Pseudomyxoma peritonei (PMP) is a rare disease that is characterized by the production and accumulation of a large amount of mucinous ascites in the abdomen, usually caused by a perforated appendicular neoplasm.1 This intraperitoneal mucin can accumulate through the inguinal canal or other hernia orifice, resulting in symptoms that are indistinguishable from an abdominal wall hernia. Albeit a rare situation, the incidental finding of mucinous material during hernia repair surgery is possible. We present the case of a patient with a diagnosis of PMP discovered during umbilical hernia surgery, and we discuss the general management of this type of patient.
The patient is a 60-year-old woman, with no history of interest, who was referred to our center after the finding of gelatinous ascites with a greater omentum tumor and mucinous implants during umbilical hernia repair. During surgery, a mucinous implant was biopsied, and primary closure of the umbilical aponeurotic defect was carried out. At our hospital, tumor marker levels were determined: CEA 21 and Ca 19-9 650. Thoracic-abdominal-pelvic CT scan showed the presence of diffuse ascites. Gastroscopy and complete colonoscopy were normal. The pathology study of the biopsy reported acellular mucin.
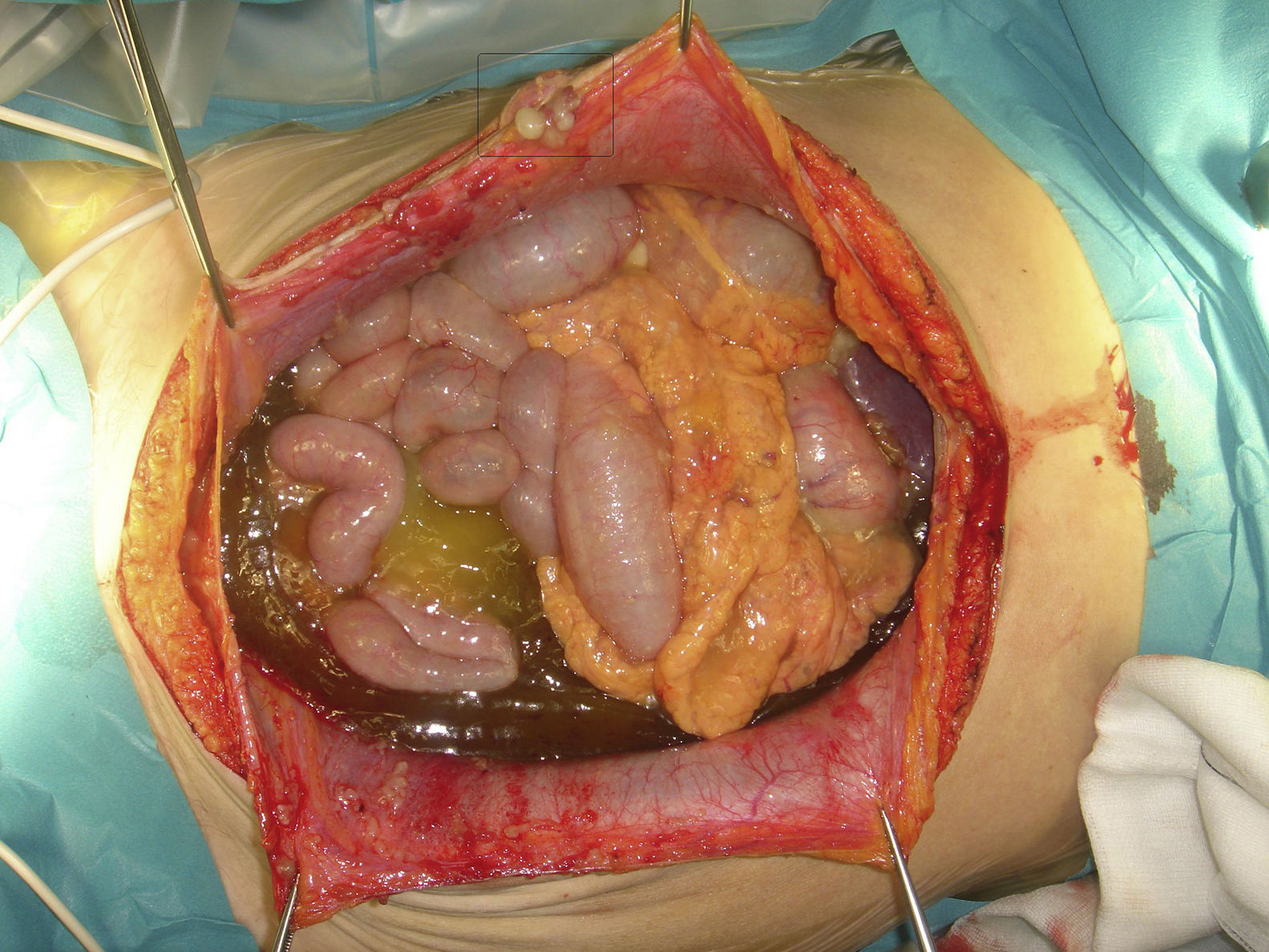
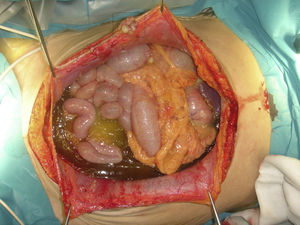
The patient was operated upon, finding a ruptured appendiceal mucinous neoplasm with a peritoneal carcinomatosis index (PCI) of 30 out of 30 (Fig. 1). A pelvic peritonectomy was performed, as well as hysterectomy with double adnexectomy and recto-uterine pouch, right hemicolectomy, peritonectomy of both flanks and right diaphragm with partial resection of the Glisson capsule, major omentectomy with splenectomy, cholecystectomy and cytoreduction of the small intestine implants, as well as omphalectomy that included the scar from previous hernia repair to the aponeurosis. Surgery was completed with hyperthermic intraperitoneal chemotherapy with mitomycin C for 90min at a constant temperature of 42°C. The patient was discharged without incident on postoperative day 10 and is currently disease-free 40 months after surgery. The pathology study confirmed the diagnosis of low grade appendiceal mucinous neoplasm (DPAM).
