The Spanish Association of Coloproctology and the Coloproctology Division of the Spanish Association of Surgeons propose this consensus document with a treatment algorithm for anal fissure that could be used for decision making. Non-surgical therapy and surgical treatment of anal fissure are explained, and the recommended algorithm is provided. The methodology used was: creation of a group of experts; search in PubMed, MEDLINE and the Cochrane Library for publications from the last 10 years about anal fissure; presentation at the 21st National Meeting of the Spanish Association of Coloproctology Foundation 2017 with voting for/against each conclusion by the attendees and review by the scientific committee of the Spanish Association of Coloproctology.
Desde la Asociación Española de Coloproctología y la Sección de Coloproctología de la Asociación Española de Cirujanos se propone un documento de consenso sobre el algoritmo de actuación en el tratamiento de la fisura anal que pueda ser de utilidad en la toma de decisiones. En él se expone la actualidad en el tratamiento conservador, médico y quirúrgico, finalizando con un algoritmo de recomendación ante una fisura anal. La metodología utilizada ha sido: creación de un grupo de expertos, búsqueda en PubMed, MEDLINE y Biblioteca Cochrane de las publicaciones de los últimos 10 años sobre fisura anal, presentación en la XXI Reunión Nacional de la Fundación Asociación Española de Coloproctología 2017 con votación de cada conclusión entre los asistentes, y revisión por el comité científico de la Asociación Española de Coloproctología.
Anal fissure (AF) is one of the most frequent reasons for consultation in surgery departments. There is ample experience and scientific evidence in order for surgeons to follow well-defined patterns. In spite of this, in daily clinical practice there is a certain controversy regarding therapeutic algorithms for anal fissure.1,2
Therefore, we believe that it would be useful for the Spanish Association of Coloproctology (Asociación Española de Coloproctología, AECP) and the Coloproctology Division of the Spanish Association of Surgeons (Sección de Coloproctología de la Asociación Española de Cirujanos) to propose a therapeutic algorithm based on evidence and consensus in an attempt at creating a position paper to aid in decision-making.
We presented the review of these paradigms and therapeutic algorithm for AF at the National Symposium of the AECP, held in May, 2017.
MethodsThe methodology used in the creation of the consensus document was the following:
- •
A work group was organized, including 4 specialized surgeons, 3 experts in coloproctology and a work group coordinator.
- •
The consensus document was divided into 4 areas of interest regarding AF: hygiene-dietary treatment/conservative measures, medical treatment, surgical treatment and algorithms of the scientific societies, with a final consensus algorithm proposed by the AECP.
- •
PubMed, MEDLINE and Cochrane Library databases were searched for publications from the last 10 years using the keywords: anal fissure, treatment.
- •
In May 2017, the 21st National Meeting of the AECP Foundation was held in Almería, Spain. In round table discussions, 4 surgeons presented the bibliographic review of each area of interest and closed the table with conclusions based on the scientific evidence and the opinion of the experts. Each conclusion was voted on (agree/disagree) by the attendees.
- •
After the meeting, the first document was drawn up, including this information, all the evidence obtained in the bibliographic search and the opinion of the experts. All evidence and recommendations have been classified in accordance with the Centre for Evidence-Based Medicine (Oxford, England).
- •
The document has been evaluated by the scientific committee of the AECP, as well as by the experts of the work group. After the modifications made based on their opinions, the final document was completed.
AF is a painful lesion of the anal region that presents as a linear ulcer that can extend from the pectineal line to the anal margin. It is usually located in the posterior raphe and is accompanied with very notable symptoms of proctalgia that often affect the patient's quality of life. The condition is considered acute when its progression is quick, its treatment requires no more than hygiene-dietary measures and, normally, its duration is no more than 6–8 weeks. Once this time has elapsed, the fissure is considered chronic (CAF); additional factors that establish the diagnosis include the evolution time, persistence of symptoms and other signs, such as evidence of a sentinel papilla during examination or the visualization of fibers of the internal sphincter.1,2
In the presence of atypical symptoms or examination findings, other pathological processes must be ruled out, and complementary studies (colonoscopy, biopsy, etc.) must be conducted before starting treatment. Once the diagnosis is established, there are several therapeutic options to be assessed, as discussed below.
