Verrucous carcinoma (VC) is a rare variant of squamous carcinoma that is difficult to diagnose and whose therapeutic management should be individualized. Its location in the esophagus, first described by Minielly in 1967,1 is rare, and only 50 cases have been reported in the literature.
Its exact etiology is unknown, but VC is strongly associated with prolonged inflammatory factors, such as achalasia, gastroesophageal reflux disease, alcohol and tobacco use. The most recently published cases suggest a possible relationship with papillomavirus (HPV) infection, which is why this cause should be considered in all patients with this suspected diagnosis.2
VC predominantly affects males (ratio 2:1) with a mean age of 60 (range 36–79 years). The main clinical manifestation is dysphagia, which is usually accompanied by weight loss. Other symptoms may include hematemesis, cough and odynophagia.
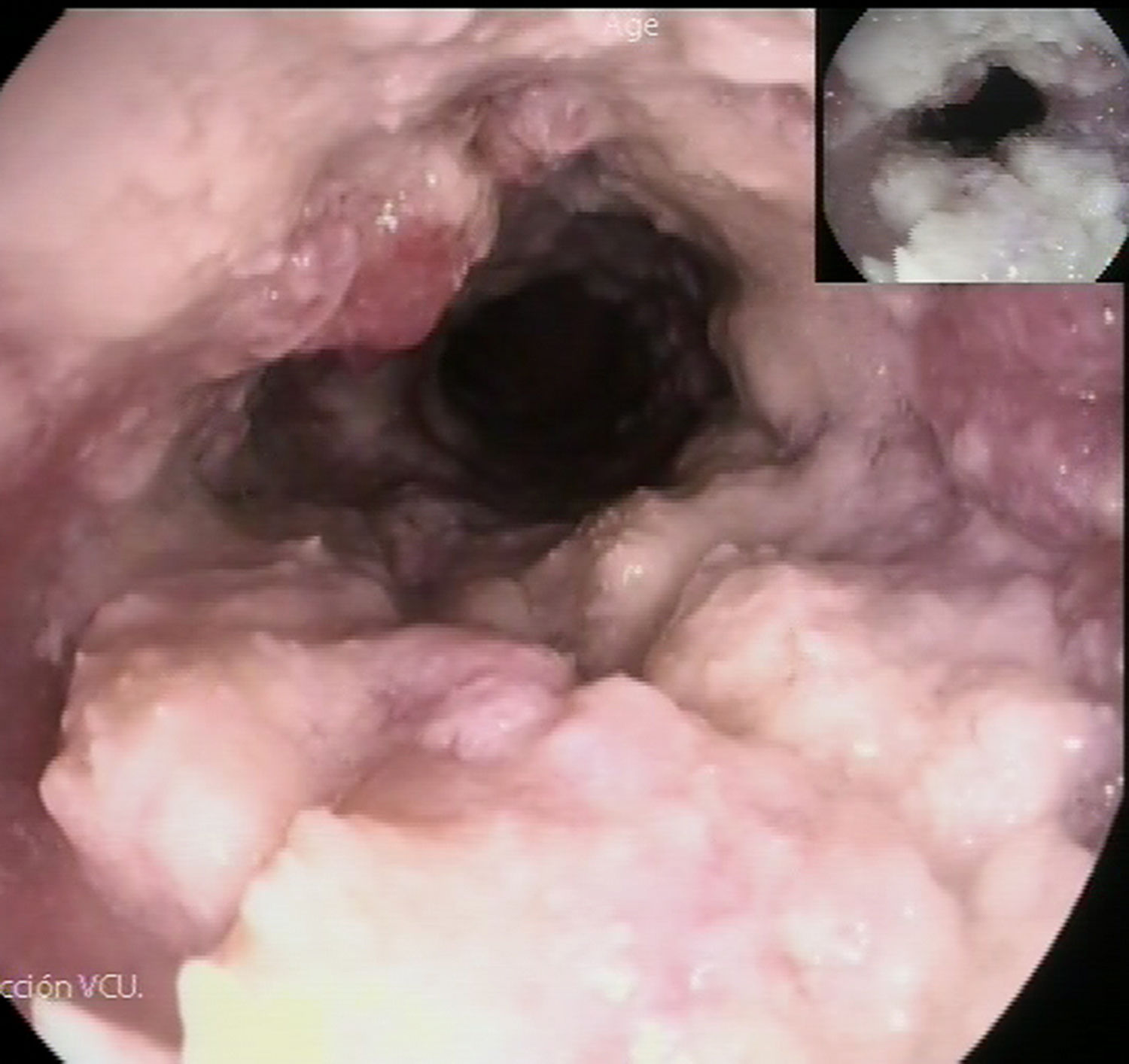
The suspected diagnosis can be established by endoscopy, with a typical macroscopic appearance consisting of a whitish wart-like mass. The exophytic nature of these lesions makes it very difficult to obtain biopsies in which the invasive component of the tumor is visualized. Frequently, only nonspecific inflammatory changes with the absence of malignancy are observed. Therefore, complete tumor resection is usually necessary to reach a definitive diagnosis.3
The pattern of superficial growth, limited lymph node and distant involvement, and the response to chemoradiotherapy differentiate VC from squamous cell carcinoma, making endoscopic resection and neoadjuvant treatment valid alternatives to esophagectomy.
The objective of this article is to describe a case of esophageal VC that demonstrates the difficulty to diagnose and stage this entity, and, therefore, to choose its treatment.
The patient was a 50-year-old man with progressive weight loss and dysphagia in previous months. He was a heavy drinker, smoker, and had a history of gastroesophageal reflux disease and achalasia, which had been treated with a Heller myotomy 12 years earlier.