The most frequent clinical presentation in patients with PMP is progressive abdominal distension.1 The slow increase in intra-abdominal pressure means that this disease can sometimes start as a hernia, most frequently inguinal, which occurs in 25% of men and 5% of women.1
When this finding occurs during abdominal wall hernia repair surgery, the surgeon's approach should be as restrictive as possible, taking samples for histopathology analysis, performing simple closure of the hernia defect and referring the patient to a center specialized in peritoneal oncology surgery for definitive treatment by means of cytoreduction and administration of hyperthermic intraperitoneal chemotherapy (HIPEC).2 The use of mesh, even in large defects, can be accompanied by problems related to the surgical wound, as well as an increase in the scar area facilitating the implantation and growth of tumor cells.2 A recent publication by Sugarbaker found no hernia recurrence in the follow-up of patients undergoing cytoreduction and HIPEC due to PMP who had inguinal hernias. The peritonectomy of the hernia sac and fibrosis of the tract could explain this favorable evolution.3 As for the type of mesh to be used, there is no evidence or consensus in this regard.4
In conclusion, if the PMP is discovered at the time of hernia surgery, a sensible approach would be to take samples, close the aponeurotic defect with no added prosthetic material and refer the patient to a tertiary center experienced in peritoneal oncology for evaluation and specific treatment.
Please cite this article as: Gonzalez-Gil A, Gil J, Cascales-Campos P. ¿Qué hacer cuando se descubre un seudomixoma peritoneal durante la reparación de una hernia de pared abdominal? Cir Esp. 2018;96:120–121.