Intraductal papillary neoplasm of the bile duct (IPNB) is an uncommon condition characterized by the exophytic papillary growth of the biliary epithelium toward the ductal lumen. Previously included in the group of tumors with the same name located in the pancreas, these neoplasms present evident differences and, since 2010, they have been considered a separate entity with demonstrated potential for malignization toward cholangiocarcinoma.1,2
We present the case of a patient with IPNB who was operated on at our hospital.
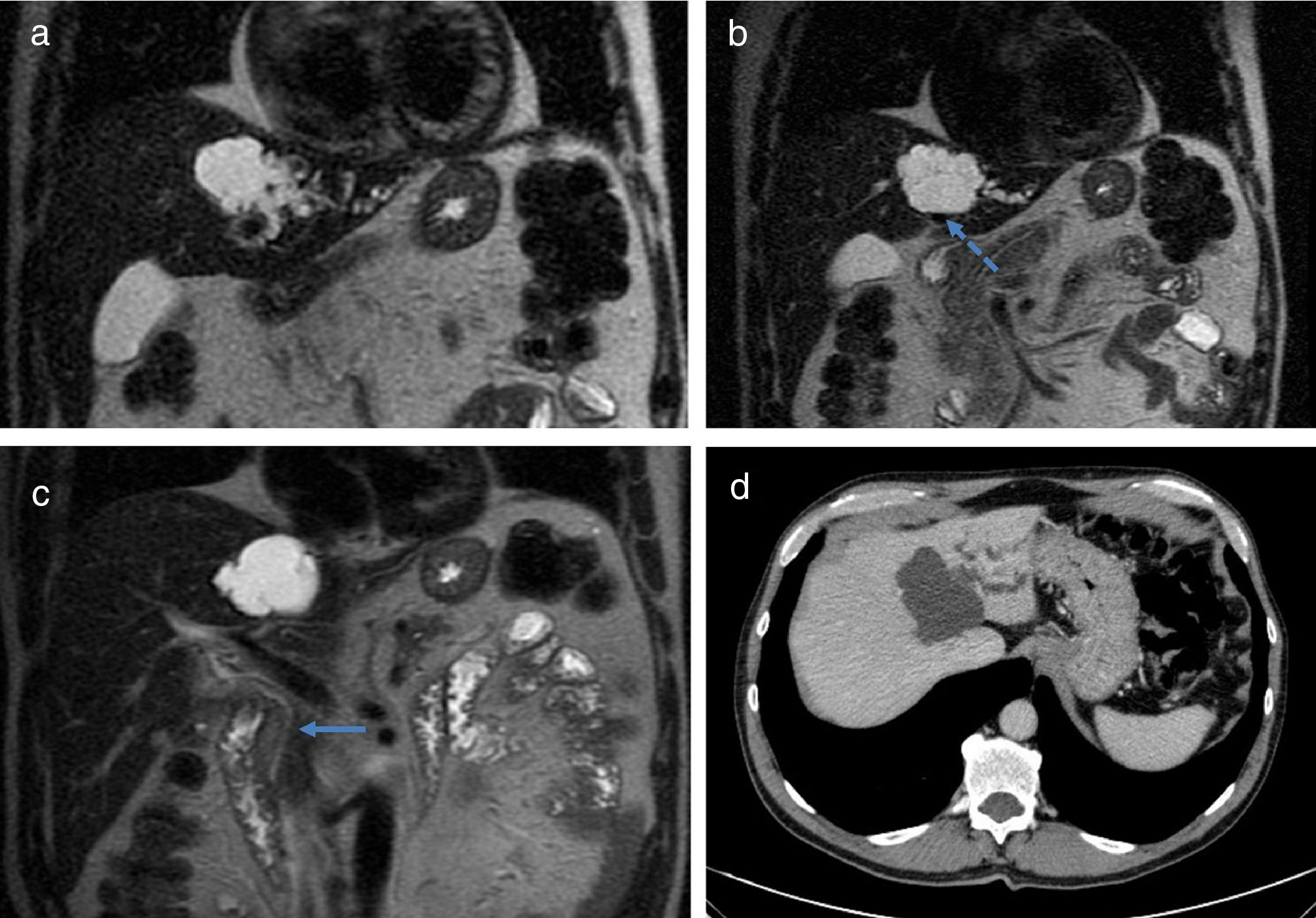
The patient is a 59-year-old male, who was asymptomatic and had no pathological history. A routine ultrasound detected a 5×5cm cystic lesion in the left hepatic lobe, with dilation of the intrahepatic left bile duct (BD), while the extrahepatic duct was normal. Computed tomography and magnetic resonance cholangiography showed evidence of a polylobulated cystic lesion in segment IV, with thin interior walls and no solid or enhanced areas. It caused compression of the left portal branch and dilatation of the bile ducts of segments II–III, which came into contact with the lesion (Fig. 1). Endoscopic ultrasound confirmed the described findings, as well as the normal diameter of the extrahepatic BD (Fig. 2). The lab work-up showed normal liver function and tumor markers.
