Cardiac myxomas account for 50% of all benign cardiac tumors. Their clinical presentation varies from embolisms to fever. Our objective was to describe the surgical experience in the resection of cardiac myxomas during an 8-year period.
MethodsThis is a retrospective, descriptive study of a series of cases with cardiac myxomas diagnosed from 2014 to 2022 at a tertiary care center. Descriptive statistics were used to define the populational and surgical characteristics. We used Pearson’s correlation to study the relationship between postoperative complications and age, tumor size and affected cardiac chamber.
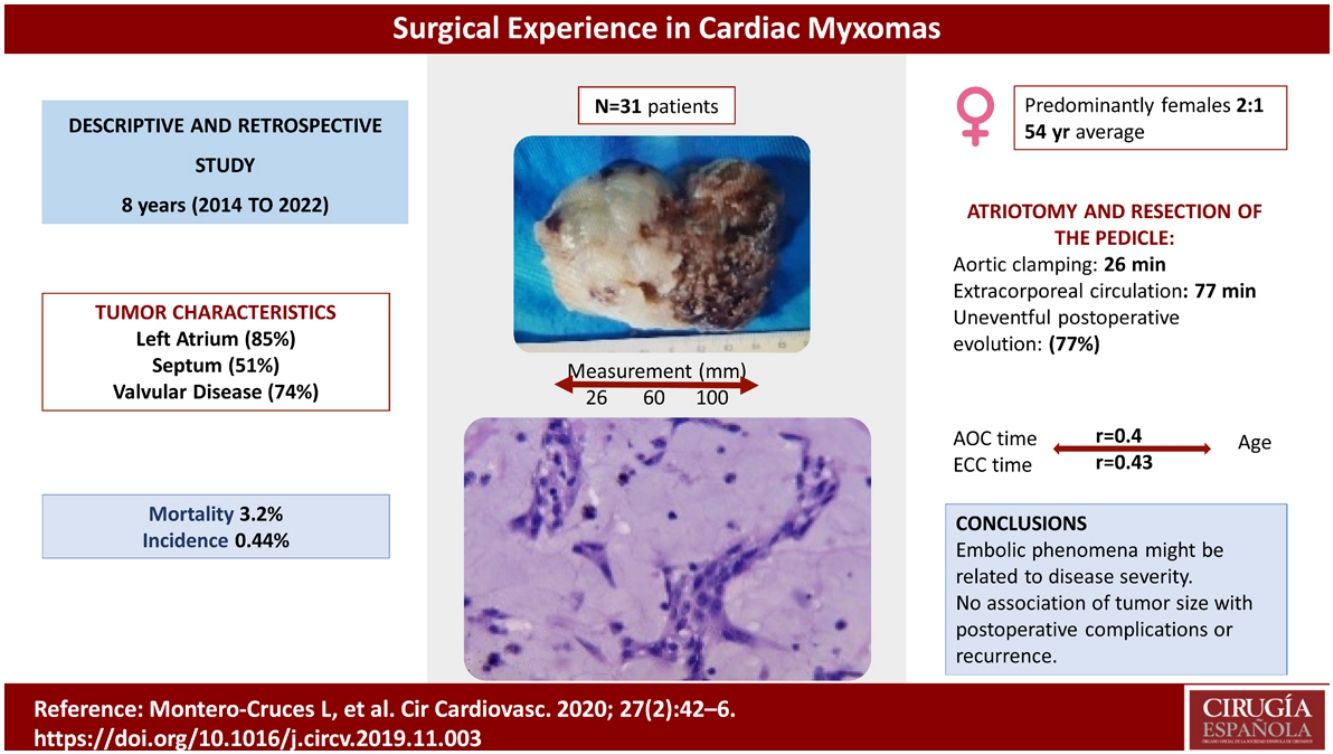
Results31 patients were included, with a predominance of females (1:2 ratio). The prevalence was 0.44%, which was calculated based on the number of cardiac surgeries performed in our unit over the 8-year period. The main clinical manifestation was dyspnea (85%, n = 23), followed by cerebrovascular event (CVE) (18%, n = 5). Atriotomy and resection of the pedicle were performed with preservation of the interatrial septum. Mortality was 3.2%. The postoperative evolution was uneventful in 77%. Tumor recurrence occurred in 2 patients (7%), both debuting with embolic phenomena. No association was observed between postoperative complications or recurrence and tumor size, nor aortic clamping and extracorporeal circulation times with regard to age.
