There are few publications related to postoperative morbidity in hepatic hydatidosis and these have mixed results. The aim of this study was to determine risk and protective factors of postoperative morbidity in patients operated on for hepatic hydatidosis.
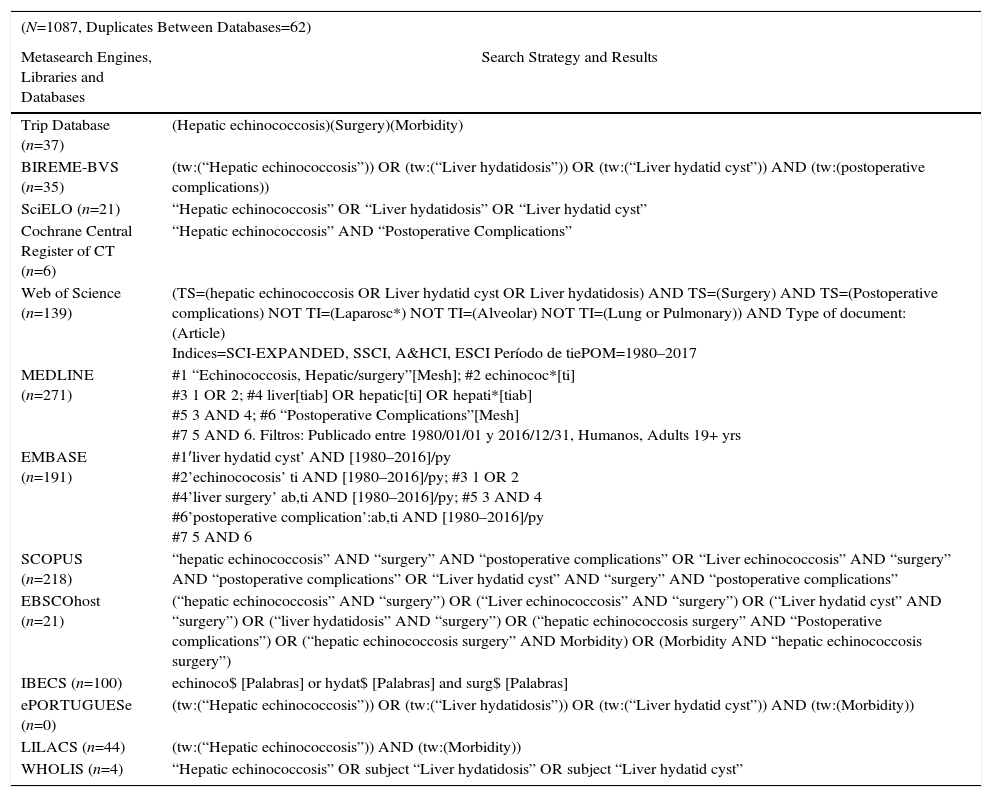
A comprehensive review was made of the evidence, based on systematic reviews, clinical analyses and observational studies, obtained from the Trip Database, BVS, SciELO, Cochrane Central Register of Controlled Trials, WoS, MEDLINE, EMBASE, SCOPUS, EBSCOhost, IBECS, ePORTUGUESe, LILACS and WHOLIS.
1087 related articles were identified; 69 fulfilled the selection criteria (2 systematic reviews, 3 clinical trials and 64 observational studies). Age, history of previous surgery for hepatic hydatidosis, location in the hepatic center, existence of biliary communications and evolutionary complications of the cyst were identified as risk factors, and radical surgical techniques as protective factors.
Risk and protective factors were identified; however, the studies are few and the quality moderate to low.
Las publicaciones relacionadas con morbilidad postoperatoria en hidatidosis hepática son escasas y de resultados disímiles. El objetivo de este estudio fue determinar factores de riesgo y protectores de morbilidad postoperatoria en pacientes intervenidos por hidatidosis hepática.
Se realizó una revisión global de la evidencia, basada en revisiones sistemáticas, ensayos clínicos y estudios observacionales, obtenidos de Trip Database, BVS, SciELO, Cochrane Central Register of Controlled Trials, WoS, MEDLINE, EMBASE, SCOPUS, EBSCOhost, IBECS, ePORTUGUESe, LILACS y WHOLIS.
Se identificaron 1.087 artículos relacionados y 69 cumplían criterios de selección (2 revisiones sistemáticas, 3 ensayos clínicos y 64 estudios observacionales). Se identificaron como factores de riesgo la edad, el antecedente de cirugía previa por hidatidosis hepática, la localización centro hepática, la existencia de comunicaciones biliares y complicaciones evolutivas del quiste y como protectores las técnicas quirúrgicas radicales.
Se identificaron factores de riesgo y protectores; sin embargo, los estudios son escasos y de calidad moderada a baja.
Hydatidosis is an endemic zoonosis in Chile, with an average incidence of 1.9/100000, hospital discharges of 6.3/100000 inhabitants and a mortality rate of 0.2/100000 inhabitants.1 The regions of Aysén and La Araucanía are the most widely affected, the latter with a discharge rate of 28.1/100000 inhabitants.2
This situation determines the need to treat a significant number of new cases of hydatid disease of the liver (HDL) per year in a timely and efficient manner, while investigating evolutionary complications3 and hydatidosis in other locations.4
Despite being an endemic disease in several countries, there have been few publications, with a low level of evidence. Their results are dissimilar, especially regarding the development of postoperative morbidity (POM) and potential variables associated with the development of POM, reason why it is complex to establish strategies to prevent POM in order to control risk factors (RF).
In articles from the 1990s, POM figures were reported between 23.7% and 62.5%.5–10 As of the year 2000, figures between 21.3% and 53.8% were reported,11–14 and from 2010 to date there have been reports of POM between 37.9% and 79.9%.15–17
A global review of the evidence is a qualitative method that is able to combine results from articles extracted from the published literature and later synthesize summaries and conclusions to answer questions related to clinical scenarios of treatment, causes, diagnosis and prognosis. Therefore, they can be used to assess the existing evidence regarding clinical situations in which there is uncertainty, thus allowing subsequent studies to be planned.18
The objective of this study was to summarize the available evidence about associated variables, risk and protective factors (PF) of POM in patients treated surgically for HDL.
MethodsType of StudyOverview of the evidence available.
PopulationIncluded in the study were systematic reviews (SR), clinical trials (CT) and observational studies (OS [concurrent and historical cohorts; cases and controls and case series – CS]) published between January 1980 and May 2017, with no language restriction, that included adult human populations treated surgically for HDL and had evaluated the development of POM. We excluded from the study those articles that included patients treated with laparoscopic surgery, needle aspiration, or injection and re-aspiration, articles with topics unrelated to the objective, reviews of the literature, consensus documents and discussion articles.
