Two-stage liver resection with portal ligation or embolization makes it possible to perform R0 resection in patients with liver metastasis from colorectal cancer and insufficient residual liver volume (RLV).1 In recent years, the ALPPS technique (associating liver partition and portal vein ligation for staged hepatectomy) and its variations have been developed to achieve greater and faster hypertrophy of the liver remnant, which allows the second surgical stage to be done earlier, thus avoiding the progression of the disease during the interval.2–5 Nonetheless, this technique presents morbidity and mortality that are higher than two-stage surgery.1,6,7 We present another alternative for R0 resection in patients with advanced liver disease, high tumour load in segment IV and very small RLV. It involves performing right hepatic trisectionectomy in two stages, with portal vein embolization during the interval.
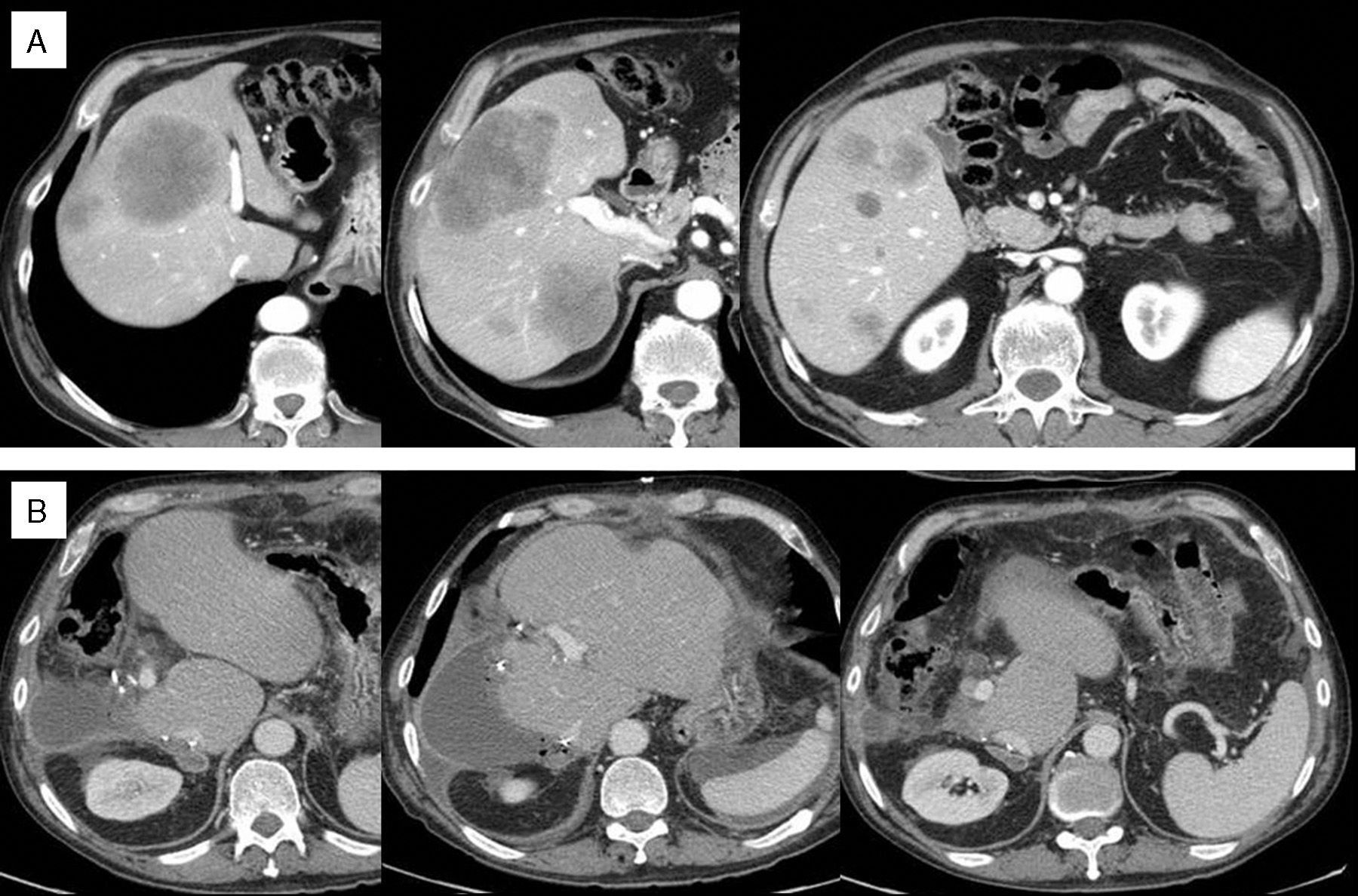
The patient is a 68-year-old male with adenocarcinoma of the splenic flexure that was non-stenosing and showed no signs of bleeding. Multiple potentially resectable bilobar liver metastases were observed. Initial CEA was 344, K-ras mutation. Fig. 1A shows the images of the initial CT scan. After 10 cycles of FOLFOX/bevacizumab and no RECIST response, we observed a morphologic response and contemplated the possibility of surgical resection. The RLV for R0 resection was 18% (240cc, weight 80kg). Portal vein embolization of segment IV was not possible due to the large metastasis in this segment that cut off the portal branches, impeding coil placement. We considered the ALPPS technique, but we thought that the risk of complications was high in segment IV due to the elevated tumour load and the risk of liver failure due to the small residual volume. We therefore decided to perform the following technique:
(A) Initial CT scan: multiple metastases measuring 1–10cm in the right segments and segment IV, one metastasis in segment II and 2 in segment III (superficial, 0.5–1cm) and segment I is disease free; non-specific lung nodule, 0.5cm; (B) post-operative CT scan: absence of liver disease.
