Información de la revista
Compartir
Descargar PDF
Más opciones de artículo
Letter to the Editor
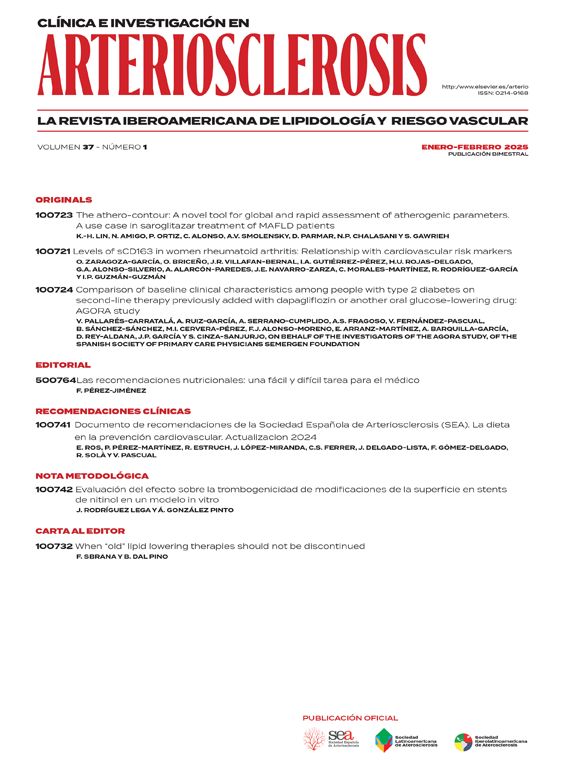
When “old” lipid lowering therapies not should be discontinued
Cuándo no se deben suspender las terapias hipolipemiantes «antiguas»
Visitas
55
Francesco Sbrana
, Beatrice Dal Pino
Autor para correspondencia
Lipoapheresis Unit and Reference Center for Inherited Dyslipidemias, Fondazione Toscana Gabriele Monasterio, Pisa, Italy
Este artículo ha recibido
Información del artículo
Opciones para acceder a los textos completos de la publicación Clínica e Investigación en Arteriosclerosis
Suscriptor
Suscribirse
Comprar
Contactar
Teléfono para suscripciones e incidencias
De lunes a viernes de 9h a 18h (GMT+1) excepto los meses de julio y agosto que será de 9 a 15h
Llamadas desde España
932 415 960
Llamadas desde fuera de España
+34 932 415 960
E-mail