Retrorectal cystic hamartoma, or tail-gut, is a rare malformation derived from embryonic remnants of the intestine that can manifest as pain, obstruction or superinfection. Several surgical approaches have been described, including transperineal, transabdominal, laparoscopic and, recently, TEM access. Complete removal of the epithelium of the cyst is an essential condition for healing, as its persistence would lead to recurrence. We present the case of a patient who had been treated surgically five times: thrice by perineal access, one laparoscopy-assisted, and finally the transrectal access using TEM.
The patient is a 37-year-old woman whose only history of interest was perianal suppuration since childhood. Initially, she had been diagnosed with a perianal abscess that debrided spontaneously. Subsequently, she underwent elective surgery for perianal fistula flattening at the ages of 16 and 20. Given the recurring perianal disease, a rectal MRI was performed in 2008, which demonstrated the existence of a retrorectal hamartoma (tail-gut cyst).
Given this diagnostic evidence, elective surgery was performed in October 2008, and, using a left sacrococcygeal perineal approach with resection of the coccyx, the cystic lesion was resected and the external sphincter was repaired. The pathology study showed a cystic lesion covered with non-keratinized squamous epithelium compatible with retrorectal cystic hamartoma with extension to the periosteum of the coccyx. After an asymptomatic period, in 2012 the patient presented a new episode of anal suppuration while pregnant, which was self-limiting with antibiotic treatment. After childbirth, a new MRI demonstrated recurrence of the retrorectal cystic lesion. In February 2013, the patient was operated on again, involving laparoscopic excision of the cystic lesion. The patient remained asymptomatic until September 2017.
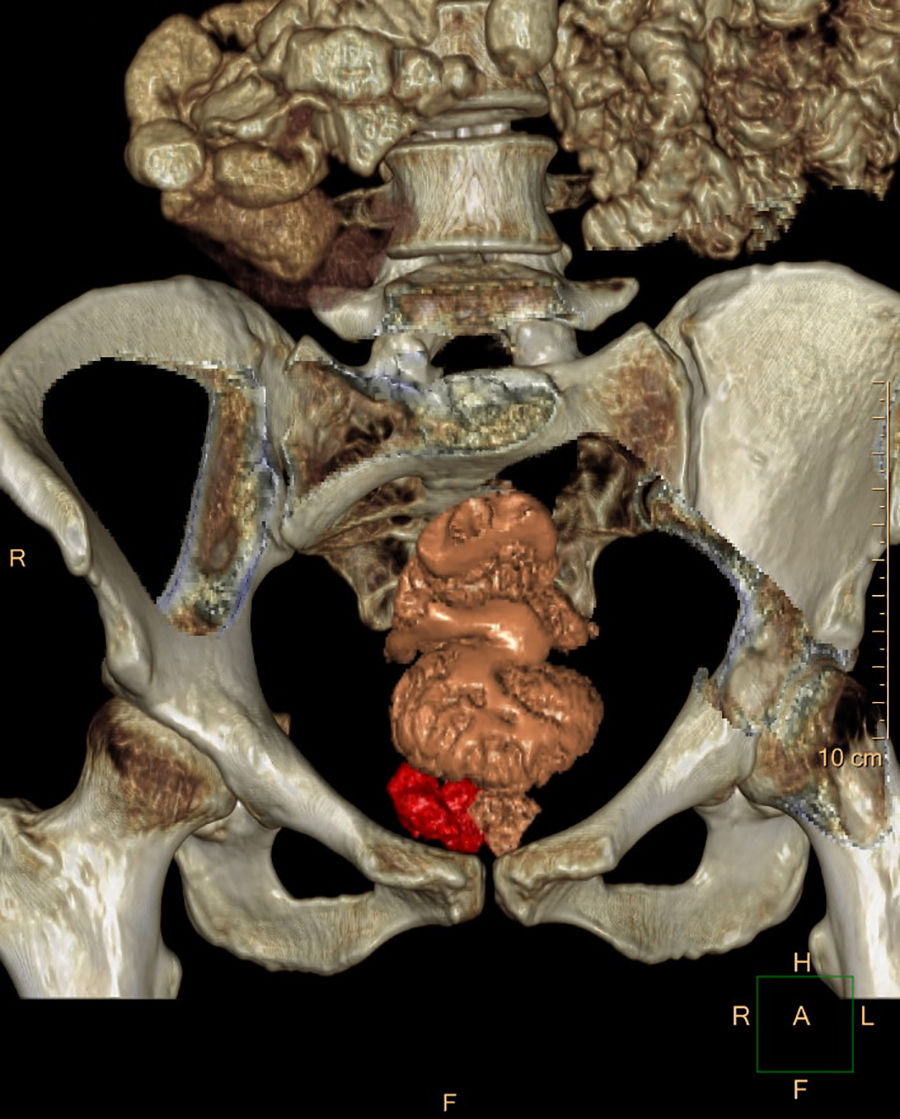
In a follow-up study due to the reappearance of discomfort in the perineal area, MRI (Fig. 1) and 3-D CT reconstruction (Fig. 2) showed a cystic lesion measuring 26×30×10mm in diameter in the right ischioanal fossa above the sphincter complex, compatible with recurrence/persistence of a retrorectal cystic hamartoma. Given the anatomical location of the lesion in the lower-third of the rectum and the probable existence of perilesional fibrosis, we decided to perform a transanal approach using TEM, and the cystic lesion was able to be completely removed. The patient was discharged without incident 48h later. The pathology study confirmed the recurrence of a retrorectal cystic hamartoma with disease-free margins.
Tail-gut or cystic hamartomas are congenital in origin, derived from embryonic epithelial cells of the intestine. According to the retrorectal tumor (RT) classification by Hulingand, Johnson or Dozois,1 tail-gut has a benign behavior.
RT are very rare lesions, with an undefined incidence ranging from 2 to 6 cases per year at reference hospitals.2 The symptoms these patients present are nonspecific, so the diagnosis is usually incidental or casual.3
The diagnosis and classification of RT is done by CT and MRI,3 not requiring biopsies in most cases.
The treatment of these lesions is surgical and the approach is classically determined by the Woodfield algorithm,4 which indicates either an abdominal or perineal approach according to the location of the lesion in reference to the S3–S4 vertebrae. The possibility of malignancy, size, vascularization, relationship or infiltration of neighboring structures are also important when determining the approach.
Laparoscopy plays an important role in the surgical treatment of RT. Recently published series, one with 12 cases5 and our own with 11,6 have shown that this option is possible, with low morbidity and very low recurrence rates. Another surgical possibility is the approach of these lesions by TEM, which has also been described in the literature in several series of 3,7 48 and 6 patients,9 all of them being tail-guts of about 3cm in diameter located at about 6cm from the anal margin. During a 20-month radiological follow-up, there was no evidence of recurrence.
In the case of benign embryonic RT, recurrence was very uncommon at about 0–11%5–10 with 10-year follow-ups.1 Incomplete excision of the cyst epithelium was emphasized as the most important factor in recurrence.
The transanal approach by TEM may be indicated in benign retrorectal lesions, especially if the location of the lesion is in the middle or distal third of the rectum. The disadvantages are those associated with the technique itself: the learning curve, the cost of the apparatus and the opening of the rectal wall. Given the difficulty of the laparoscopic approach in this type of injury, TEM is an alternative to be considered.
Please cite this article as: Hernandez Casanovas P, Bollo Rodriguez J, Martinez Sanchez C, Pernas Canadell JC, Targarona Soler EM. Tratamiento mediante microcirugía endoscópica transanal de un hamartoma quístico retrorrectal birrecidivado. Cir Esp. 2018;96:455–456.