ConclusionsFour atrial myxoma resections are performed in our unit per year, with an estimated prevalence of 0.44%. The tumor characteristics described coincide with the previous literature. A relationship between embolisms and recurrences cannot be ruled out. Wide surgical resection of the pedicle and base of tumor implantation may influence tumor recurrence, although further studies are needed.
Los mixomas cardíacos representan el 50% de los tumores cardíacos benignos. La presentación clínica varía desde embolismos hasta fiebre. El objetivo fue describir la experiencia quirúrgica en la resección de mixomas cardíacos durante 8 años.
MétodosEstudio retrospectivo, descriptivo, de serie de casos de mixomas cardíacos diagnosticados entre 2014 y 2022 en un centro de tercer nivel. Se utilizó estadística descriptiva para definir las características poblacionales y quirúrgicas. Mediante la correlación de Pearson se estudió la relación entre las complicaciones postoperatorias y la edad, el tamaño del tumor y la cavidad cardiaca afectada.
ResultadosSe incluyeron 31 pacientes, predominantemente mujeres (1:2). La prevalencia fue 0.44%, calculada en base a las cirugías cardíacas realizadas en nuestra unidad durante 8 años. La principal manifestación fue disnea (85%, n = 23), seguida de EVC (18%, n = 5). Se realizó atriotomía y resección del pedículo con preservación del tabique interauricular. La mortalidad fue del 3.2%. La evolución posquirúrgica fue adecuada en el 77%. La recidiva ocurrió en 2 pacientes (7%), debutando ambos con embolismos. No se observó asociación entre las complicaciones postoperatorias o recurrencia y el tamaño tumoral; ni en pinzamiento aórtico y los tiempos de circulación extracorpórea con respecto a la edad.
ConclusionesEn nuestra unidad se realizan cuatro resecciones de mixoma auricular anuales (prevalencia de 0.44%). Las características tumorales descritas coinciden con la literatura previa. No se descarta relación entre embolismos y recurrencias. La resección amplia del pedículo y base del tumor puede influir en la recurrencia tumoral, aunque, se requieren más estudios.
Cardiac myxomas account for 50% of all benign heart tumors, followed by lipomas (21%), papillary fibroelastomas (16%), and rhabdomyomas (2%).1 Myxomas are predominantly located in the left atrium and are more frequent in females between the fourth and sixth decades of life.2 Their clinical presentation is variable, ranging from weight loss to heart failure and embolisms.3
We present a retrospective, descriptive case series. Our objective was to describe the surgical experience with cardiac myxomas at a tertiary hospital, emphasizing clinical presentation, tumor recurrence, embolic phenomena, complications and surgical outcomes, while also estimating the prevalence of cardiac myxomas in our unit. A hypothesis was made of a possible association between tumor recurrence, embolic phenomena, tumor size and surgical outcomes.
Epidemiology, etiology, and morphologyRight atrial masses are rare, and most of them are benign tumors like myxoma. Overall, myxomas are responsible for almost 80% of intracardiac masses.4
According to the 5th Edition of the WHO Classification of Tumors of the Heart, the most common cardiac tumor is papillary fibroelastoma.5 However, the incidence of benign tumors in Mexico is 0.16%, and myxoma continues to be the most common cardiac tumor (74%).6 Patients are predominantly female (2:1), but this difference disappears after the age of 65 years, possibly because the inhibitory mechanism of myxoma cells stops functioning in males.7
Myxomas are gelatinous friable lesions, ranging from 2 to 11 cm in size. Their surface can be lobular, smooth or villiform, and the villiform type may be associated with thromboembolism.8
Myxomas have a myxoid stroma with hemorrhage and calcification that may demonstrate bone, gland and giant cells. Immunohistochemical testing shows positivity for PRKAR1A and could be useful as a screening tool in Carney complex, which appears in 3%–10% of myxomas.8
Location and clinical manifestationsMyxomas are located on the left side of the interatrial septum in 75%–80% of cases, followed by the posterior atrial wall, anterior atrial wall, and atrial appendage. Right atrial myxoma occurs in 15%–20% of cases and originates at the edge of the fossa ovalis.2
Symptoms are variable and include dyspnea, chest pain and embolism. Up to 30% of patients develop constitutional symptoms. Embolization occurs in 10% of cases of right myxoma, resulting in pulmonary embolism or infarction, the latter in patients with a foramen ovale. The “myxoma triad” is characterized by obstructive symptoms (which mimic mitral stenosis, including dyspnea, orthopnea or syncope), constitutional symptoms and embolic phenomena.9,8
