In recent years, femoral artery pseudoaneurysms have been an increasingly frequent complication. They can be caused by peripheral catheterization or appear at the site of a bypass anastomosis (vein or stent).1,2 According to the latest series, anastomotic pseudoaneurysms (APA) complicate arterial anastomoses from 1.4% to 4%. Their mean interval for presentation is 6 years, and even less if associated with superinfection (the presence of bacterial colonization in APA is 80%).3,4 APA present as a dilation of the arterial wall adjacent to the anastomosis, and its most common manifestation is a painful and hyperpulsatile inguinal mass,2 which is why it should be included in the differential diagnosis of all inguinal masses. Thrombosed APA that are overinfected may present as a non-pulsatile mass with surrounding erythema, imitating a strangulated hernia.5 There is a life-threatening risk for APA rupture and hemorrhagic shock, entailing a surgical emergency that makes its early diagnosis of utmost importance.6
We present the case of a 76-year-old hypertensive, insulin-dependent diabetic, obese male patient with a body mass index of 37.5. His medical history included revascularized ischemic cardiomyopathy with a triple coronary bypass and atrial fibrillation treated with Sintrom®. His surgical history of interest included left carotid endarterectomy and repair of an uncomplicated abdominal aortic aneurysm with aortobiiliac bypass and right iliofemoral bypass with Dacron® prosthesis together with right femoral endarterectomy 12 years earlier. The patient came to the general surgery outpatient clinic for a symptomatic right inguinal mass that increased with Valsalva maneuvers and had grown progressively over the past year; he was diagnosed with right inguinal hernia and was pending weight reduction to schedule surgical repair.
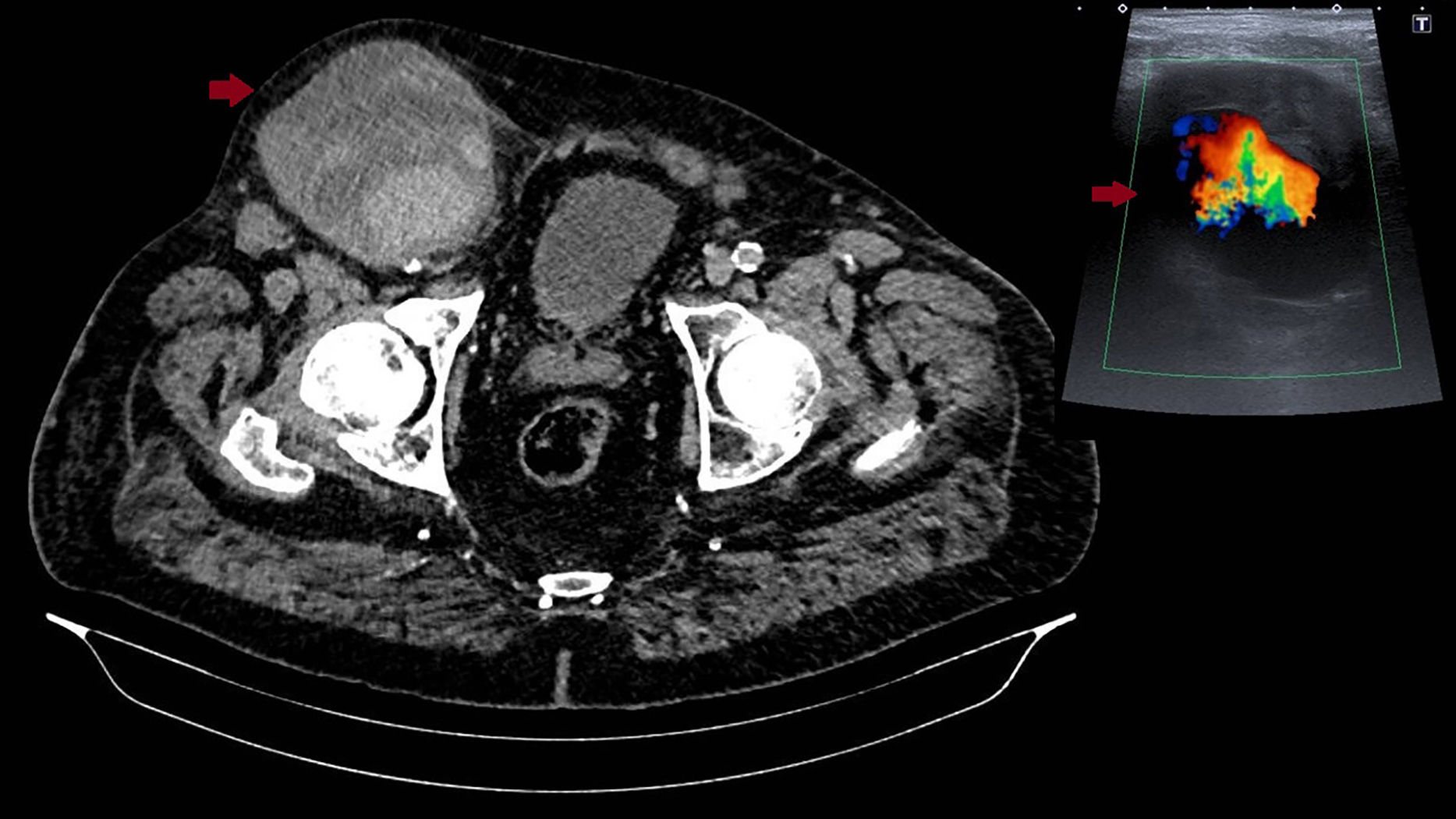