Hygiene and Dietary Treatment; Conservative MeasuresThe conservative treatment of AF is contemplated as an initial therapeutic step, both in the acute and chronic phases of this process.3
As stated in the recommendations of the clinical practice guidelines of the American Society of Colon and Rectal Surgeons, this “basic” step is safe, has few side effects, and should be the first line of treatment (Strong recommendation, Level of evidence IB).4
Treatment aims to reduce anal muscle tone as an initial measure. To this end, in addition to the usual healthcare recommendations (abstaining from smoking, moderate physical exercise, proper rest) and the application of sitz baths with warm water, it is necessary to avoid constipation. Therefore, the consumption of liquids should be increased, the diet should be rich in fiber, and stool softeners should be used.5
These conservative measures by themselves can cure AF and prevent recurrences.6,7
Increased Intake of Dietary FiberDietary fiber is the edible part of plants or similar carbohydrates that is resistant to the hydrolysis of human digestive enzymes, which prevents its absorption and leads to its fermentation in the large intestine.
Soluble fiber is easily fermentable and able to retain water in the upper digestive tract, obtaining a viscous gel-like mixture. This fiber group includes guar gum, mucilage, soy polysaccharides, inulin, pectin and oligosaccharides, which are present in vegetables, fruits and vegetables, barley and oats.8
Insoluble fiber has a greater effect on the final retention of water in its transit through the colon, diluting the intestinal waste and acting as a substrate for the gut flora, which contributes to increase fecal volume. Lignin and cellulose are found in wheat bran, rye, whole grains, rice by-products, lettuce, escarole, broccoli, green beans, apples and fruit skin.8
Stool SoftenersThese are dietary compounds that contribute to the production of a bulkier and softer fecal mass. The most common are Psyllium or Plantago ovata (rich in mucilage and soluble hemicellulose), methylcellulose and oral soluble and insoluble fiber supplements (wheat bran, guar gum, pectin, plum).
Sitz BathsTheir use has traditionally been suggested in order to reduce the anal sphincter tone and reduce pain.9,10
Currently, all consensus documents for the treatment of AF include using sitz baths because, although the evidence is weak, its use entails few adverse effects, improves the hygiene of the area and produces relief of symptoms in some patients.11,12
Evidence- 1.
A diet rich in fiber is recommended in the acute phase of AF, providing 25–30g/day.
- 2.
Maintained fiber intake is recommended to prevent recurrences of AF.
- 3.
Fiber supplements (non-laxative) are recommended as a conservative treatment of AF.
- 4.
Sitz baths with warm water (36–40°C) for 10min are recommended.
- 5.
Sitz baths are recommended twice a day and after each bowel movement.
- 6.
Adding other substances to the bath has not been demonstrated to be beneficial, so this recommendation is left to the criteria of the specialist.
Medical or pharmacological treatment should be aimed at achieving transitory relaxation of the internal anal sphincter, thereby resolving hypertonia and improving the vascularization of the mucosa of this area, but with the subsequent recovery of the normal baseline tone, thereby avoiding the risk of incontinence.
There are several drugs, such as calcium channel blockers (CA), captopril and diltiazem mainly, nitric oxide donors (glyceryl trinitrate [GTN]) and botulinum toxin (BT).
The latest Cochrane review13 conducted an analysis of the pharmacological treatment of AF, including 75 randomized clinical trials up to August 2010. The efficacy and morbidity of 17 different treatments for AF were assessed, among these GTN, isosorbide dinitrate, diltiazem, nifedipine and BT, as well as surgical sphincterotomy. These authors conclude that the medical treatment of AF, usually based on GTN, BT or CA, in both acute and chronic fissures and fissures in children, can be applied with higher cure rates than placebo (hygiene-dietary measures). In addition, they indicate that, in CAF in adults, any of these treatments is very far from the effectiveness of surgery. On the other hand, the risk of using these treatments is not great, except for headache secondary to treatment with oral GTN or CA, with no long-term adverse effects. GTN reaches a cure rate of 48.9%, with recurrences around 50%–60% in the long term. CA achieve similar cure rates, with no follow-up studies of more than one year. There are several studies on BT with variable doses (10–100IU) and diverse sites of application (in the internal anal sphincter, intersphinteric, on both sides, etc.), with cure rates of up to 67.5%.