DiagnosisTransthoracic echocardiography is the first-line imaging tool, with a sensitivity of 93%. Differential diagnoses include thrombus, vegetation and calcific lesions.10
Polypoid myxomas have a smooth surface and cystic and hemorrhagic areas, while papillary myxomas have multiple villi and may be associated with embolic phenomena lesions.10
On magnetic resonance imaging, cardiac myxomas may appear with an iso/hypointense or hyperintense signal versus the myocardium in T1 weighted sequences. The absence of intravenous contrast enhancement differentiates an intracavitary thrombus from myxoma.11
Treatment and prognosisSurgical resectionThe treatment of choice is surgical resection. Surgery must be performed promptly due to the possibility of embolism or sudden death. Tumor resection must include the base and wide margins to prevent recurrence.2,8
Different techniques are the left atrial, transseptal atrial, superior transseptal or biatrial approaches, followed by complete removal of the specimen including its implantation site, or by using laser photocoagulation in an area of 1 cm around the pedicle. Even with the above measures, up to 6% of cases present recurrence due to incomplete resection. Resection may result in an atrial septal defect, which is closed with a patch to form a neo-septum. In case of valve damage or adhesion of the tumor to the leaflets, valve repair, annuloplasty or valve replacement with a prosthesis may be required.12
PrognosisSurgical resection is associated with low mortality and excellent long-term outcomes. Reported complications in previous series are paroxysmal atrial fibrillation, surgical site infection, valve replacement; the inpatient mortality rate is 0%.3
In one of the reported series, there was only one recurrence over 5 years following excision.8
Even in high surgical risk patients, for instance patients over the age of 70 years, tumor resection can be curative with successful postoperative evolution.7
MethodsThe objective of the study was to describe the surgical experience from a clinical standpoint, identifying embolic events, tumor recurrence, postoperative outcomes of cardiac myxoma resection and to estimate the prevalence of cardiac myxomas in our unit. As a secondary objective, we analyzed the relationship between tumor size with surgical outcomes and embolic phenomena with tumor recurrence.
This is a descriptive, retrospective, case series. We identified patients diagnosed with cardiac myxoma in the cardiothoracic surgery service from 2014 to 2022 by searching through the clinical records of the surgeries performed during this period.
The mean was used as the central measure and the standard deviation as the measure of dispersion in continuous variables.
We described the population baseline characteristics (age, gender, comorbidities, left ventricle ejection fraction and clinical manifestations) reporting the frequency and percentage.
The surgical event characteristics included the maximum diameter of the specimen, aortic clamping and extracorporeal circulation time, determining the standard deviation, average value, minimum value and maximum value. The postoperative evolution was studied based on the frequency of shock and atrial septal defect, as illustrated in Table 3.
We studied the relationship between the postoperative complications with age, tumor size and the affected cardiac chamber. The r value was determined between surgical times of aortic clamping (AOC) and extracorporeal circulation (ECC) with age and the affected chamber.
The prevalence was estimated based on the number of cardiac surgeries performed in our unit during the 8-year follow-up.
ResultsA total of 31 patients were identified over a period of 8 years, 4 of which were excluded from the study due to incomplete records. One patient died before surgery due to embolism, and 26 underwent surgical resection.
A prevalence of 0.44% was calculated during the 8-year follow-up based on the specific population and the number of surgeries performed in the unit during that period.
Population characteristicsTable 1 specifies the baseline characteristics of the population: 66% of the patients were female (n = 18), and the average age was 54 ± 16 years. The male:female ratio was 1:2. In total, 37% of the patients were healthy previously. The most common comorbidity was systemic arterial hypertension, followed by coronary artery disease and type 2 diabetes mellitus.
Baseline characteristics of the population n = 27 (%).