Search MethodologyThe search was completed with PICO components (study population [P], intervention in evaluation [I], comparator [C] and outcome [O]). Based on this strategy, we searched for studies with HDL patients (P), who underwent open surgery (I) and whose response variables were POM (O). To this end, the following metasearch engines, libraries and databases were reviewed: Trip Database, BVS, SciELO, Cochrane Central Register of Controlled Trials, WoS, MEDLINE, EMBASE, SCOPUS, EBSCOhost, IBECS, ePORTUGUESe, LILACS and WHOLIS. Sensitive searches were performed using MeSH terms, free words, truncated terms and Boolean connectors (AND and OR), with strategies adapted to each database.
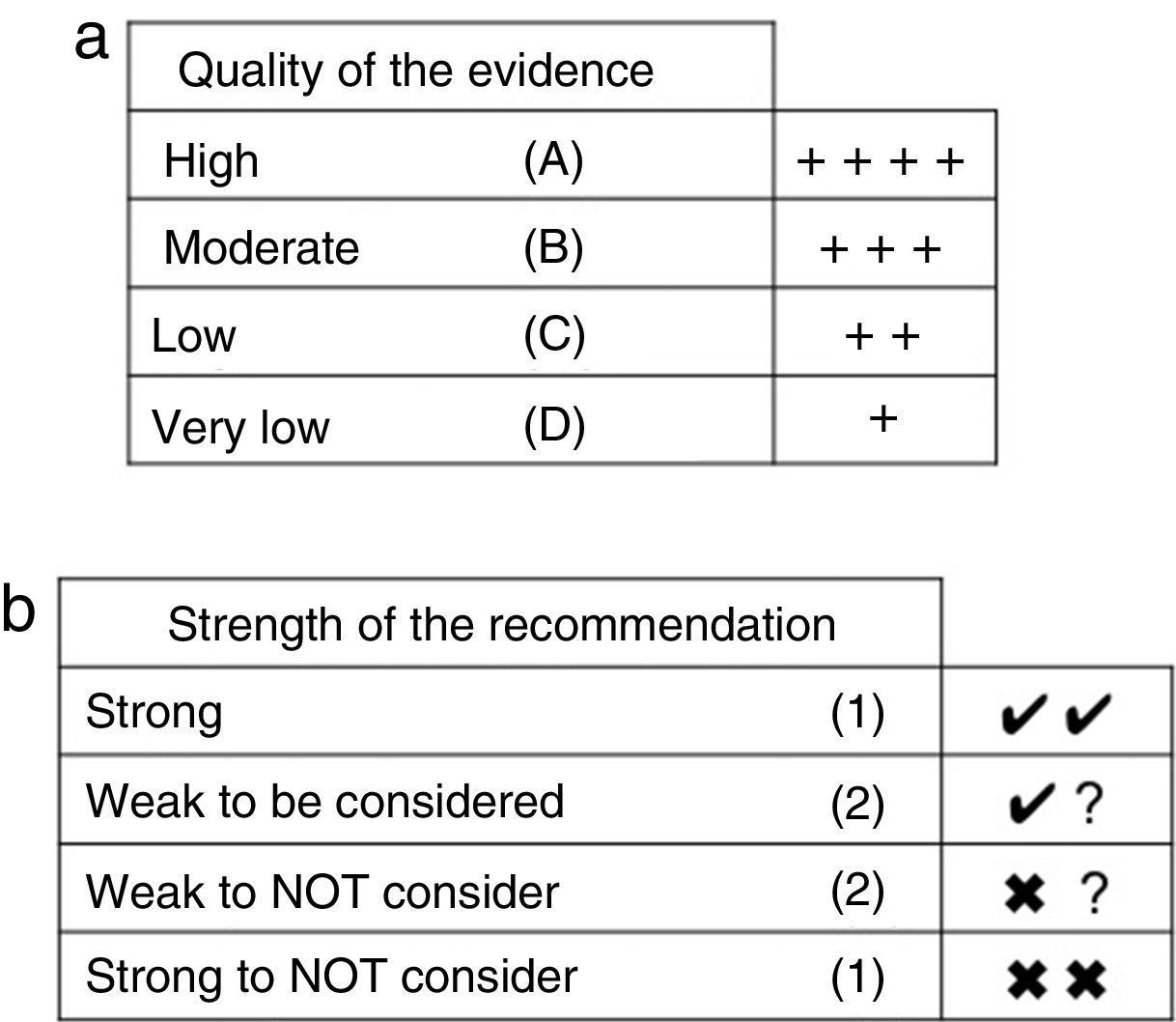
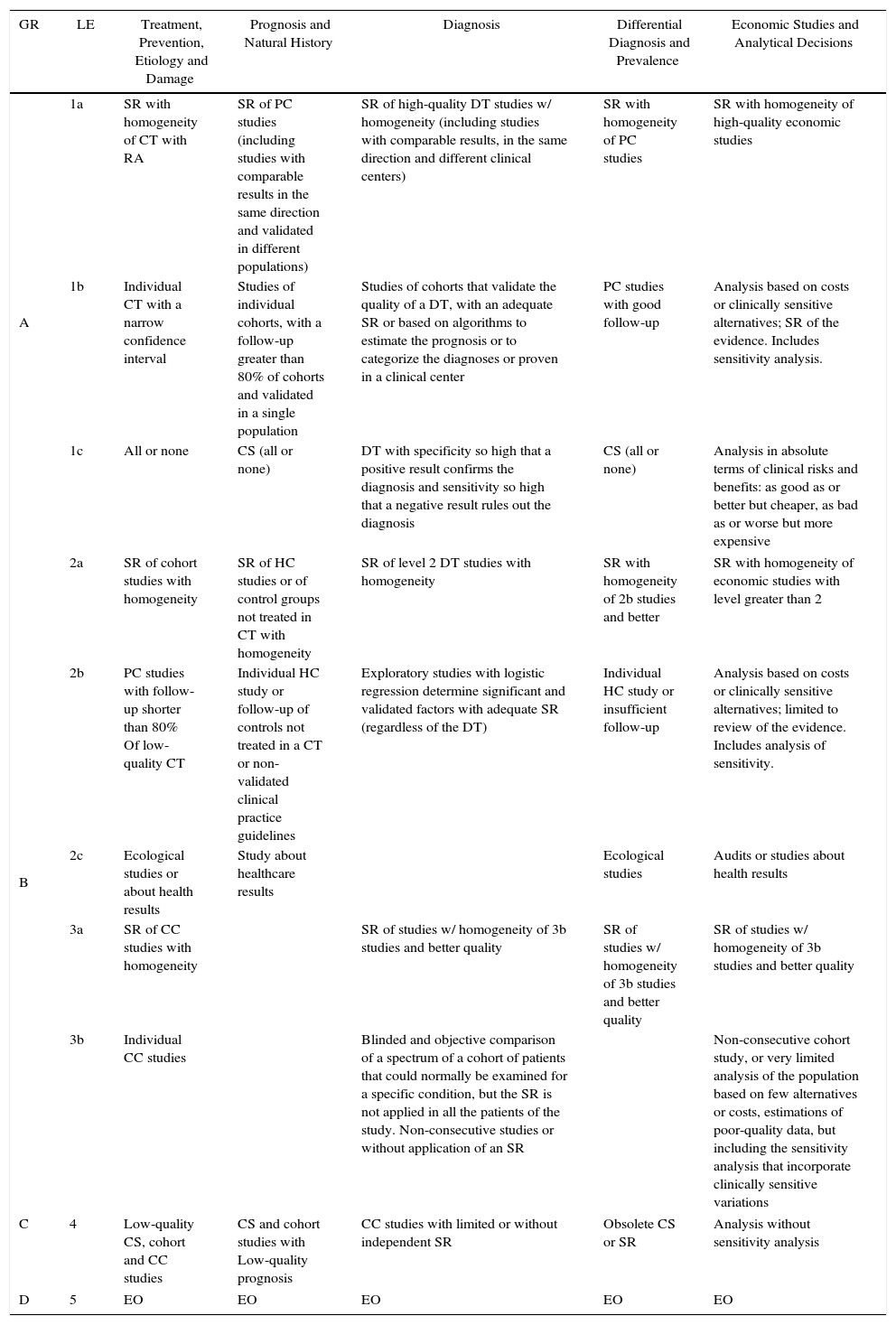
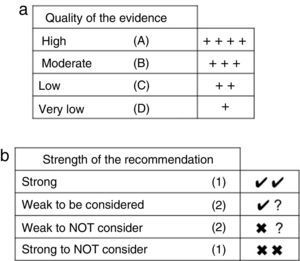
Summary, Assessment and Classification of the EvidenceWe began with an evaluation of the risk of bias (internal validity) of the studies, for which summary tables were generated and validity tables were constructed, using the design proposed by SIGN.19 Subsequently, a classification of levels of evidence was carried out, using the proposal of the Centre for Evidence-Based Medicine20 (Table 1). Finally, a global classification of the evidence was made by applying the GRADE system, which considers the study design, risk of bias, coherence, precision of the results, publication bias and whether the evaluation of the evidence is direct or indirect21 (Fig. 1a and b).
Proposed Classification of the Levels of Evidence of the CEBM 2009.
| GR | LE | Treatment, Prevention, Etiology and Damage | Prognosis and Natural History | Diagnosis | Differential Diagnosis and Prevalence | Economic Studies and Analytical Decisions |
|---|---|---|---|---|---|---|
| A | 1a | SR with homogeneity of CT with RA | SR of PC studies (including studies with comparable results in the same direction and validated in different populations) | SR of high-quality DT studies w/ homogeneity (including studies with comparable results, in the same direction and different clinical centers) | SR with homogeneity of PC studies | SR with homogeneity of high-quality economic studies |
| 1b | Individual CT with a narrow confidence interval | Studies of individual cohorts, with a follow-up greater than 80% of cohorts and validated in a single population | Studies of cohorts that validate the quality of a DT, with an adequate SR or based on algorithms to estimate the prognosis or to categorize the diagnoses or proven in a clinical center | PC studies with good follow-up | Analysis based on costs or clinically sensitive alternatives; SR of the evidence. Includes sensitivity analysis. | |