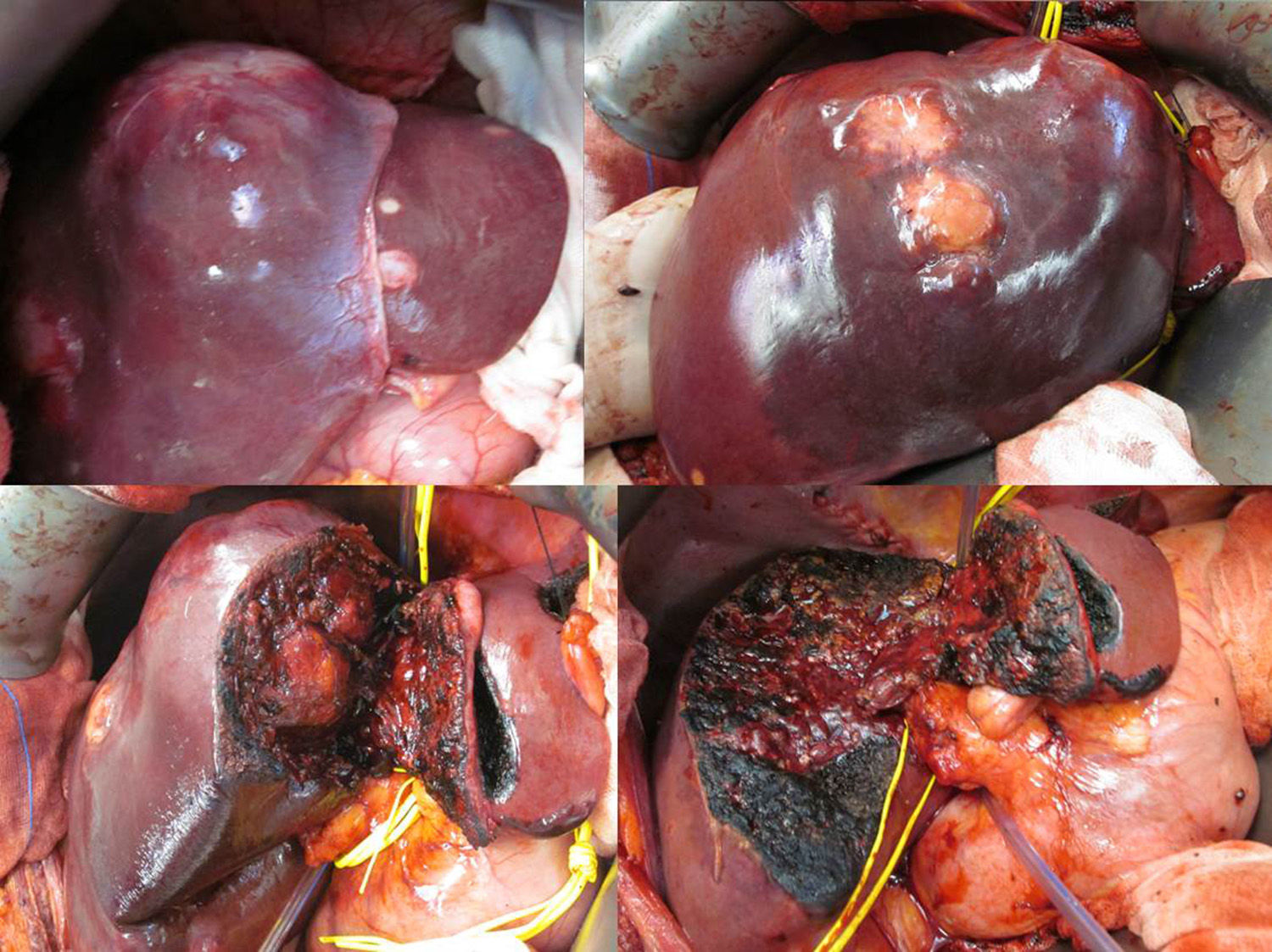
We first began with non-anatomical resection of the 3 metastases described in segments II and III. We then performed standard mesohepatectomy (segments IVa+b, V and VIII), which involved: intra-Glissonian ligation of the portal-biliary branches of segment IV; liver parenchyma dissection on the sagittal plane between the left lateral and medial segments up to the precaval plane; intraparenchymal dissection and ligation of the portal-biliary branches and artery of the right anterior segments; extra-Glissonian isolation of the right posterior pedicle, which was marked with a vascular band for the second intervention; dissection of the parenchyma in the sagittal plane between the right anterior and posterior segments up to the precaval plane; ligation and dissection of the middle hepatic vein (MHV); dissection of right MHV, marked with a vascular band. The postoperative period was uneventful and with no evidence of liver failure (bilirubin [mg/dl] and prothrombin activity [%] on the 1st, 3rd, 5th and 7th days post-op: 1/72, 1/79, 0.7/88 and 0.7/86, respectively). The patient was discharged with no symptoms on the 7th day post-op (Fig. 2).