The therapeutic algorithm for AF, published in 2016 in UpToDate,14 begins with hygiene-dietary measures and pharmacological support. The recommendations that are established are: support measures (fiber, stool softeners, sitz baths, topical analgesia); topical vasodilators (nifedipine or nitroglycerin) for one month, instead of surgery (Grade of recommendation 1B). They recommend using 0.2%–0.3% nifedipine (pharmaceutical compound) instead of nitroglycerin as a topical vasodilator. Nifedipine has fewer side effects and drug interactions than nitroglycerin and may be more effective (Grade of recommendation 2B). If the pharmaceutical compound were not available, commercial 0.4% nitroglycerin could be administered. In patients with typical AF, who do not respond after 8 weeks of initial medical treatment, BT injection or lateral internal sphincterotomy (LIS) are recommended (Grade of recommendation 2C). The authors conclude that, although medical treatment is less effective than surgical treatment, it should be offered due to its wide availability, good tolerance and absence of serious complications.
The publication of the American Society of Colon and Rectal Surgeons4 concludes that the medical treatment of AF is safe, has few side effects and should be the first-line treatment (Grade of recommendation 1B). AF can be treated with topical nitrates, although the side effects may limit its efficacy (Grade of recommendation 1A). CA have a similar effect in AF as topical nitrates but fewer side effects and can be used as a first-line treatment (Grade of recommendation 1A). BT has similar results for healing as other topical therapies as first-line treatment in AF and slightly better in terms of healing rates as a second-line therapy after topical treatment (Grade of recommendation 1C). LIS is associated with clearly higher CAF healing rates compared to medical therapy and, therefore, may be offered in selected patients, even if drug treatment failure has not been confirmed (Grade of recommendation 1B).
In a recent study published in the British Medical Journal,15 different medical treatments were compared to LIS, which was observed to be more effective than nitric oxide donors (glyceryl trinitrate and isosorbide mononitrate) in the healing of AF between 6 weeks and 2 years (High level of evidence). In addition, surgery reduced the time to complete pain control versus nitric oxide donors (Low level of evidence). LIS is more effective than BT in curing AF between 18 weeks and 3 years (High level of evidence). Gas leaks or mild incontinence occur in 9% of patients treated with LIS versus 0/166 (0%) with BT.
There are very few studies with long-term follow-up of BT therapy. Several authors16–18 have observed recurrence rates of 40%–50% after a follow-up period of more than 3 years.
Evidence- 1.
Medical treatment of acute fissures is safe, has few side effects and should be the first-line treatment (Grade of recommendation 1).
- 2.
CA have a similar effect on CAF as topical nitrates, but fewer side effects, and can be used as a first-line treatment (Grade of recommendation 1A).
- 3.
BT has similar results for healing as other topical therapies as a first-line treatment in CAF and slightly better in terms of healing rates as a second-line option after topical treatment (Grade of recommendation 1C).
- 4.
LIS is associated with clearly superior CAF healing rates compared to medical treatment.
The unacceptable risk of incontinence and inferiority as a technique compared to LIS have made it obsolete and no longer used.19,20
Derived from this technique, a new interest has arisen due to the development of calibrated and controlled procedures with anal dilators or pneumatic balloons. The healing rate of this “controlled” dilation is similar to that of sphincterotomy, but with a much lower rate of incontinence.21,22
Lateral Internal SphincterotomyThe objective of this procedure is to reduce sphincter tone through the division of the internal anal sphincter with direct vision (open technique) or guided by the finger (closed technique) below the pectineal line, finding no significant differences between the two.23,24 Healing rates vary from 92% to 100%, while early and late incontinence rates are 3.3% to 16%.15
Before deciding on a more “aggressive” approach, morphological (endoanal ultrasound) and functional (anorectal manometry) diagnostic techniques of the anorectal complex can be considered. In women, the division of the internal anal sphincter tends to be more extensive than expected, which is probably related to the shorter anal canal in women versus men. Age, childbirth, previous obstetric trauma, previous anorectal surgery (hemorrhoidectomy, fistulectomy or fistulotomy, anal dilatation or LIS) and previous sphincterotomy may further compromise sphincter function. Undetected sphincter anomalies should be suspected in patients with incontinence and a correct LIS technique. For persistent symptoms/pain after surgery, ultrasound can evaluate the anatomical result of LIS and classify it as complete or incomplete, and assess its radial and longitudinal extension.25,26
Therefore, careful patient selection, absence of preoperative continence problems and meticulous surgical technique are necessary to achieve good results. It is noteworthy that the current trend is to perform the “adapted” sphincterotomy technique (the length of the fissure and not to the dentate line as originally) and laterally, avoiding doing so on the posterior side (key-hole deformity) to minimize the rate of incontinence.