| 1c | All or none | CS (all or none) | DT with specificity so high that a positive result confirms the diagnosis and sensitivity so high that a negative result rules out the diagnosis | CS (all or none) | Analysis in absolute terms of clinical risks and benefits: as good as or better but cheaper, as bad as or worse but more expensive | |
| B | 2a | SR of cohort studies with homogeneity | SR of HC studies or of control groups not treated in CT with homogeneity | SR of level 2 DT studies with homogeneity | SR with homogeneity of 2b studies and better | SR with homogeneity of economic studies with level greater than 2 |
| 2b | PC studies with follow-up shorter than 80% Of low-quality CT | Individual HC study or follow-up of controls not treated in a CT or non-validated clinical practice guidelines | Exploratory studies with logistic regression determine significant and validated factors with adequate SR (regardless of the DT) | Individual HC study or insufficient follow-up | Analysis based on costs or clinically sensitive alternatives; limited to review of the evidence. Includes analysis of sensitivity. | |
| 2c | Ecological studies or about health results | Study about healthcare results | Ecological studies | Audits or studies about health results | ||
| 3a | SR of CC studies with homogeneity | SR of studies w/ homogeneity of 3b studies and better quality | SR of studies w/ homogeneity of 3b studies and better quality | SR of studies w/ homogeneity of 3b studies and better quality | ||
| 3b | Individual CC studies | Blinded and objective comparison of a spectrum of a cohort of patients that could normally be examined for a specific condition, but the SR is not applied in all the patients of the study. Non-consecutive studies or without application of an SR | Non-consecutive cohort study, or very limited analysis of the population based on few alternatives or costs, estimations of poor-quality data, but including the sensitivity analysis that incorporate clinically sensitive variations | |||
| C | 4 | Low-quality CS, cohort and CC studies | CS and cohort studies with Low-quality prognosis | CC studies with limited or without independent SR | Obsolete CS or SR | Analysis without sensitivity analysis |
| D | 5 | EO | EO | EO | EO | EO |
RA: random assignation; CC: cases and controls; HC: historic cohorts; PC: prospective cohorts, individual, with homogeneity; CT: clinical trial; SR: standard of reference; GR: grade of recommendation; LE: level of evidence; EO: expert opinion without explicit critical evaluation, not based on physiology, nor on judicial research work, nor on fundamental principles; DT: diagnostic tests; SR: systematic review; CS: case series.
We evaluated preoperative clinical variables, parasite and surgical variables that could influence the development of POM.
