Minimally invasive anatomical sublobar resections have gained relevance in recent years mainly due to advances in imaging techniques, screening programs and the increase in second neoplasms. Accurate identification of the segmental or subsegmental bronchus is vital to guarantee optimal results in segmentectomies and subsegmentectomies. Given the complexity and the possibility of anatomical variations, several authors have published different methods to identify the target bronchus. However, these methods have certain limitations. This article describes a new rapid and effective technique, with a low risk of complications and without additional cost, for the identification of segmental bronchi in minimally invasive segmentectomies.
Las resecciones sublobares anatómicas mínimamente invasivas han ganado relevancia durante los últimos años gracias al avance de las técnicas de imagen, los programas de cribado y el aumento de segundas neoplasias. La identificación precisa del bronquio segmentario o subsegmentario objeto de resección es vital para obtener resultados óptimos en segmentectomías y subsegmentectomías. Dada la complejidad y la posibilidad de variaciones anatómicas, varios autores han publicado distintos métodos para identificar el bronquio objetivo de la resección. Sin embargo, estos métodos tienen ciertas limitaciones. El presente artículo describe una nueva técnica rápida, efectiva, con bajo riesgo de complicaciones y sin coste adicional para la identificación de los bronquios segmentarios en segmentectomías mínimamente invasivas.
In recent years, lung cancer screening programs using low-dose computed tomography have become widespread and, consequently, small lung lesions are being detected more frequently, whose significance is often uncertain. In particular, the diagnosis of subcentimeter or subsolid lesions has been increasing; in these cases, limited resections have been shown to be a valid therapeutic option.1,2 In this context, the recently published results of the JCOG0802/WJOG4607L clinical trial3 could change the current standards of extension of surgical resection in favor of segmentectomy in patients with non–small-cell lung carcinoma lesions smaller than 2 cm with no lymph node involvement. Furthermore, the risk of developing a second pulmonary primary lesion after initial surgical treatment for lung cancer is high,4 and many patients with poor lung function due to previous resection can only be offered an anatomical resection limited to the affected segment.5 Thus, the indications for anatomical lung segmentectomies have increased in recent years. Given that there is a wide variety of possible segmentectomies and the likelihood of finding anatomical variations in the structures of pulmonary vessels and bronchi is high, it is relatively difficult to develop the experience and skills necessary for this type of surgical procedure. Therefore, the success of these complex interventions is highly dependent on the intraoperative interpretation of the segment's anatomy, especially in minimally invasive approaches. The correct identification of anomalous branches of the pulmonary vessels or bronchi is important to avoid intraoperative accidents, such as bleeding, postoperative infarct or ventilation defects. Several authors have published different methods6–9 to guarantee correct intraoperative bronchial identification, although these methods have certain limitations. Thus, to date, there is no standardized technique to directly mark the target bronchus.
In this article, we describe a method for identifying the target bronchus in minimally invasive anatomical segmentectomies based on the use of near-infrared fluorescence.
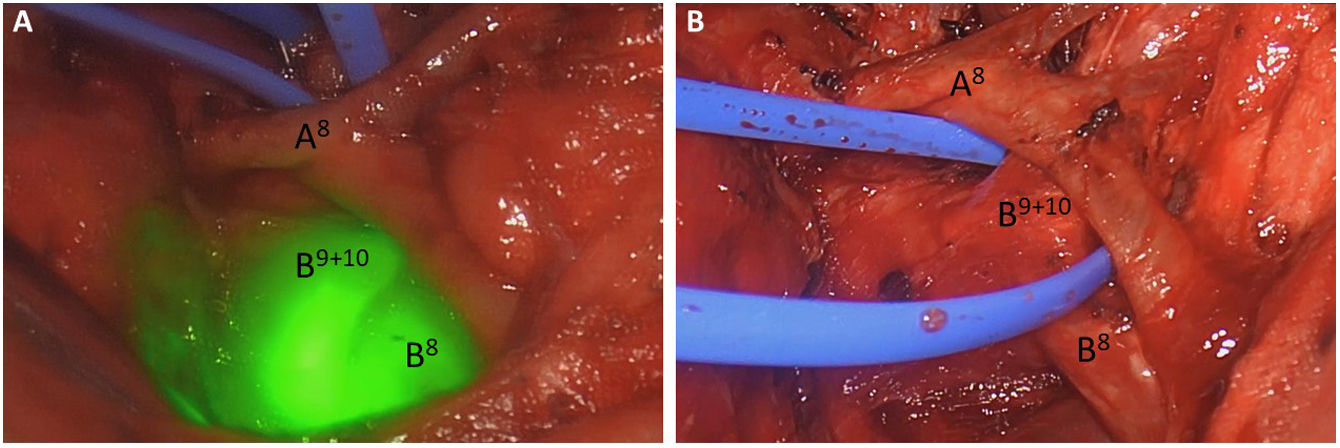
Surgical techniqueCase 1A 79-year-old patient with a history of treated rectal adenocarcinoma presented a 1.9-cm lung lesion located in left segments 9–10 during follow-up. The patient was scheduled for left S9+10 video-assisted thoracoscopic segmentectomy. To achieve one-lung ventilation, the patient was intubated with a left double-lumen endotracheal tube, and correct tube positioning was confirmed with a flexible intubation bronchoscope (KARL STORZ GmbH & Co KG, Tuttlingen, Germany). During the procedure, after dividing arterial branch A9+10, segmental bronchi B9+10 were identified endoscopically by inserting the previously used bronchoscope through the bronchial lumen. Once the B9+10 segmental bronchi had been identified endoscopically by an expert surgeon, the tip of the bronchoscope was focused on the target segmental bronchus, and the standard video-thoracoscopic view of the Stryker 1688 Advanced Imaging Modalities 4 K thoracoscopy platform (Stryker, Kalamazoo, MI, USA) was changed to near-infrared fluorescence overlay, providing visualization of the luminescence of the target bronchi without the need to administer indocyanine green (Fig. 1).