Advancement-Flap AnoplastyThis technique involves curettage of the area and creating a local flap of skin and subcutaneous cellular tissue with a thickness of 1cm, which covers the defect of the fissure beyond its outer edge and is sutured to the rectal mucosa. Possible complications include necrosis, dehiscence and infection. The indications for this technique are the risk of incontinence (age, multiple childbirths, obstetric trauma, anorectal surgery) and the persistence of symptoms after conservative therapies or sphincterotomy.27
The studies by Giordano et al. and Chambers et al. did not find significant differences in the cure rates (98% advancement-flap anoplasty versus 100% LIS), with a lower risk of incontinence (0%–3.3%) and a lower rate of complications (dehiscence 5.9%) compared to LIS.28,29
FissurectomyThis consists of a curettage of the fissure to allow for its healing. Barnes et al. studied the combination with high doses of BT and achieved a cure rate of 93% and temporary gas incontinence of 7%. It can be considered a second-line therapy for CAF that is not cured with the use of topical therapy, or even as a first-line therapy for patients who have signs of chronic disease.30
FissurotomyThe presence of a subcutaneous tract can make the fissure persist due to repeated infections. This technique allows for the cicatrization of the path, release of the perianal skin, as well as the widening of the anal canal, making sphincterotomy unnecessary. Incontinence is eliminated with a cure rate of 98.2%.31
Therapies Under EvaluationThe transplantation of autogenous hypogastrium adipose tissue promotes the healing of lesions associated with local ischemia and improves the elasticity of the scar tissue in cases of associated anal stenosis. It is easy to perform, safe, well tolerated and repeatable. The pilot study by Lolli, with a small number of cases and a relatively short follow-up, is worth mentioning. It may represent a promising approach for difficult-to-treat chronic anal fissures, especially in association with anal stenosis, but the technique requires further verification before its possible application.32
Posterior sacral/tibial stimulation, through parasympathetic activation, leads to relaxation of the internal anal sphincter with a positive effect on spasm, which subsequently improves ischemia. Another mechanism of action could be the greater blood flow of the rectal mucosa. It can be an effective method for the treatment of CAF, with rapid relief of symptoms and healing, without complications, in patients who choose not to undergo an invasive procedure with high comorbidity, recurrent fissures and side effects of medical treatment, as shown by some studies.33 However, the results must be verified in larger controlled series.
Sphincterolysis involves firm pressure with the fingers in the left-lateral intersphincter space, on the internal anal sphincter, to divide (by fracturing the fibers) the thickness without breaking the anal mucosa. It seems to be an effective, safe and easy procedure, with a cure rate of 97% and temporary incontinence of 3.5%, which resolved itself in 97% of the patients within one month.34
As a conclusion, a meta-analysis was recently published,35 where LIS was the most effective treatment option (93.1%) in CAF (Level of evidence 1A). However, 9.4% of patients suffered postoperative incontinence. Other treatment options, such as advancement flap anoplasty and/or fissurectomy, were less effective but safer, with a cure rate of almost 80% and a risk of incontinence of 4.9%.
We can establish, with a Level of evidence 1A and a Grade of recommendation A: Evidence: surgical treatment is the second therapeutic step for CAF.
Evidence: surgery is the most effective long-term treatment for CAF.
Evidence: surgery may be indicated, as the first therapeutic step, in young patients with severe untreatable acute proctalgia who accept the risk of fecal incontinence.
Evidence: LIS continues to be the surgical technique of choice.
Evidence: LIS is the technique of choice in patients with rejection, failure or complications after pharmacological therapy.
