipose tissue loss that diminish the aortomesenteric angle. Other causes include postoperative complications that increase the pressure on the SMAS (postoperative weight loss, adhesions, scoliosis surgery, etc.).5–7
Conservative treatment with nutritional support to sustain weight gain can improve quality of life and avoid complications due to episodes of recurrent intestinal obstruction.
The radiological criteria for diagnosis have not been clearly established. However, in a suggestive clinical context, the presence of an aortomesenteric angle of less than 25° and/or a distance of less than 8mm between the SMAS and the edge of the duodenum should lead us to suspect the possibility of a WS4 (Fig. 1).
Nevertheless, there are false negatives, especially in asymptomatic or oligosymptomatic periods when it may be difficult to objectify duodenal compression or retrograde dilation.
Acute treatment consists of decompression using a nasogastric tube, placement of the patient in the left lateral decubitus position, fluid and electrolyte supplementation, and hypercaloric nutritional therapy, preferably enteral (oral or through a nasogastric tube).8
Given the failure of conservative treatment or clinical persistence, surgical treatment is indicated, and a duodenojejunostomy, gastrojejunostomy or division of the Treitz ligament can be performed to mobilize the duodenum (Strong technique9). The best results are obtained with duodenojejunal anastomosis,3,4,10 as in our case series.
Laparoscopic duodenojejunostomy is an effective, minimally invasive treatment, with an acceptable rate of postoperative complications and favorable long-term results, which is why it is considered the treatment of choice.
FundingThe authors have received no funding for writing this study.
Thanks to Dr. Alberto Colina Alonso, Director of the Department and Clinical Management Unit of General and Gastrointestinal Surgery at the Hospital Universitario Cruces, for his support in surgical research and training.
Please cite this article as: Aranda Escaño E, Perfecto Valero A, Tellaeche de la Iglesia M, Fernández Gómez-Cruzado L, Santidrian Martinez JI. Síndrome de la pinza aorto-mesentérica (Sind. de Wilkie). Análisis de una serie de 5 casos. Cir Esp. 2020;98:48–50.