A) Visualization and identification of the bronchial segment anatomy with video-assisted thoracoscopic vision with near-infrared fluorescence overlay after inserting the bronchoscope though the endotracheal tube; indocyanine green was not administered; B) Standard video-assisted thoracoscopy view after dissection of the B9+10 bronchus.
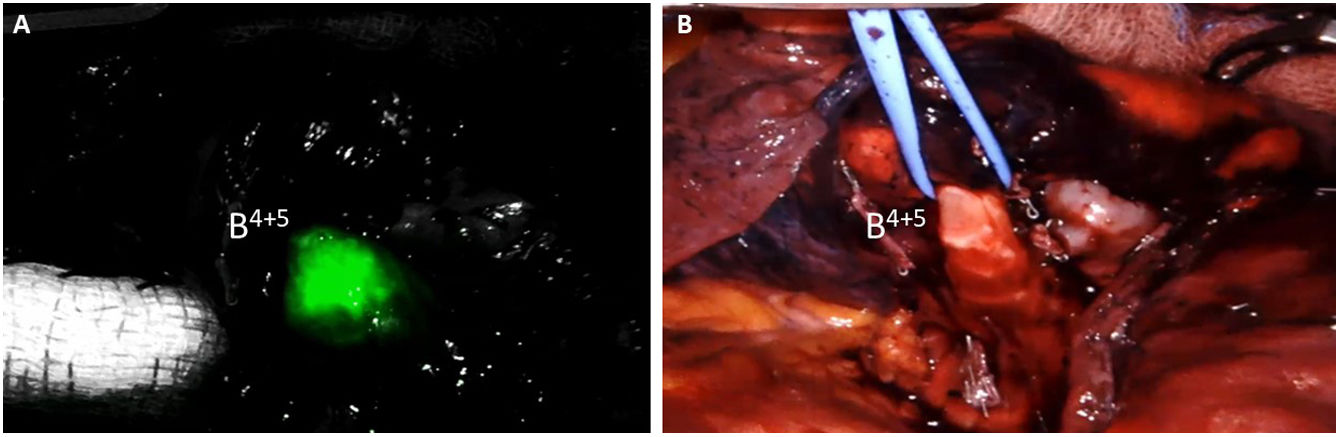
A 60-year-old patient with a history of ischemic heart disease was diagnosed with adenocarcinoma of the colon. The extension study revealed a 2 cm pulmonary nodule located in the lingula. The patient was scheduled for a robotic lingulectomy. In this case, to achieve one-lung ventilation, the patient was intubated with a single-lumen tube with a built-in blocker; correct positioning of the tube and blocker was confirmed with a single-use flexible video bronchoscope (Ambu® aScope™ Broncho Slim 3.8/1.2). After independently dividing arterial branches A4 and A5 and the lower branches of the superior pulmonary vein V4+5, segmental bronchi B4+5 were identified endoscopically by introducing the previously used video bronchoscope through the endotracheal tube after cessation of ventilation on the mechanical respirator and deflation of the blocker cuff. Once the B4+5 segmental bronchi had been identified by the expert anesthesiologist and confirmed on the monitor (Ambu® aView™) by the surgeon in the surgical field, the console surgeon activated the FireFly infrared fluorescence system integrated in the daVinci® X robot (Intuitive Surgical, Sunnyvale, CA, USA), providing visualization of fluorescence in the target bronchi without the need to administer any dye with fluorescent properties (Fig. 2).
DiscussionThe anatomical structure of the different lung segments is complex and often demonstrates individual variations; hence, segmentectomies, and especially subsegmentectomies, are a challenge for many surgeons. To date, different methods have been used to identify the segmental structures and the intersegmental plane. Three-dimensional (3D) computed tomography bronchography and angiography6 is the most widely used technique. This method facilitates the correct interpretation of the 3D arrangement of the segmental structures and allows for 3D models to be printed. However, it does not provide for direct marking of the target bronchus during surgery. Recently, Xu et al8 have described a new method for the identification of the segmental bronchus based on bronchial labeling with methylene blue guided by electromagnetic navigation bronchoscopy (ENB). Although this method is feasible and effective for the identification of segmental and subsegmental bronchi, it has certain drawbacks, such as the need for specific equipment (ENB system) and the additional time required for the identification and marking of the bronchus. In addition, the amount of methylene blue injected must be optimal to prevent dissemination of the dye in the bronchial tree and to avoid incorrect bronchial identification.
Our study describes a fast, effective technique for the identification of segmental bronchi during minimally invasive segmentectomies (both video-assisted thoracoscopic and robotic) that has a low risk of complications, no additional cost, and could safely shorten the duration of these procedures. The main advantages of the technique described are that it is a fast and safe procedure that does not require the consumption of additional material resources or the administration of any agent with fluorescent properties. The essential requirements to successfully conduct this technique include a near-infrared fluorescence video-assisted thoracoscopy platform (the daVinci® robotic platform has the integrated FireFly system) and a surgeon or anesthesiologist expert in bronchoscopy present in the operating room to correctly identify the target segmental bronchus.
In conclusion, our study demonstrates the utility of near-infrared fluorescence for the identification of segmental bronchi in minimally invasive segmentectomies.
Conflict of interestsThe authors declare that they have no conflict of interest.