Eleven months after diagnosis, the patient went to the hospital emergency department due to sudden, self-limiting pain in the right iliac fossa and a sensation of low-grade fever. On examination, the abdomen was distended yet soft, bowel sounds were present and there were no signs of peritoneal irritation; an indurated mass was observed in the right inguinal region that was painless on palpation; there was no evidence of abdominal or inguinal scars. The patient was assessed by a general surgeon on duty and diagnosed with an incarcerated inguinal hernia following attempted reduction and the administration of a muscle relaxant. After inguinal manipulation, the patient presented sudden worsening of pain with signs of hemodynamic instability. Urgent abdominal ultrasound was ordered, followed by CT angiography (Fig. 1), which showed a large aneurysmal dilatation in the right iliofemoral region measuring 10cm (anteroposterior)×9cm (transverse) with partial thrombus and peripheral areas compatible with acute arterial bleeding from the ruptured right iliofemoral APA.
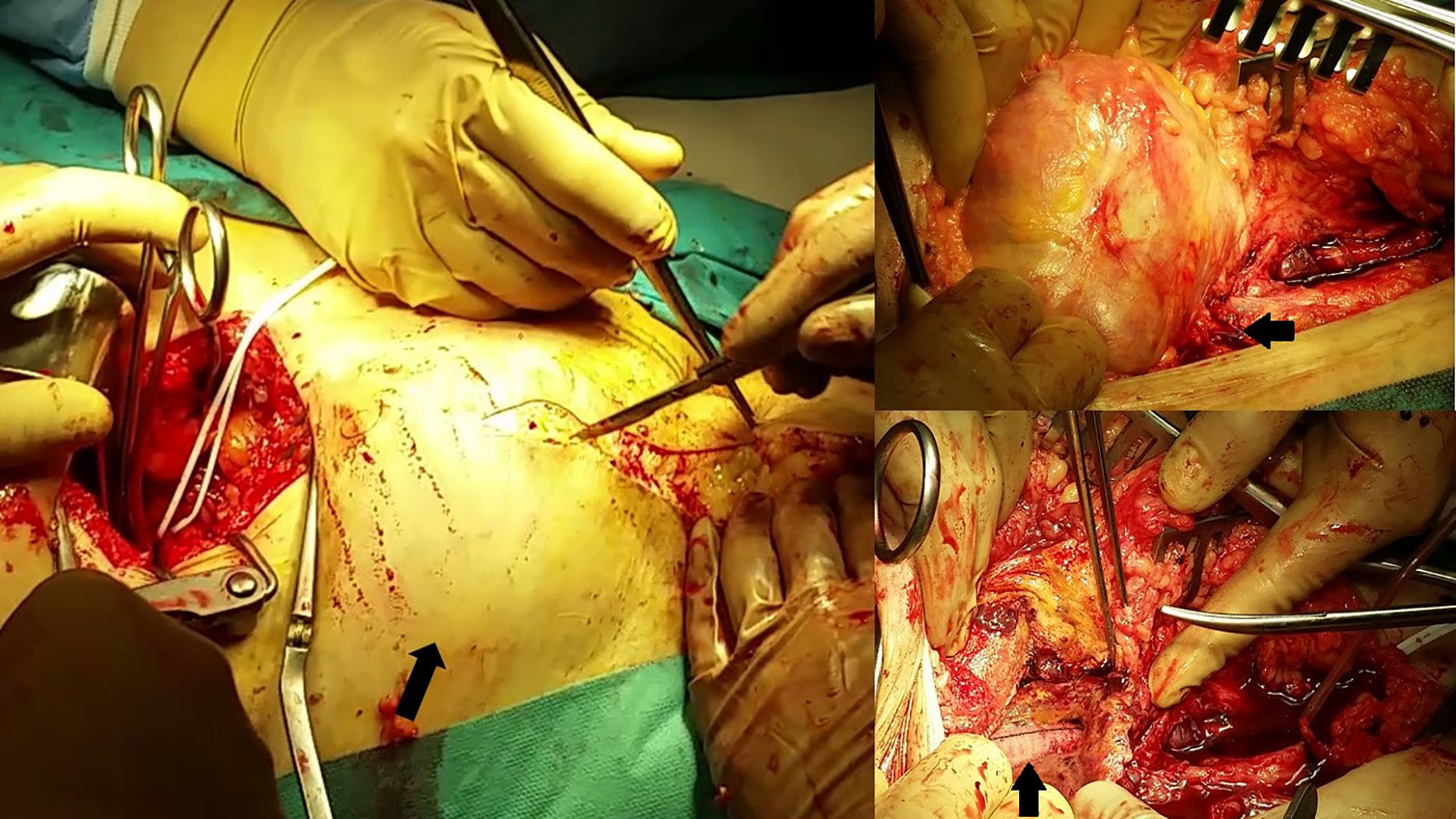
Given these findings, the patient was transferred urgently to the referral hospital for vascular surgery assessment. Upon arrival, the patient was hemodynamically stable, with no need for vasoactive support. He presented a very painful right inguinal hyperpulsating mass and preserved bilateral femoral pulse with adequate distal perfusion. After coagulation correction, urgent surgery was conducted, involving resection of the femoral para-anastomotic aneurysm (Fig. 2) with iliac clamping using a low retroperitoneal abdominal approach and closure with a “shotgun barrel” bovine pericardium patch in between the superficial and deep femoral arteries. An intraoperative biopsy was taken for microbiology study that detected Staphylococcus hominis hominis, which was treated according to the antibiogram. After surgery, the patient experienced chest pain due to hypertensive heart disease assessed by the Cardiology Department, and there have been no further incidents of interest to date.
