Since the introduction of laparoscopic cholecystectomy, there has been an increase in the incidence and severity of iatrogenic lesions of hepatic pedicle elements. In open surgery the rate is 0.1% and 0.3%–0.6% in laparoscopic surgery.1
These lesions are classified as biliary or vascular. Biliary tract lesions are the most common and 47% can be associated with vascular lesions, mainly of the right hepatic artery, common hepatic artery or portal vein.2–5 Surgical reconstruction of the bile duct and a conservative approach to arterial lesions are usually possible, and the management of these situations is widely reported in several publications. In cases of hepatic ischemia with atrophy of the parenchyma and sepsis, hepatic resection is the treatment of choice. Orthotopic liver transplantation (OLT) is used in exceptional cases, when the vascular and biliary lesions are irreparable,1,5–7 or later in cases of terminal-phase secondary biliary cirrhosis.
We present the case of a patient who underwent elective surgery for cholelithiasis at another hospital. Laparoscopic cholecystectomy was performed, and following the inadvertent complete resection of the hepatic pedicle, emergency OLT was required.
A 58-year-old patient with no prior medical history presented symptomatic cholelithiasis and an episode of acute cholecystitis. He had been treated conservatively and he underwent elective laparoscopic cholecystectomy on August 16, 2012.
During surgery, according to the report, there was heavy bleeding that was resolved with the placement of multiple clips at the sites of the hemorrhage, without the need for conversion. After 24h, follow-up lab work showed significant changes in coagulation and a marked increase in the pattern of cytolysis. Therefore, due to suspected hepatic ischemia, the patient was referred to our hospital.
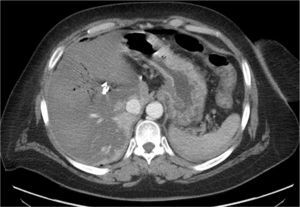
On August 17th, upon admission the patient was afebrile and hemodynamically stable. The work-up showed: bilirubin 50μmol/L (0–18μmol/L), ALT 100.6μkat/L (0–0.63μkat/L), AST 174μkat/L (0–0.5μkat/L), TP 2.4 (0.8–1.2). CT showed a multitude of hemoclips in the hepatic pedicle, with complete occlusion of vascular structures of the hepatic hilum and generalized liver hypoperfusion (Fig. 1). Likewise, we observed acute thrombosis of the portomesenteric venous confluence with partial extension to the splenic vein and superior mesenteric vein. Given the extension and severity the injury, the patient was considered a candidate for emergency OLT.
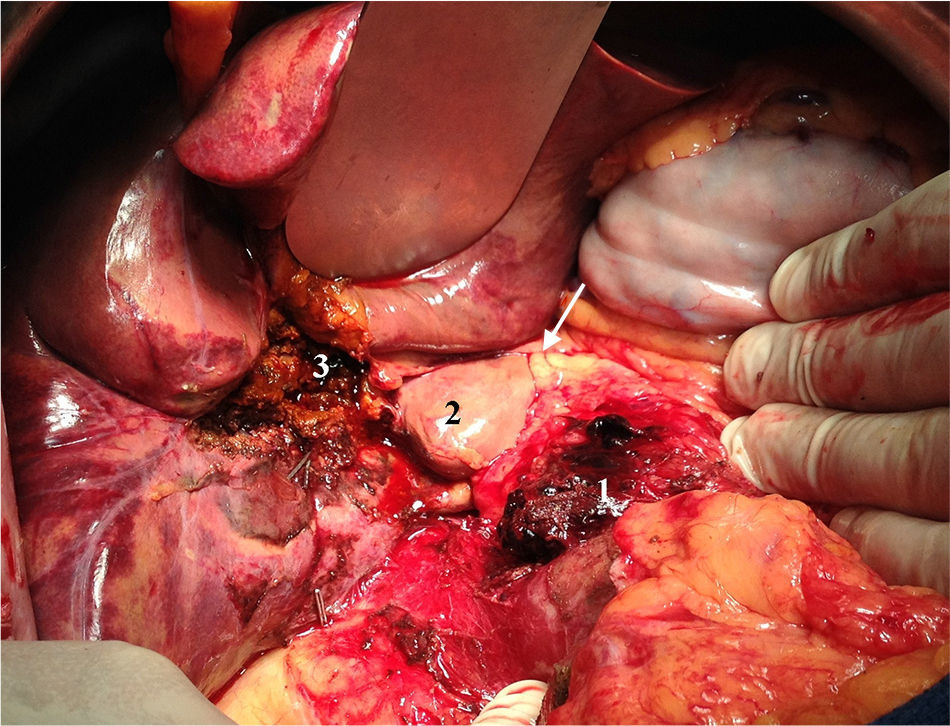
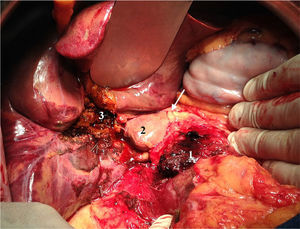
On August 18th, 7h after inclusion on the emergency list, OLT was performed with a cadaveric donor. During surgery, massive hepatic infarction was observed due to resection of the entire hepatic pedicle, along with supraduodenal iatrogenesis caused by the use of clips as well as dissection of the common hepatic artery, portal vein and bile duct (Fig. 2).
Orthotopic OLT was performed with arterial anastomosis directly to the supraceliac aorta as the hepatic artery of the recipient was considered inadequate. We performed thrombectomy of the portomesenteric venous axis with portal anastomosis, which required the interposition of an iliac vein graft. The bile duct was reconstructed by means of a Roux-en-Y hepatic jejunostomy because it was impossible to use the bile duct remains.
The patient was discharged on the 17th day of hospitalization after an uneventful postoperative period. Four months after transplantation, the patient maintains normal activity with perfect liver graft function.
The correlation between laparoscopic cholecystectomy and bile duct injuries and their management has been well studied.2,3 In all cases of suspected post-cholecystectomy iatrogenesis, conversion to open surgery is recommended in order to evaluate the severity of the lesions.7
Strasberg defines vasculo-biliary injury as injury to the bile duct, hepatic artery or portal vein. It is thought that the biliary injury may be secondary to iatrogenesis during surgery or the result of an ischemic process, as both cases are accompanied by some degree of hepatic ischemia.3,8
Portal injury is very rare, but when associated with arterial injury it leads to rapid necrosis of the liver parenchyma. This requires right hepatectomy in cases of right portal vein injury, while injury to the common portal vein trunk requires OLT.3,5
There are few case reports of biliary injury associated with complete severing of the hepatic artery and common portal vein trunk,3,6,9 but they all lead to fulminant liver failure. Given the rapidly progressing liver ischemia, it is important to immediately transfer the patient to a tertiary hospital in order to assess the severity of the injuries and to provide appropriate treatment. Emergency OLT is the only treatment option in cases of fulminant liver failure and later on in cases with complications secondary to bile duct injury, such as secondary biliary cirrhosis and uncontrollable sepsis.1,7,10 Nevertheless, even though long-term survival with good quality of life is possible, it is too high a price to pay for patients with benign disease.
Please cite this article as: Muñoz A, Rodriguez G, Torras J, Secanella L, Fabregat J. Trasplante hepático urgente tras resección completa del pedículo hepático durante una colecistectomía laparoscópica. Cir Esp. 2014;92:53–54.