Three esophagogastroscopies were performed with biopsies, none of which contributed to the definitive diagnosis. All reported a mucosa that was completely covered by whitish, non-cottony exudates between 20 and 32cm from the dental arch that could not be removed with washing; there was also adhered food debris and a papilliform polypoid nodular mass 26cm from the arch (Fig. 1). The pathology studies showed evidence of a papillomatous and verruciform hyperplastic keratinizing epithelium, with notable superficial acute and deep chronic inflammatory infiltrate, no signs of malignancy and with fungal structures.
The study was completed with a computed tomography scan, hybridizations for HPV and lab work-up, including tumor markers, which were negative.
Given the high suspicion of VC that was not confirmed, the patient was referred to another hospital for an endoscopic ultrasound, which reported the same endoscopic findings as well as loss of structure of the esophageal wall and loss of layered pattern, hypoechogenic appearance, indentations in the esophageal adventitia (suggestive of T3 if the tumor nature is confirmed), and no invasion of neighboring structures or lymphadenopathies associated with the tumor or in the area of the celiac trunk.
Despite not having histological confirmation, after assessment of the case in the Digestive Tumors Committee, we decided to perform a transhiatal esophagectomy with sleeve gastroplasty, ruling out endoscopic resection due to the endoscopic ultrasound findings.
The postoperative period ran its course with dehiscence of the cervical anastomosis and secondary respiratory distress, associated with symptoms compatible with alcohol withdrawal syndrome. The patient was managed conservatively, developing dysphagia secondary to stenosis of the esophagogastric anastomosis, which was resolved after endoscopic dilatations.
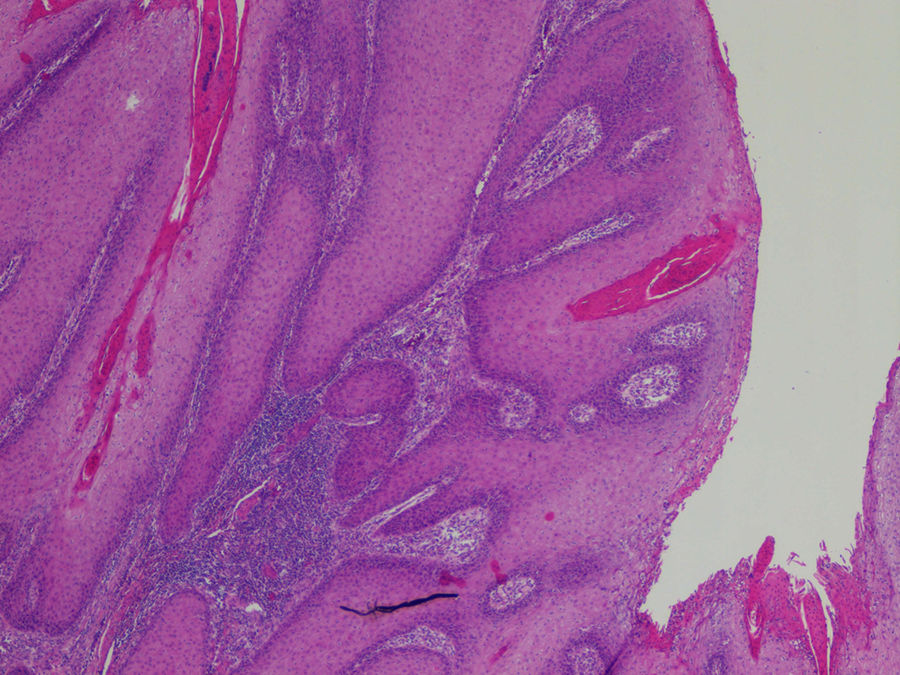
In the histological study of the surgical specimen, a well-differentiated malignant epithelial neoplasm was observed with acanthotic and hyperkeratotic superficial papillomatous growth with minimal basal atypia and chronic deep inflammation. The neoplasm showed extensive superficial growth, predominantly intramucosal, although the muscularis propria was free of neoplastic infiltration. The definitive pathology diagnosis was well-differentiated verrucous squamous cell carcinoma, with free surgical margins, absence of lymph node metastasis and associated areas of Barrett's esophagus (TNM stage: pT1N0) (Fig. 2).
As in our case, it is not uncommon to find disagreement between the endoscopic ultrasound and the definitive pathology study, due to the high level of chronic deep inflammation that may lead to overstaging by endoscopic ultrasound.4
The differential diagnosis of VC should include benign lesions associated with stenosis or dysphagia, such as esophageal leiomyoma, papilloma or esophageal tuberculosis, and with malignant lesions like adenocarcinoma of the esophagus.5
As this pathology is rare, there are no precise recommendations for its treatment. Endoscopic mucosal and submucosal resections have been described for early stages, with good results.6 Other authors, including Brandalise et al.,7 have described a positive response to neoadjuvant treatment in patients with involvement of the entire esophagus, allowing for more conservative resections.
However, despite its slow growth and high degree of differentiation, due to the frequent diagnostic delay in locally advanced stages, esophagectomy continues to be the most common therapeutic option.8
Morbidity and mortality are associated with local invasion (pulmonary, bronchial, pleural and pericardial involvement) and surgical complications (fistulas). No distant metastasis has been reported in the literature.9
Please cite this article as: Paseiro Crespo G, García Nebreda M, Barceló López M, Marqués Medina E, Gimeno Aranguez M. Carcinoma verrucoso esofágico: una rara entidad de difícil diagnóstico. Cir Esp. 2018;96:453–455.