DefinitionsRF were defined as variables that determined the probability (estimated through measures of association and their respective 95% confidence intervals [95%CI]), for developing an event of interest (development of POM). PF were defined as variables capable of reducing the probability (estimated through measures of association and 95%CI) for developing POM. Finally, associated variables were defined as those associated with the outcome of interest (POM), but lacked a measure of association with the respective 95%CI, or whose result was meager (value close to 1 or 95%CI of 1).
Statistical AnalysisThe selected data were compiled in an Excel spreadsheet. Clinical trials included in an SR were not considered in the analysis. No statistical analyses are used in this type of study design.
Ethical ConsiderationsAuthors and study centers were not revealed so as to reduce selection and analytical bias.
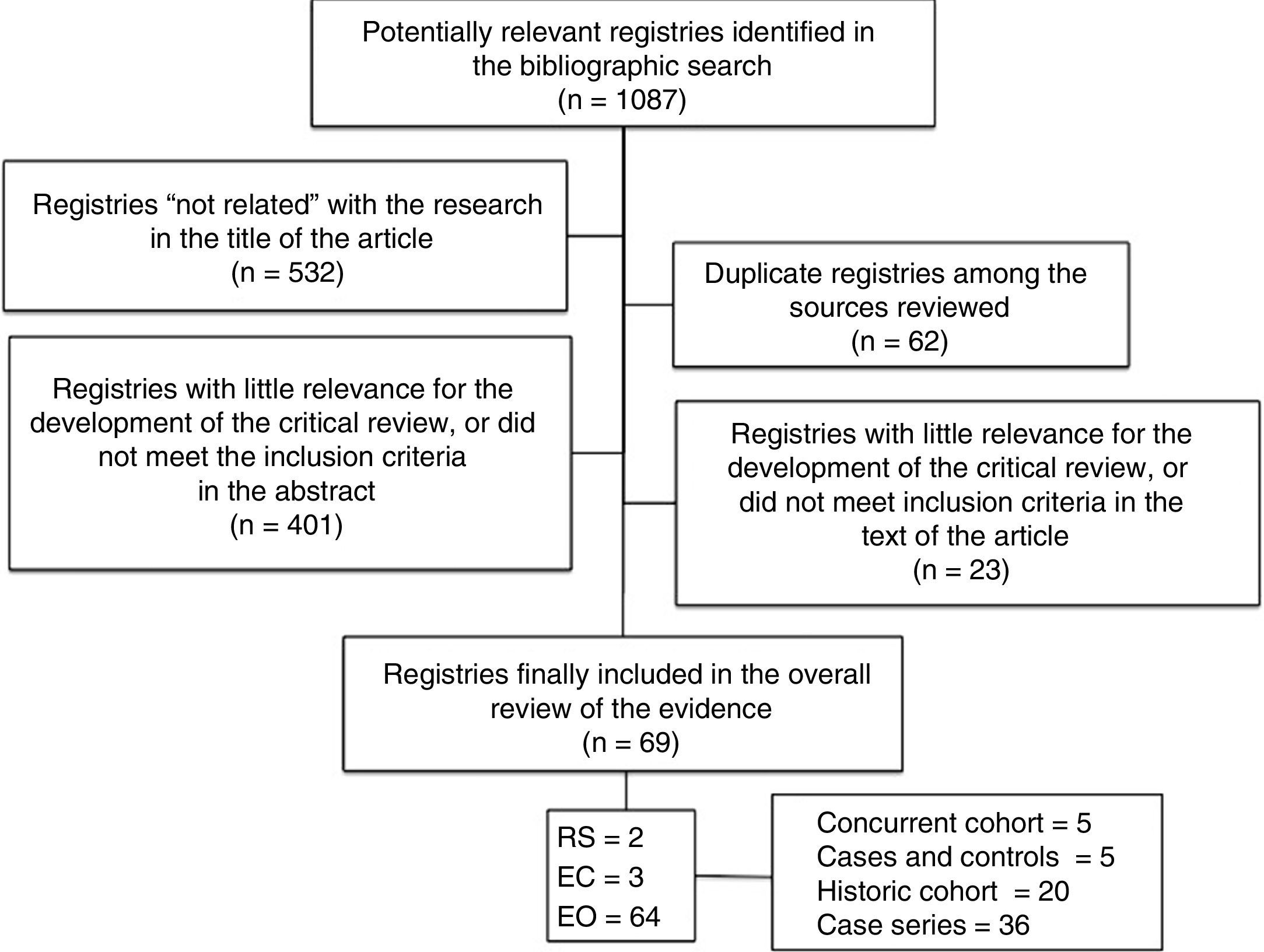
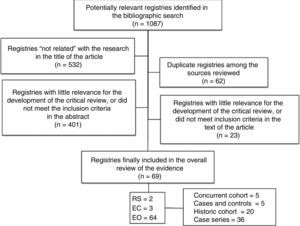
ResultsFrom the indicated search, 1087 studies were identified. After analyzing the titles, 532 were discarded because they were considered “unrelated” to the investigation. In this same stage, it was verified that 62 were duplicate articles among the databases consulted (Table 2). Afterwards, the abstracts were then analyzed, which eliminated 401 studies because they had little relevance for the review, or because they did not meet the selection criteria. Then we proceeded to the in-depth analysis of the 92 selected studies, and the detailed reading of these confirmed the definitive inclusion of 69 studies that fulfilled the selection criteria: 2 RS, one composed of 32 retrospective studies22 and the other by 5 studies without randomized assignment23; three low-quality CT24–26 and 64 OS (5 concurrent cohort studies27–31; 3 case and control, 2 nested in one cohort32,33 and another that was not34; 20 historical cohorts9,13,15,17,35–50 and 36 CS,3–8,10–12,14,16,29,51–74 representing a population of 11403 subjects that are the object of this analysis) (flowchart of identified studies [Fig. 2]).
