The patient is a 70-year-old woman with no prior medical history of interest who came to our Internal Medicine Department complaining of pain and the sensation of a mass in the right hypochondrium. The lab work done at that time showed a normal hemogram and biochemistry. Abdominal-pelvic CT revealed the existence of a liver mass occupying the entire right hepatic lobe, irrigated by portal branches and compatible with a giant hemangioma. The patient was sent to our Hepatobiliary Surgery Unit. Magnetic resonance imaging of the liver was ordered in order to be able to better characterize the tumor, assess its relationship with different vascular structures and plan the surgical technique.
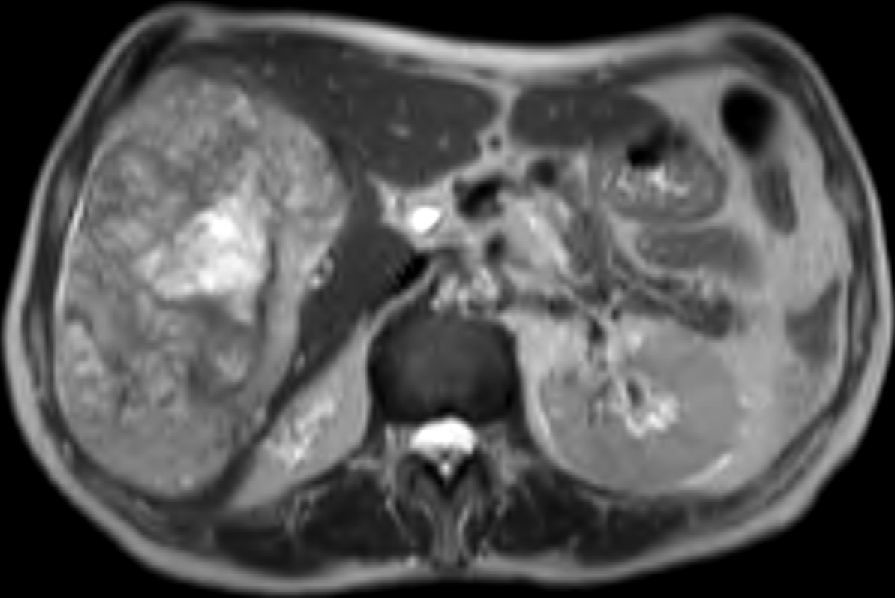
The patient came to our Emergency Department 48h after the MRI test due to epigastric pain and syncope. She presented with tachycardia (HR 130), hypotension (70/40) and tachypnea (RR 40). The blood work-up showed anemia (Hb 5.8), severe thrombocytopenia (platelets 42,000) and altered coagulation (INR 2.1). The patient was hemodynamically stabilized with fluid therapy and the transfusion of 6 units of packed red blood cells; the coagulation was corrected with the transfusion of 4 pools of platelets and 2000ml of fresh plasma. At that time, we assessed the magnetic resonance (Fig. 1), which demonstrated the existence of a voluminous liver mass measuring 18cm×12cm in the right liver lobe with intralesional bleeding.
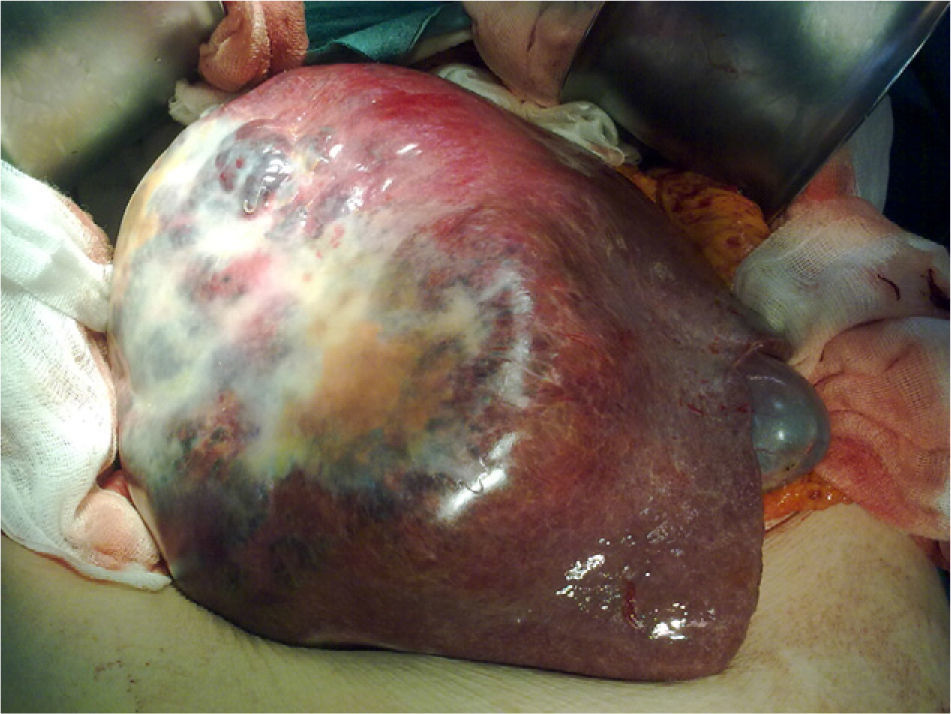
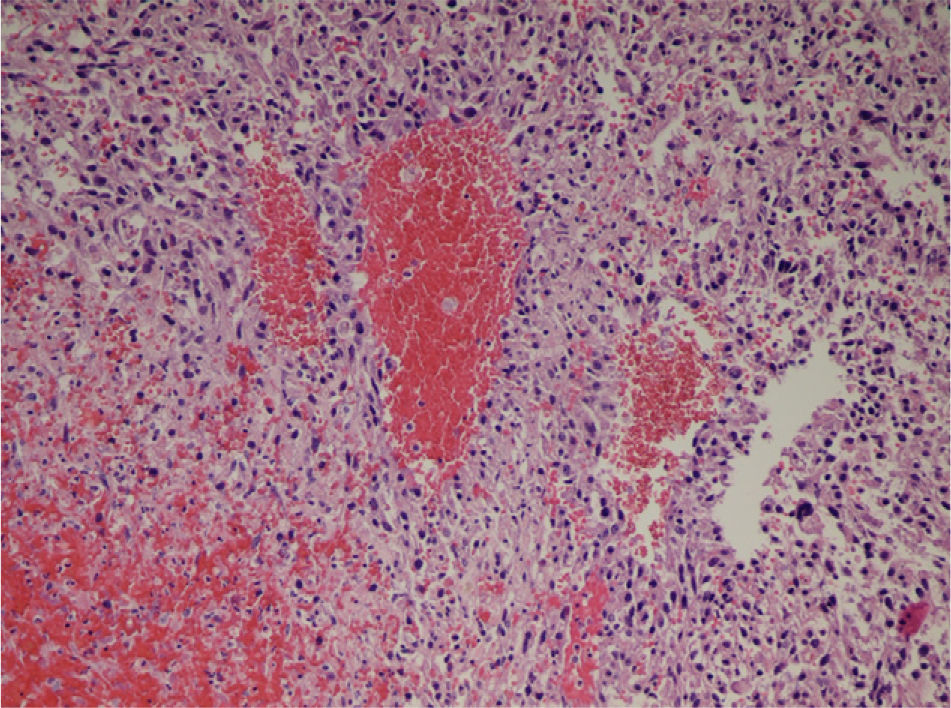
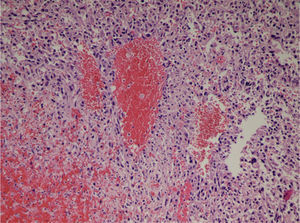
The patient was assessed by the Interventional Radiology Department of our hospital. Abdominal ultrasound showed that there was no intra-abdominal free fluid. At this time, the possibility of performing arteriography and embolization of the right hepatic artery was ruled out due to that fact that the intratumoral bleeding was from the right portal branch. The patient was taken to surgery, where we carried out an extended right subcostal laparotomy and observed a large tumor mass that occupied the entire right liver lobe from the right dome of the diaphragm to the pelvis, which was elastic in consistency and violet in color (Fig. 2). We performed right hepatectomy under total vascular exclusion. The patient was discharged on the 8th day post-surgery with no complications. In the pathology study of the surgical specimen, a neoplastic proliferation of epithelioid or fusiform cells was observed with atypia that formed nests or vascular structures interspersed with areas of hemorrhage and necrosis, showing cellular uptake with vascular markers (CD31, CD34, F.VIII), compatible with high-grade angiosarcoma (Fig. 3).