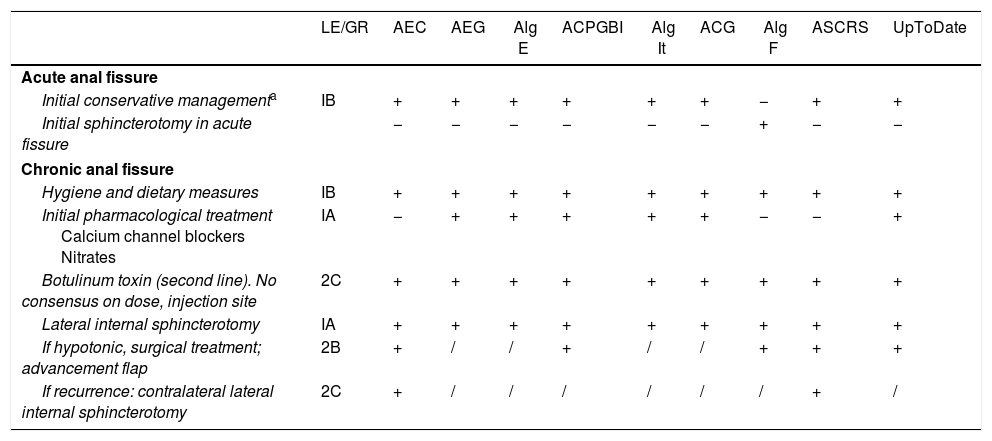
Algorithms by the Scientific SocietiesThe treatment of AF has been the frequent subject of discussion by various scientific societies. Despite having a common general tendency for management, there are discrepancies, which are shown in Table 1.
Management of Anal Fissure According to Different Scientific Societies.
| LE/GR | AEC | AEG | Alg E | ACPGBI | Alg It | ACG | Alg F | ASCRS | UpToDate | |
|---|---|---|---|---|---|---|---|---|---|---|
| Acute anal fissure | ||||||||||
| Initial conservative managementa | IB | + | + | + | + | + | + | − | + | + |
| Initial sphincterotomy in acute fissure | − | − | − | − | − | − | + | − | − | |
| Chronic anal fissure | ||||||||||
| Hygiene and dietary measures | IB | + | + | + | + | + | + | + | + | + |
| Initial pharmacological treatment Calcium channel blockers Nitrates | IA | − | + | + | + | + | + | − | − | + |
| Botulinum toxin (second line). No consensus on dose, injection site | 2C | + | + | + | + | + | + | + | + | + |
| Lateral internal sphincterotomy | IA | + | + | + | + | + | + | + | + | + |
| If hypotonic, surgical treatment; advancement flap | 2B | + | / | / | + | / | / | + | + | + |
| If recurrence: contralateral lateral internal sphincterotomy | 2C | + | / | / | / | / | / | / | + | / |
ACG: algorithm of the American College of Gastroenterology5; ACPGBI: algorithm of the Coloproctology Association of Great Britain and Ireland3; AEC: algorithm of the Spanish Association of Surgeons36; AEG: algorithm of the Spanish Association of Gastroenterology37; Alg E: algorithm of the European consensus38; Alg F: algorithm of the French group40; Alg It: algorithm of the Italian group39; ASCRS: algorithm of the American Society of Colon and Rectal Surgeons4; LE/GR: level of evidence/grade of recommendation; UpToDate: algorithm published in UpToDate.14
There are several points of consensus among the published guidelines. With regard to the management of acute fissure, all of them recommend a conservative approach, with the exception of the French algorithm, which contemplates using LIS in cases of poor pain control.
Regarding CAF, there is a general consensus about the use of first-line pharmacological treatment (chemical sphincterotomy). However, some guidelines, such as that of the European Gastroenterology Association, the American Society of Colon and Rectal Surgeons and the French algorithm contemplate LIS as an initial possibility in patients with no risk of incontinence. In general, preference is shown for the use of topical diltiazem over GTN or BT, due to a lower rate of side effects. After reviewing recommendations about BT, there is no consensus regarding dose, injection site or interval between doses. The use of these drugs is subject to their availability in each country. Surgical treatment (except in the mentioned guidelines) would be reserved for patients in whom pharmacological treatment has failed, and LIS would be the gold standard. The different algorithms also contemplated other options, such as the mucous advancement flap or controlled pneumatic dilation.
If symptoms persist despite treatment, further studies will be required to rule out other etiologies, such as Crohn's disease, HIV or neoplasms.
Regarding the evidence reviewed, we can conclude:
- 1.
Management of acute fissure should be conservative.
- 2.
For the pharmacological treatment of CAF, CA is recommended over GTN.
- 3.
LIS is the gold standard when surgical treatment is required.