Search Strategies and Results Obtained for Each Source of Information Used.
| (N=1087, Duplicates Between Databases=62) | |
|---|---|
| Metasearch Engines, Libraries and Databases | Search Strategy and Results |
| Trip Database (n=37) | (Hepatic echinococcosis)(Surgery)(Morbidity) |
| BIREME-BVS (n=35) | (tw:(“Hepatic echinococcosis”)) OR (tw:(“Liver hydatidosis”)) OR (tw:(“Liver hydatid cyst”)) AND (tw:(postoperative complications)) |
| SciELO (n=21) | “Hepatic echinococcosis” OR “Liver hydatidosis” OR “Liver hydatid cyst” |
| Cochrane Central Register of CT (n=6) | “Hepatic echinococcosis” AND “Postoperative Complications” |
| Web of Science (n=139) | (TS=(hepatic echinococcosis OR Liver hydatid cyst OR Liver hydatidosis) AND TS=(Surgery) AND TS=(Postoperative complications) NOT TI=(Laparosc*) NOT TI=(Alveolar) NOT TI=(Lung or Pulmonary)) AND Type of document: (Article) Indices=SCI-EXPANDED, SSCI, A&HCI, ESCI Período de tiePOM=1980–2017 |
| MEDLINE (n=271) | #1 “Echinococcosis, Hepatic/surgery”[Mesh]; #2 echinococ*[ti] #3 1 OR 2; #4 liver[tiab] OR hepatic[ti] OR hepati*[tiab] #5 3 AND 4; #6 “Postoperative Complications”[Mesh] #7 5 AND 6. Filtros: Publicado entre 1980/01/01 y 2016/12/31, Humanos, Adults 19+ yrs |
| EMBASE (n=191) | #1′liver hydatid cyst’ AND [1980–2016]/py #2’echinococosis’ ti AND [1980–2016]/py; #3 1 OR 2 #4’liver surgery’ ab,ti AND [1980–2016]/py; #5 3 AND 4 #6’postoperative complication’:ab,ti AND [1980–2016]/py #7 5 AND 6 |
| SCOPUS (n=218) | “hepatic echinococcosis” AND “surgery” AND “postoperative complications” OR “Liver echinococcosis” AND “surgery” AND “postoperative complications” OR “Liver hydatid cyst” AND “surgery” AND “postoperative complications” |
| EBSCOhost (n=21) | (“hepatic echinococcosis” AND “surgery”) OR (“Liver echinococcosis” AND “surgery”) OR (“Liver hydatid cyst” AND “surgery”) OR (“liver hydatidosis” AND “surgery”) OR (“hepatic echinococcosis surgery” AND “Postoperative complications”) OR (“hepatic echinococcosis surgery” AND Morbidity) OR (Morbidity AND “hepatic echinococcosis surgery”) |
| IBECS (n=100) | echinoco$ [Palabras] or hydat$ [Palabras] and surg$ [Palabras] |
| ePORTUGUESe (n=0) | (tw:(“Hepatic echinococcosis”)) OR (tw:(“Liver hydatidosis”)) OR (tw:(“Liver hydatid cyst”)) AND (tw:(Morbidity)) |
| LILACS (n=44) | (tw:(“Hepatic echinococcosis”)) AND (tw:(Morbidity)) |
| WHOLIS (n=4) | “Hepatic echinococcosis” OR subject “Liver hydatidosis” OR subject “Liver hydatid cyst” |
A low-quality SR with a historical cohort study stated that, in order to reduce POM, a surgical team with experience in hepatobiliary surgery is required, along with adequate infrastructure, perioperative support and a rigorous follow-up to be able to analyze complications23,50 (treatment studies 3a and 4 and prognostic studies 2a and 2b).
AgeThere is a series of articles that suggest that this is a variable associated with the development of POM. An SR identified a tendency for higher POM in patients aged ≥61 years (POM: 25.4%, OR 1.38 [0.74–2.57], P=.310)23 (treatment study 3a and prognosis study 2a). Something similar was verified in a nested case-control study, in which age >45 years is indicated as a cut-off point for all types of cysts (P=.017; OR: 1.1 [1.0; 1.1]).32 In another study of equivalent design, age >60 years was estimated as the cut-off point in uncomplicated cysts (P=.002; OR: 1.1 [1.0–1.1]])33 (treatment study 3b and prognosis 2b). Finally, a CS mentioned the cut-off point of age >61 (POM of 64.3% vs 38.6% in the subgroup aged 41–60 years, and 23.5% of the subgroup aged <40 years of age; P=.0412) (treatment and prognosis studies 4).
History of Previous Surgery for Hydatid Disease of the LiverThere is evidence to indicate this as an RF compared to patients who are operated on for the first time, which is supported by a nested case–control study (P=.018; OR: 4.1 [1.3–13.2])32 (treatment study 3b and prognostic study 2b).
Laboratory VariablesA CS observed that, in patients with POM, average alkaline phosphatase levels were 616±576U/L vs 397±440U/L in those who did not develop POM62 (treatment and prognosis study 4).
Parasite VariablesLocationEvidence was found in a nested case–control study that supported that the central location of the liver in uncomplicated cysts is associated with higher POM than lateral locations (P=.003; OR: 3.9 [1.6–9.8])33 and 2 CS mentioned the location in the “liver dome” as an RF63,65; P<.0001, OR: 2.84 (95%CI: 1.58–5.07)63 (treatment studies 3b and 4 and prognosis studies 2b and 4).
DiameterA historical cohort concluded that cysts >10cm in diameter were associated with higher POM.42 In 4 CS, it was observed that cyst diameter was associated with the development of more complications. Two set a cut-off point of 10cm,61,65 with a POM of 30.0% and 26.6%, respectively; another one also set it at 10cm (POM 44.4% in cysts larger than 10cm vs 24.5% in those smaller than 10cm; P=.002; OR: 16.7 95%CI: 1.2–4.45)12 and another set the cut-off point at 9cm63 (treatment and prognosis study 4).
NumberThere is evidence based on an RS that there is higher POM in patients with 3 or more cysts compared to those with 2 or fewer (POM 30.0% vs 14.5%; OR: 3.1 [1.85–5.17]; P=.001).23 Also, a historical cohort study concluded that having 3 or more cysts is an independent variable for greater POM (OR: 2.55; 95%CI: 1.42–4.59)41 (treatment studies 3b and 4 and prognosis studies 2a and 2b).
Wall ThicknessThere is evidence that the thicker the cyst wall, the higher the risk for POM, based on an RS (POM 23.1% vs 6.2%; OR: 2.59 [1.27–5.29]; P=.009)23 (treatment study 3a and prognosis study 2a).
Cystobiliary CommunicationsThe existence of cystobiliary communications (CBC) is an RF for the development of POM, based on an RS (POM 32.9% vs 135%; OR: 227 [1.38–372]; P=.001)23 (treatment study 3a and prognosis study 2a). This fact is also supported by a concurrent cohort (POM without CB 9.4% vs 21.8% with CB; P<.001; RR: 3.4 [2.6–4.2])30 and 2 CS that report POM in the presence of CBC of up to 25.0%60,63; P=.024; OR: 2.3 (95%CI: 1.11–4.85)63 (treatment studies 2b and 4 and prognosis studies 1b and 4).