| Sex | Male | 9 (33) |
| Female | 18 (66) | |
| Age | Average | 54 |
| Standard deviation | 16 | |
| Minimum age | 2 | |
| Maximum age | 77 | |
| Comorbidities | DM type 2 | 6 (22) |
| Systemic arterial hypertension | 10 (37) | |
| Hypothyroidism | 1 (3) | |
| Previous CVE | 2 (7) | |
| Dyslipidemia | 2 (7) | |
| Familial myxomatosis | 0 (0) | |
| Coronary arterial disease | 9 (33) | |
| Affected chamber | Right atrium | 3 (11) |
| Left ventricle | 1 (3) | |
| Left atrium | 23 (85) | |
| Previously healthy patients | 10 (37) | |
| Situation | Septum | 14 (51) |
| OTRV | 1 (3) | |
| Valve | 1 (3) | |
| Atrial ceiling | 9(33) | |
| Foramen ovale | 2 (7) | |
| LVEF (%) | Average | 59% |
| Minimum value | 45% | |
| Maximum value | 78% | |
| Standard deviation | 6.7% | |
| Valvular disease | Frequency | 20 (74) |
| Mitral regurgitation | 11 (40) | |
| Mitral stenosis | 2 (7) | |
| Aortic insufficiency | 1 (3) | |
| Tricuspid regurgitation | 4 (14) | |
| Tricuspid stenosis | 1 (3) | |
| Pericardial effusion | 1 (3) | |
| Asymptomatic | 1 (0) | |
| Clinical manifestations | Dyspnea | 23 (85) |
| Cerebrovascular event | 5 (18) | |
| Acute lung edema | 2 (7) | |
| Extremity embolization | 0 (0) | |
| Pulmonary embolism | 1 (3) | |
| Chest pain | 1 (3) | |
| Syncope | 3 (11) | |
| Palpitations | 5 (18) |
In the case of the 2-year-old patient, the presence of hereditary myxomas, such as in the context of the Carney complex, was ruled out.
Tumor characteristicsThe most affected cardiac chamber was the left atrium (85%). The most common tumor location was in the septum (51%), followed by the roof of the atrium (33%). Most of the population had preserved LVEF, with an average of 59%. More than half of the patients had valve disease (74%, n = 20), the most common of which was mitral valve regurgitation (40%, n = 11).
The main clinical manifestation was dyspnea (85%, n = 23) and cerebrovascular event (CVE) (18%, n = 5). One patient presented 2 strokes, and another presented the event after tumor resection. Only one patient was asymptomatic.
The maximum diameter of the tumor was 100 mm and the minimum 26 mm, with an average of 60 mm. The macroscopic and microscopic descriptions of one of the tumors are shown in Figs. 1 and 2.
The surgical outcomes are described in Tables 2 and 3. Mean aortic clamping time was 26 min ± 45 min. Mean extracorporeal circulation time was 77 ± 23 min. Postoperative evolution was uneventful in most patients (77%, n = 21). The most common complication was cardiogenic shock and prolonged mechanical ventilation, which occurred in 22% (n = 6) of the patients.
Postoperative evolution.
| Postoperative complication | n (%) |
|---|---|
| Iatrogenic atrial septal defect | 1 (3) |
| Cardiogenic shock | 3 (11) |
| Mechanical ventilation | 3 (11) |
| Acute renal injury | 1 (3) |
| More than usual bleeding | 1 (3) |
| Persistent arrhythmia | 1 (3) |
| No complications | 21 (77) |
| Mortality | 2 (7) |
| Recurrence | 2 (7) |
Relationship between postoperative complications with age, tumor size, and the affected cardiac chamber.
| Cardiogenic shock | Prolonged IMV | More than usual bleeding | Recurrence | |
|---|---|---|---|---|
| Average age | 22 years | 22 years | 20 years | 44 years |
| Size average | 65 mm | 65 mm | 30 mm | 47 mm |
| RA location | 33% | 33% | No | No |
| LA location | 66% | 66% | Yes | Yes |
Tumor recurrence occurred in 2 patients (7%), both in the left atrium. Both patients were female, under 60 years of age, with valvular disease (double mitral lesion and tricuspid insufficiency) and had also debuted with CVD. Both had been treated with the transseptal approach. One of the recurrences occurred 4 years after surgery and the other 5 months after the first surgical intervention. One of the patients with recurrence had a torpid course with prolonged IMV and cardiogenic shock, and the other recurrence had a benign course without complications. One patient presented an iatrogenic atrial septal defect. Both biopsies were reanalyzed, but no tumor was found in the resection margins.
Among the identified patients, 2 died over the 8 years studied: one before the surgical intervention (diagnosis of myxoma had been made clinically and echocardiographically), and the other after the second procedure due to recurrence, confirmed by biopsy.
The average tumor size found in patients who presented tumor recurrence was 47 mm, specifically 70 mm in patients who presented arrhythmias and 65 mm in patients with cardiogenic shock and prolonged invasive mechanical ventilation (IMV) (Table 4).
The AOC average time in RA was 50 min, in LA 23 min, and in LV 60 min. The ECC average time was 54 min for RA, 75 min for LA, and 87 min for LV. The r values for AOC and ECC surgical times concerning age were 0.4 and 0.43, respectively (Table 4).