The microscopic study of the surgical specimen reveals a neoplastic proliferation of epithelioid cells with atypia forming nests or vascular structures interspersed with areas of hemorrhage and necrosis, showing cellular uptake with vascular markers (CD31, CD34, F.VIII), compatible with high-grade angiosarcoma.
Hepatic angiosarcoma or Kupffer cell sarcoma is a malignant mesenchymal tumor with a very low incidence (0.14–0.25 per million inhabitants) and represents 1.8% of all primary liver tumors. Patient age at presentation is between the sixth and seventh decades of life.1 It is associated with exposure to thorotrast (radiologic contrast material used up until the 1960s), vinyl chloride (the largest series of hepatic angiosarcoma was published in Great Britain in the 1980s and included 55 patients during a period of 20 years, all with previous exposure to vinyl chloride, used for manufacturing plastics),2 arsenic (treatment of psoriasis), and diseases such as hemochromatosis and Von Recklinghausen disease. Due to its hypervascular characteristics, it is difficult to differentiate it from other vascular tumors of the liver, such as hemangioendothelioma, hepatocarcinoma or adenoma.3 Survival without treatment is less than 6 months due to its rapid progression, high rate of recurrence and the lack of response to treatment with radio- and chemotherapy. Even liver transplantation has no benefit due to its high rate of recurrence and low survival after transplantation. Surgical resection with free margins continues to be the only treatment option, but it is technically very complex and on many occasions the disease has already disseminated before diagnosis, making resection impossible. Due to its low incidence, treatment is not clear and there is no established protocol for the treatment of hepatic angiosarcoma with active bleeding.4
In 1940, Kasabach and Merrit described a new syndrome in a boy with kaposiform hemangioendothelioma, severe thrombocytopenia, anemia and consumption coagulopathy related to activation of intravascular coagulation in intratumoral vascular lesions, which involves activation of the coagulation factors and platelet aggregation.5 Although this syndrome has never been related with hepatic angiosarcoma in adults, there is a clear parallel with our case report with regard to clinical symptoms, presentation and physiopathology.
Please cite this article as: González Rodríguez FJ, Domínguez Comesaña E, Portela Serra JL, Lede Fernández Á, Piñón Cimadevila MÁ. Actuación quirúrgica urgente en un síndrome de Kasabach-Merrit asociado a angiosarcoma hepático gigante. Cir Esp. 2014;92:370–372.