Coexistence of Evolutive ComplicationsThere is evidence based on an RS that found greater POM in patients with cyst complications compared to uncomplicated cysts (POM 35.5% vs 19.6%; OR: 2.55 [1.42–4.59]; P=.002)23 (treatment study 3a and prognosis study 2a). Furthermore, there is a historic cohort and 2 CS that provide evidence on this item: in this first, POM was verified at 27.8% vs 15.2% in patients with complicated HDL compared to those without complications (P=.02545); the series described that the coexistence of evolutive complications of HDL versus uncomplicated cysts were associated with 20.0% vs 9.0% POM,62 while verifying that the POM in complicated cysts was 52.0% vs 21.0% when uncomplicated; P<.00112 (treatment study 4 and prognosis studies 2b and 4).
By separating the different evolutive complication options of cysts, we found evidence to support the position that cyst infection, presence of cholangiohydatidosis, existence of hepatothoracic transit and hydatid seeding are associated with the development POM22,45 (treatment studies 3a and 4 and prognosis studies 2a and 4).
Cyst infection. There is evidence based on a prospective cohort showing that secondary hepatic abscess in patients with HDL behaves as an RF for the development of POM (28.9% vs 11.1%; P=.001; RR: 2.5 [1.4–5.0]).29 On the other hand, a CS reported a POM of 23.4% in this type of cases34 (treatment studies 2b and 4 and prognosis study 1b and 4).
Cholangiohydatidosis. Two CS were found about the role of cholangiohydatidosis as an entity associated with higher POM in patients with HDL. Both included few cases and reported POM with and without secondary acute cholangitis of 30.0% and 23.0%, respectively70,73 (treatment and prognosis study 4).
Hepatothoracic transit. Four small CS were found (37–42 cases) that reported POM from 24.3% to 58.1%52,54,59,71 (treatment and prognosis study 4).
Hydatid seeding. There is available evidence that in an RS showing that patients with HDL that present hydatid seeding, and therefore require procedures in addition to the treatment of HDL, have a greater probability to develop POM, which can reach 35.0%23 (treatment study 3a and prognosis study 2a). In addition, evidence was found from a retrospective cohort39 that verified statistically significant differences between patients with and without HDL rupture (26% vs 15%; P=.018) and in 3 small CS (17–43),4,64,74 in which POM reached 35.3% (treatment and prognosis study 4).
Surgical VariablesTreatment of Cystobiliary CommunicationsThere is evidence from a low-quality RS that supports the use of the Kehr tube versus choledochoduodenostomy (POM: 18.1% Kehr tube vs 40.0%)22 (treatment study 3a and prognosis study 2a). Something similar has been seen in a historic cohort and 2 CS37,53,69 (treatment and prognosis study 4). Finally, a concurrent cohort advocates simple suture of the biliary comunications30 (treatment study 2b and prognosis study 1b).
Surgical AlternativesEvidence was found in favor of radical surgery vs conservative techniques, demonstrating that radical techniques were associated with lower POM. One RS (POM: 17.7% vs 34.6%; OR=0.42, 95%CI: 0.32–0.56; P<.00001) indicated that radical surgery is a PF against the development of POM compared to conservative surgery).23 Further evidence: one CT (POM: 0.0% vs 35.3%; P=.011)25; 7 historic cohorts (POM: 13.3% vs 31.4%; P<.001),35 (POM: 16.6 vs 42.8%; P<.05),9 (POM: 3.2% vs 11.6%; P<.001),40 (POM: 26% vs 45%; P<.05)15; (POM: 19.0 vs 28.0; P<.05),44 (POM: 16.2% vs 79.9%; P<.001),17 (POM: 0.0% vs 31.0%; P=.004)49 (treatment studies 3a, 2b and 4, and prognosis studies 2a, 2b and 4). However, in a case–control study, no differences were verified (POM: 15.0% vs 19.0%; OR: 1.28; 95%CI: 0.57–2.86),34 which was likewise reported in a historic cohort (POM: 16.6% vs 24.2%; P>.05)43 (treatment and prognosis study 4).
There is also evidence comparing the results obtained from cystectomy, cystojejunostomy and Posadas procedure, showing evidence in favor of cystectomy over the Posadas in a historic cohort (POM: 0.0% vs 31.6%; P=.005)38 and partial cystectomy over other techniques in a historic cohort (POM: 7.3% vs 14.3%; P<.05).47 There is also evidence to support he use of Roux-en-Y cystojejunostomy versus cystectomy in a historic cohort (POM: 7.7% vs 40.0%; P<.05).48 Further evidence shows that cystectomy is superior to polar drainage and cystostomy with cavity wall suture, based on a historic cohort (POM: 8.3% vs 32.5%; POM: 8.3% vs 54.5%; POM: 8.3% vs P=.0037)13 (treatment and prognosis study 4).
Other evidence enables us to compare the results obtained by applying drainage vs other options in the treatment of the residual cavity. Evidence was confirmed that supports omentoplasty vs drainage based on a CT (POM: 22.7% vs 42.9%; P=.00163),26 2 concurrent cohorts (POM: 23.0% vs 6.0%; P=.03),27 (POM: 5.7% vs 16.6%; P<.05)28 and a historic cohort (POM: 9.7% vs 32.5%; P<.05)13 (treatment studies 2b and 4, and prognosis studies 1b, 2b and 4).
More evidence demonstrates that the use of drainage is associated with less development of POM than the use of cavity wall suture in a historic cohort (POM: 32.5% vs 54.4%; P<.05).13 However, in another historic cohort, the results show that it is the use of cavity wall suture which is associated with lower POM (POM: 5.6% vs 15.4%; P<.05)46 (treatment and prognosis study 4). Finally, there is evidence that the lack of use of drainage is associated with a lower POM than the use of drainage once the surgical procedure is done, based in a historic cohort (POM: 10.0% vs 44.7%; P<.05)36 (treatment and prognosis study 4).
Furthermore, there is evidence regarding the utilization of cavity wall suture vs omentoplasty, which indicates that the use of cavity wall suture associated with drainage is a PF against POM compared to the use of omentoplasty and cavity wall suture without drainage, based on an RS (POM 15.3% vs 23.8% vs 25.6%; OR: 2.23 [1.12–4.44]; P=.023)23 (treatment study 3a and prognosis study 2a). Evidence was also found in favor of using cavity wall suture over omentoplasty in a concurrent cohort (POM: 2.5% vs 18.8%; P=.04 and RR: 0.3 [0.03–0.70]), which determined that the use of cavity wall suture would be a PF against the development of local complications31 and in a historic cohort (POM: 28.6% vs 50.0%; P=.005)38 (treatment studies 2b and 4 and prognosis studies 1b and 4).