DiscussionThe most common cardiac tumor in our country continues to be myxoma, unlike the most recent classification of cardiac tumors by the WHO, which lists aortic fibroelastoma as the most common cardiac tumor.5
The incidence of atrial myxomas reported in Mexico at other medical centers is 0.16%.13 Since our study is a descriptive, retrospective, case series and not a prospective one, the incidence could not be estimated. Instead, we estimated the prevalence, based on the number of cardiac surgeries performed in our unit in 8 years (0.44%).
Four tumor resections are performed per year at our hospital. In the 8 years studied, 93% of cardiac tumor resections were cardiac myxomas; the remainder were papillary fibroelastoma and one metastatic tumor.
Approximately 75%–80% of myxomas originate on the left side of the interatrial septum, which coincides with our data (85% in LA and 51% in the interatrial septum).
The study population was made up mainly of women in their fifth decade of life, whose main comorbidity was hypertension (37%).
As in previous studies,14 the male:female ratio was 1:2. The reported age range of 40–60 years corresponded to the average age of 54 years, however there was a significant standard deviation due to a 2-year-old patient. This coincides with other series were women represented 80% of the population, with a median age of 59 years.15
The most common symptom was dyspnea, as in previous reviews.15 The rate of embolic phenomena is striking (second most common manifestation, CVD in 18%, n = 5), which was related to the severity of the disease since the 2 recurrences found debuted with embolic phenomena.
Mitral regurgitation was the most common valve disease. Tricuspid stenosis is rare and is considered due to functional stenosis of the valve because of increased right atrial pressure, which occurred in one patient.
The surgical approach performed was atriotomy and pedicle resection, and the interatrial septum was preserved. The surgical risk was low in all our patients, except in the patient who presented recurrence 5 months after the first intervention.
The complications of prolonged mechanical ventilation and bleeding greater than usual were found in the youngest patients, with an average age of 22 years.
The reported mortality is 0% in some series,3 which is much lower compared to the rate reported in our series (3.2%).
A 10%–15% chance of recurrence is reported in nonfamilial myxomas in a period of 4 years,3 which is unlike the present study, where it was found in 7% of the population. The slides of both recurrences were analyzed, finding no evidence of residual tumor. In the histological analysis, the only difference found was a higher concentration of inflammatory infiltrate and areas of hemorrhage, with a myxoid matrix of similar characteristics.
Although the sample size is small, it calls attention to the 2 recurrences in our follow up, as larger series of 41 patients with 15 years of follow up in other countries report no recurrences.15
Tumor size was not associated with postoperative complications or recurrence.
In the series of 23 myxomas at a hospital in Morocco over 25 years,16 the average age was lower than in our series, the female:male ratio was higher (2.28), and one recurrence was reported in which the patient died due mediastinitis.
In a private hospital in Spain, a similar proportion of embolic events was reported compared to our study (14% and 18%, respectively). The incidence of embolism was 30%–45% in LA myxomas, 65% in LV myxomas, and 10% in right myxomas, and up to 50% involved the CNS.15
In another series from Argentina,17 the most common clinical presentation was constitutional symptoms (unlike the present study), followed by dyspnea. Hospital mortality was 3.2%, which coincides with the present study.
One of the strengths of the study is the analysis of surgical outcomes in terms of location, size, and demographic variables, such as age and the possible relationship between tumor recurrence and embolic manifestations, not tumor size. The sample size has been a limitation, and further studies are required to confirm these associations.
More studies are required to describe the position of papillary fibroelastoma, which is reported internationally as the most common cardiac tumor.
ConclusionsIn the Northeast of the country, 4 atrial myxoma resections are performed per year. Since the general incidence of benign tumors reported in our country is 0.16%, similar to other series, the present study is the second-largest case series of cardiac myxomas, excluding other benign cardiac tumors. The estimated prevalence was 0.44%, based on the number of cardiac surgeries performed in 8 years.
As in the previous series presented, the prognosis for recurrence is serious.
There was no correlation between tumor size and surgical outcomes.
Although the sample size is limited to make a strong association between the severity of embolic phenomena and tumor recurrence, this cannot be rule out either. Recurrences of cardiac myxomas, how they develop, and surgical methods to prevent them suggest a path for further investigation.
Although, no data for tumor recurrence were found in the histological analysis, wide surgical resection of the pedicle and the base of tumor implantation may influence tumor recurrence. Further studies are necessary to expand the analysis, including other hospitals and all type of cardiac tumors.
Conflict of interest and funding sourcesThe authors have no conflicts of interest to declare. This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.