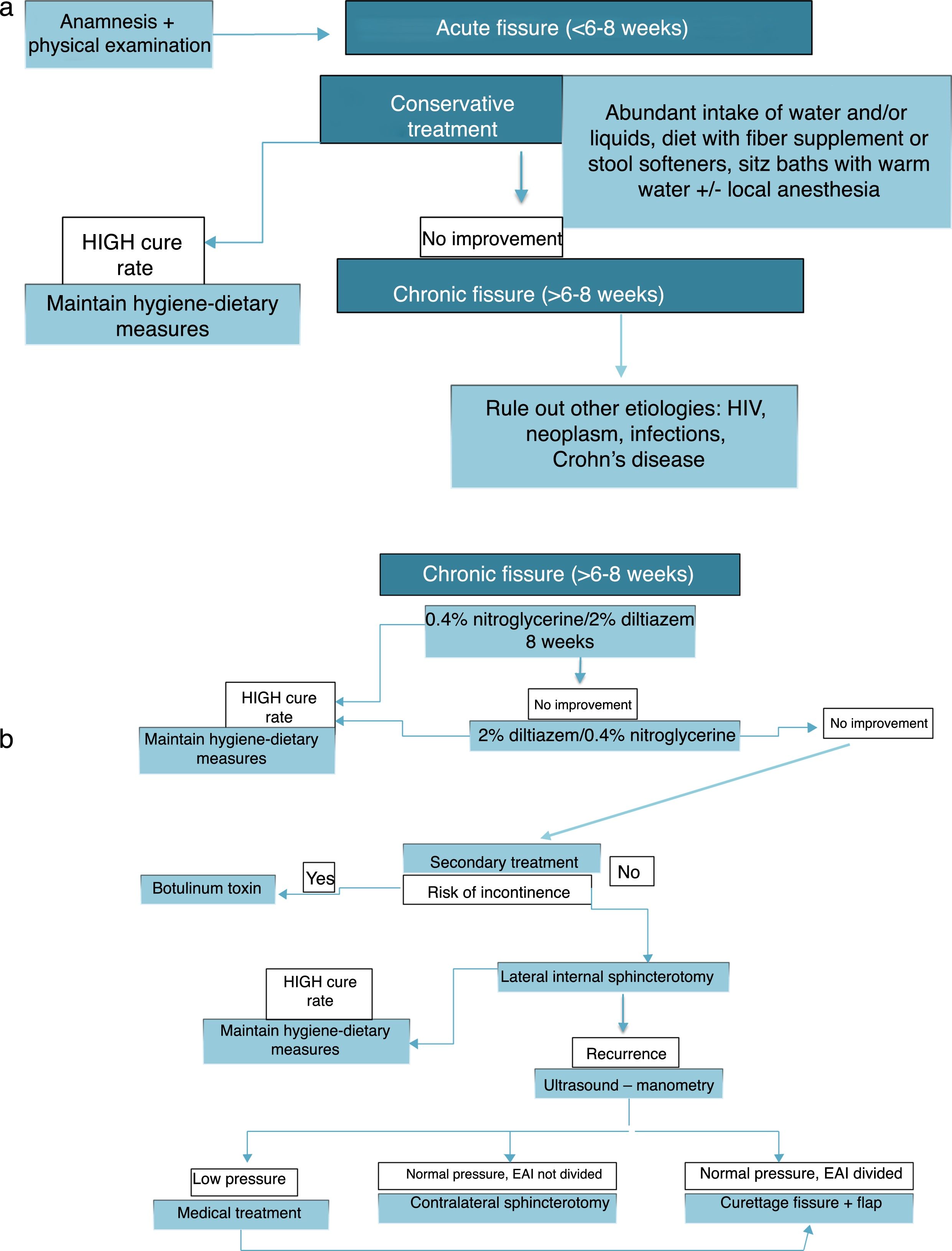
The agreed algorithm, after including the reviewed evidence from the bibliographic search, assessments and contributions by the members of the expert panel, as well as the surgeons in attendance, is shown in Fig. 1.
Conflict of InterestsThe authors have no conflict of interests to declare
Please cite this article as: Arroyo A, Montes E, Calderón T, Blesa I, Elía M, Salgado G, et al. Tratamiento de la fisura anal: algoritmo de actuación. Documento de consenso de la Asociación Española de Coloproctología y la Sección de Coloproctología de la Asociación Española de Cirujanos. Cir Esp. 2018;96:260–267.