However, there is also evidence in favor of using omentoplasty versus not using it based on a multicenter CT (POM: 10.0% vs 34.0%; P<.03)24 and also in favor of using omentoplasty vs cavity wall suture in a historic cohort (POM: 9.7% vs 54.5%; P=.003713) (treatment and prognosis studies 2b and 4).
With regards to the need for additional surgery, there is evidence supporting that the treatment of concomitant localizations of HDL is associated with higher POM, based on a historic cohort13 and 2 CS12,14 (treatment and prognosis study 4).
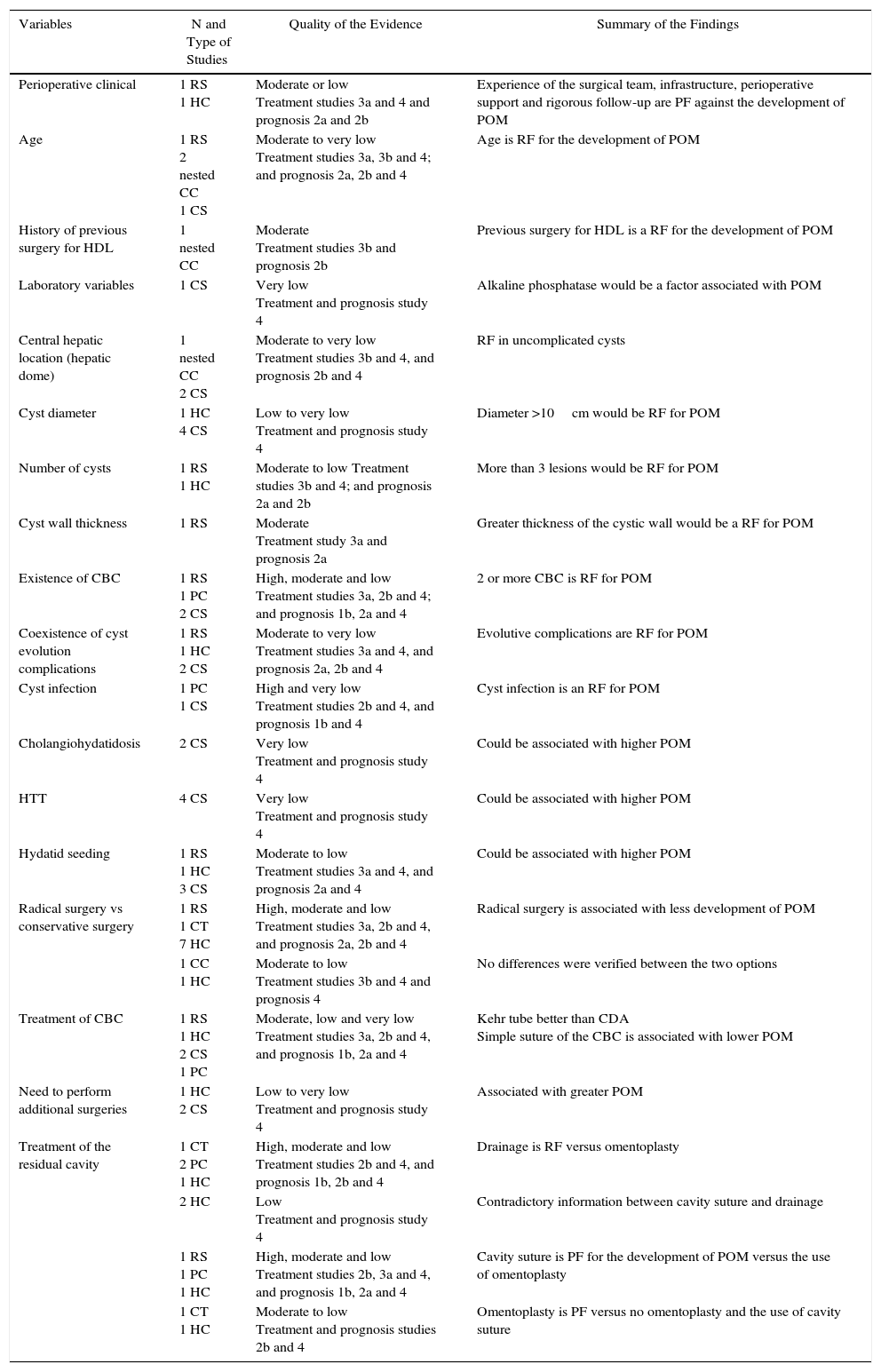
The findings mentioned above are summarized in Table 3, which also indicates the corresponding quality of the evidence.
Summary of the Evidence Found.