Three weeks later, RLV (segments I–III) was 26% (382cc). CT scan showed growth of right residual metastases and slight growth of the lung nodule, with no disease at other locations. Right portal vein embolization was carried out (posterior segments), reaching an RLV of 33% (504cc) 4 weeks after embolization (hypertrophy 110% of initial volume). Three cycles of systemic chemotherapy were planned (5-FU and levamisol) during the interval. At the time of the second cycle, however, the patient presented febrile neutropenia, so the third cycle was not administered, and the second stage of surgery was delayed.
Second Stage of Surgery (9 Weeks After the First)The primary tumour was observed in the splenic flexure, with no metastasis in segments I–III. We performed oncologic left hemicolectomy followed by resection of the remaining right liver lobe (posterior segments). To do so, the vascular bands were easily identified on the right MHV and right pedicle. The right pedicle was occluded en bloc with a linear stapler, followed by dissection with a linear endostapler. Right MHV was dissected with the linear endostapler. In the postoperative period, the patient presented mild liver dysfunction: bilirubin (mg/dl) and prothrombin activity (%) on the 1st, 3rd, 5th and 7th days post-op: 1.7/47, 1.3/55, 1.5/62 and 1.3/64, respectively; and ascites that responded to diuretic treatment. The patient was discharged on the 9th day post-op.
Post-surgery reevaluation CT scan showed an absence of liver metastasis (Fig. 1B), a 1cm pulmonary nodule and another 2 new subpleural millimetric nodules. Treatment was reinitiated with systemic chemotherapy, although the disease progressed in spite of the different lines of treatment.
The 2 techniques that are currently available for R0 resection in cases such as the one we present are hepatectomy in 2 stages with embolization of the right portal vein and segment IV (with or without chemotherapy in the interval) or ALPPS.1 In cases with large tumour volume in segment IV, percutaneous embolization can be impossible or entail great risk of accidentally embolizing the branches of segments II and III. Isolated embolization of the right portal vein is not a valid option as it would lead to growth of the metastases of segment IV during the interval. ALLPS is an alternative in these cases that has been shown to achieve important and rapid increases in RLV and, therefore, R0 resection in a very short period of time, while avoiding disease progression. Nevertheless, to date, the morbidity and mortality of this technique are superior, especially with regard to biliary, septic and liver failure complications.6–8 We believe that, with the technique that we describe, the resection of segment IV avoids the complications related with cholangitis, necrosis or sepsis of this segment reported with the ALPPS technique.2,5,6,8 On the other hand, this approach is a way to “condition” the liver remnant. Mesohepatectomy causes an increase in portal flow to segments I–III, as well as the flow through the left MHV. Right portal ligation could trigger liver failure, so it is delayed until a later time. Mesohepatectomy, performed as described above, involves an in situ partition that disconnects the right liver from the left, so right portal embolization leads to a hypertrophy of the liver remnant that is greater and faster than with preoperative embolization, as in the ALPPS technique. In contrast, however, the increase in portal flow is not as abrupt because it had already increased after mesohepatectomy, and the drainage through left MHV should be greater. This situation conditions a lower risk for liver failure. We do not know how much time is required to achieve this “conditioning”, and we waited 21 days before embolization. It is likely that future experimental studies will provide data that will enable us to shorten this interval.9
We believe that this technique may allow for R0 resection in cases like the one we have described, with a very low risk for liver failure, although with a higher risk for progression than with ALLPS. Its application will be necessary in more cases in order to determine its true utility.
Please cite this article as: Alonso Casado O, González Moreno S, Encinas García S, Rubio González E, Ortega Pérez G. Triseccionectomía hepática derecha en 2 tiempos con embolización portal en el intervalo: otra alternativa en enfermedad hepática avanzada con volumen tumoral grande en segmento IV y volumen residual muy bajo. Cir Esp. 2015;93:253–256.