A femoral pseudoaneurysm is an artery wall defect causing the leakage of blood into adjacent soft tissue and subsequent fibrous encapsulation.1 APA can present in a variable time after vascular reconstruction, most frequently appearing in the first 2 years if associated with infection. In other cases, such as the one described, the etiological agent may be related with a long-standing infection. Coagulase-negative Staphylococcus are the organisms that cause 60% of femoral APA superinfections, although the bacteriology varies among the different series.5,6 Late-onset degeneration is a complication of polyester vascular prostheses that can lead to their rupture and may be favored by exposure to chronic inflammation (infectious or not) of adjacent tissues as well as individual factors, such as hypertension, anticoagulation, advanced age, obesity and female gender.4,5
Color Doppler ultrasound is an essential non-invasive tool for diagnosis that helps to make the differential diagnosis with other diseases associated with inguinal mass, such as lymphadenopathies, saphenofemoral varices, inguinal or crural hernia (initial diagnosis in this case), hydrocele, lipomas, etc.7 The diagnosis of inguinal hernias (prevalence of 5–15%) is predominantly clinical, so imaging tests have a limited role in patients with nonspecific pain and obesity.8 The presence of a pulsating flow pattern within an inguinal mass is indicative of arterial pseudoaneurysm, and the heartbeat associated with the cardiac cycle (pseudoaneurysm) should be differentiated from the movements associated with the respiratory pattern (inguinocrural hernia simulating a pseudoaneurysm) as has already been published in the literature.9,10
To conclude, in the case of a painful inguinal mass in a patient with a history of vascular intervention in the same location, Doppler ultrasound is recommended prior to manipulating the mass in order to rule out other possible diagnoses.
Please cite this article as: García Blanco VE, Ruales Romero AM, Galera Martínez MC, Dóiz Artázcoz E, Rodríguez Piñero M. Rotura de seudoaneurisma anastomótico de arteria femoral común tras diagnóstico erróneo de hernia inguinal. Cir Esp. 2018;96:459–461.