| Variables | N and Type of Studies | Quality of the Evidence | Summary of the Findings |
|---|---|---|---|
| Perioperative clinical | 1 RS 1 HC | Moderate or low Treatment studies 3a and 4 and prognosis 2a and 2b | Experience of the surgical team, infrastructure, perioperative support and rigorous follow-up are PF against the development of POM |
| Age | 1 RS 2 nested CC 1 CS | Moderate to very low Treatment studies 3a, 3b and 4; and prognosis 2a, 2b and 4 | Age is RF for the development of POM |
| History of previous surgery for HDL | 1 nested CC | Moderate Treatment studies 3b and prognosis 2b | Previous surgery for HDL is a RF for the development of POM |
| Laboratory variables | 1 CS | Very low Treatment and prognosis study 4 | Alkaline phosphatase would be a factor associated with POM |
| Central hepatic location (hepatic dome) | 1 nested CC 2 CS | Moderate to very low Treatment studies 3b and 4, and prognosis 2b and 4 | RF in uncomplicated cysts |
| Cyst diameter | 1 HC 4 CS | Low to very low Treatment and prognosis study 4 | Diameter >10cm would be RF for POM |
| Number of cysts | 1 RS 1 HC | Moderate to low Treatment studies 3b and 4; and prognosis 2a and 2b | More than 3 lesions would be RF for POM |
| Cyst wall thickness | 1 RS | Moderate Treatment study 3a and prognosis 2a | Greater thickness of the cystic wall would be a RF for POM |
| Existence of CBC | 1 RS 1 PC 2 CS | High, moderate and low Treatment studies 3a, 2b and 4; and prognosis 1b, 2a and 4 | 2 or more CBC is RF for POM |
| Coexistence of cyst evolution complications | 1 RS 1 HC 2 CS | Moderate to very low Treatment studies 3a and 4, and prognosis 2a, 2b and 4 | Evolutive complications are RF for POM |
| Cyst infection | 1 PC 1 CS | High and very low Treatment studies 2b and 4, and prognosis 1b and 4 | Cyst infection is an RF for POM |
| Cholangiohydatidosis | 2 CS | Very low Treatment and prognosis study 4 | Could be associated with higher POM |
| HTT | 4 CS | Very low Treatment and prognosis study 4 | Could be associated with higher POM |
| Hydatid seeding | 1 RS 1 HC 3 CS | Moderate to low Treatment studies 3a and 4, and prognosis 2a and 4 | Could be associated with higher POM |
| Radical surgery vs conservative surgery | 1 RS 1 CT 7 HC | High, moderate and low Treatment studies 3a, 2b and 4, and prognosis 2a, 2b and 4 | Radical surgery is associated with less development of POM |
| 1 CC 1 HC | Moderate to low Treatment studies 3b and 4 and prognosis 4 | No differences were verified between the two options | |
| Treatment of CBC | 1 RS 1 HC 2 CS 1 PC | Moderate, low and very low Treatment studies 3a, 2b and 4, and prognosis 1b, 2a and 4 | Kehr tube better than CDA Simple suture of the CBC is associated with lower POM |
| Need to perform additional surgeries | 1 HC 2 CS | Low to very low Treatment and prognosis study 4 | Associated with greater POM |
| Treatment of the residual cavity | 1 CT 2 PC 1 HC | High, moderate and low Treatment studies 2b and 4, and prognosis 1b, 2b and 4 | Drainage is RF versus omentoplasty |
| 2 HC | Low Treatment and prognosis study 4 | Contradictory information between cavity suture and drainage | |
| 1 RS 1 PC 1 HC | High, moderate and low Treatment studies 2b, 3a and 4, and prognosis 1b, 2a and 4 | Cavity suture is PF for the development of POM versus the use of omentoplasty | |
| 1 CT 1 HC | Moderate to low Treatment and prognosis studies 2b and 4 | Omentoplasty is PF versus no omentoplasty and the use of cavity suture |
CC: cases and controls; CDA: choledochoduodenostomy; HC: historical or retrospective cohort; PC: concurrent or prospective cohort; CBC: cystobiliary communications; CT: clinical trial; PF: protective factor; RF: risk factor; POM: postoperative morbidity; CS: case series; HTT: hepatothoracic transit.
High quality: additional research is highly unlikely to modify our confidence in the estimations of the effect.21
Moderate quality: additional research is likely to have an important effect in our confidence in the estimation of the effect and may change it.21
Low quality: additional research is very unlikely to have an important impact on our confidence in the estimation of the effect, and it is likely to change the estimation.21
Very low quality: any estimation of the effect is highly uncertain.21
For reasons of efficiency, this review was based on a critical evaluation of the best available evidence from the last 36 years, preferably in the form of SR. When these did not exist, CT and OS were identified. Consequently, we proceeded in a hierarchical manner, prioritizing levels of evidence and recommendation grades.
In this report, no recommendations have been made, since we believe that these should be formulated for each specific setting based on the overall quality of the evidence, initially assessing the balance between benefits and risks and finally taking into account factors such as local context, baseline risk of the population, values and preferences, as well as the associated costs.21
In our study, we decided to exclude patients treated with laparoscopy because these are usually subgroups with uncomplicated lesions that are smaller in size, with no preoperative evidence of cystobiliary communications, etc. In short, patients selected for laparoscopic surgery have a lower risk for POM.
The limitations of the study are mainly due to the low methodological quality of most of the studies that were included. However, some biases (selection, analysis and publication) were reduced with a thorough search of the literature, carried out in various sources of information and with the blinding of authors and centers.
It is difficult to find answers that explain why, in spite of technological advances, the POM of HDL surgery continues to have figures that have not changed substantially in the last 7 years, as there continue to be reports between 37.9% and 79.9%,15–17 especially when looked at from the perspective that it is a benign disease. The only way to comprehend the possible reasons for such variability would be to consider the heterogeneity of the studied populations, the different techniques applied and the diverse level of experience of the groups that report their results, which lead to an uncertainty that must be clarified.
We have identified some variables that can be considered RF for the development of POM in patients treated surgically for HDL (Table 3), including: age, history of previous surgery for HDL, location in the liver center in uncomplicated cysts, the existence of CBC (especially when there are 2 or more), and the coexistence of evolutive cyst complications (especially cyst infection). Additionally, radical surgical techniques appear as PF against the development of POM, as well as the treatment of CBC with simple suture or Kehr tube and the use of cavity wall suture versus omentoplasty. However, all of these are based on moderate to low quality evidence studies, which is why these results should be observed with caution.
Other variables that would be associated with higher POM in patients operated on for HDL were verified, such as cyst diameter (>10cm), the need to perform additional surgeries, and elevated lab workup variables, such as alkaline phosphatase. All of these are supported by quality studies of moderate, low or very low evidence, and could even be confounding or effect-modifying variables.
However, most of the studies analyzed reported results from heterogeneous populations (for example, mixing complicated and uncomplicated HDL), so that a variable that appears to be an RF might only be an effect of classification, measurement and even confounding bias.
What follows this manuscript is the development of a predictive model for POM in patients operated on for HDL, using a classification and regression tree analysis like CART (non-linear and non-parametric alternative to linear regression models), which is a robust tool that can be applied to numerical and categorical data, facilitating the identification and interpretation of complex interactions.75
As a conclusion, we can point out that the information regarding the development of POM in patients operated on for HDL is limited, heterogeneous and mostly from low-quality studies with low levels of evidence. In certain items, the results leave us with more questions than answers. It is therefore necessary to have a greater number of primary studies with a good level of evidence and quality in order to resolve the existing uncertainty regarding the existence of RF for the development of POM (for example, determining the effect that 2 or more RF could have when existing together in a population treated surgically for HDL).
FundingThis study has been partially funded by the DID-UFRO DI16-0119 project of the Research and Development Administration at the Universidad de La Frontera, Chile.
Conflict of InterestsNone.
Please cite this article as: Manterola C, Otzen T, Muñoz G, Alanis M, Kruuse E, Figueroa G. Cirugía de la hidatidosis hepática. Factores de riesgo y variables asociadas al desarrollo de morbilidad postoperatoria. Revisión global de la evidencia existente. Cir Esp. 2017;95:566–576.