(a) Magnetic resonance cholangiography image showing the cystic lesion and dilatation of the left intrahepatic bile duct; (b) MRCP image showing the relationship of the lesion with the left portal branch, displacing it (dashed arrow); (c) MRCP image showing a normal diameter of the extrahepatic bile duct (solid arrow); (d) computed tomography image showing the lesion in segment IV and dilation of the left intrahepatic bile duct.
With the suspected diagnosis of mucinous cystic neoplasm of the liver, surgical treatment was indicated. A laparoscopic approach was used to perform intraoperative ultrasound, which located the lesion in segment IV, in close contact with the left portal vein and the middle hepatic vein, and BD dilatation in segments II–III was confirmed. Laparoscopic left hepatectomy was performed. The postoperative period was uneventful and the patient was discharged on the fourth day. The histopathological study revealed the presence of ducts with cystic dilatations containing mucin, covered by cylindrical epithelium, with foci in the shape of papillary projections and no invasion of the stroma, all compatible with pancreatobiliary IPNB, with low-grade dysplasia and free resection margins. After a 40-month follow-up, the patient did not present recurrence.
IPNB is a very infrequent pathology in our environment. It usually occurs in middle-aged Asian men, and risk factors include hepatolithiasis as well as clonorchiasis.3 It tends to be multifocal and can occur at any point of the extra- or intrahepatic BD, the latter being more frequent in the left hepatic lobe,4,5 as in our case. Although up to 30% of patients remain asymptomatic, presentation is usually in the form of pain, obstructive jaundice or cholangitis.4
Preoperative diagnosis is difficult and requires the combination of several imaging tests; the differential diagnosis should include cystic liver lesions. The radiological appearance observed on ultrasound, computed tomography and magnetic resonance is BD dilatation (with three possible patterns: diffuse duct ectasia, segmental dilatation or cystic dilatation), associated or not with intraductal masses.3,6 In our case, the cystic, walled, compressive nature, with no apparent communication with the BD, led to the erroneous presumptive diagnosis of mucinous cystic neoplasm of the liver.6 Endoscopic retrograde cholangiography may be useful for confirming BD dilatation and filling defects, but mucobilia is also evident in one-third of patients.5 Intraductal ultrasound and cholangioscopy (transhepatic or oral) have also been used with biopsy, although these are only cost-efficient for the diagnosis of malignancy in 50% of cases, due to multicentricity.7
From the pathological standpoint, despite being more heterogeneous, these neoplasms are classified into four subtypes like pancreatic intraductal papillary neoplasms (pancreatobiliary, intestinal, gastric and oncocytic). The pancreatobiliary type is the most frequent in IPNB, which usually expresses mucin core proteins-1 (MUC-1) and has a poorer associated prognosis than the remaining subtypes.2,4,5,8
Considering the degree of dysplasia and depth of the invasion, IPNB are classified into 4 stages: (1) IPNB with mild-moderate dysplasia; (2) IPNB with high-grade dysplasia; (3) stage T1 cholangiocarcinoma of the American Joint Committee on Cancer; and (4) stage ≥T2 cholangiocarcinoma of the American Joint Committee on Cancer.3,9 In 40–80% of the cases, there will be foci of invasive carcinoma or of mucinous or tubular adenocarcinoma, a figure that is significantly higher than in pancreatic intraductal papillary neoplasms.4,8
It is because of this potential for malignization that surgical treatment is indicated whenever distant disease is ruled out. Major hepatectomy is recommended, either with or without lymphadenectomy and associated or not with BD resection.7 It is important to check the biliary resection margins since these tumors seem to have a superficial dissemination pattern, which, according to the series, is responsible for a recurrence rate (mainly locoregional) that reaches 47–60% within 5 years in cases of malignant degeneration.3,7 Nevertheless, the prognosis of these lesions seems to be better than in conventional cholangiocarcinoma, with survival rates close to 69% 5 years after surgery.3,4,7,10
In conclusion, despite the infrequent presentation of IPNB in our setting and its difficult preoperative diagnosis, this entity with a potential for malignancy should be included in the differential diagnosis of cystic liver lesions. With radical surgical treatment and free resection margins, the prognosis of these patients with localized lesions is acceptable.
Please cite this article as: de la Serna S, Pérez-Aguirre E, Díez-Valladares LI, García-Botella A, Torres García AJ. Neoplasia papilar intraductal de vía biliar: un reto diagnóstico para un correcto tratamiento. Cir Esp. 2018;96:457–459.