The existence of good coordination between the different levels of care is an essential factor in the development of quality and efficient healthcare. The primary care physician is fundamental in the secondary prevention of cardiovascular disease and the close collaboration between primary care and cardiology is a key factor in the control of cardiovascular disease. The CAPaCERES project (AP-Cardiology Collaboration in Cáceres) aims to improve the coordination between primary care and cardiology from the perspective of mutual knowledge and the improvement of communication between the professionals who develop it, and with that to improve the quality of care chronic patient with cardiovascular disease.
La existencia de una buena coordinación entre los distintos niveles asistenciales constituye un factor fundamental en el desarrollo de una asistencia sanitaria de calidad y eficiente. El médico de atención primaria es fundamental en la prevención secundaria de la enfermedad cardiovascular, y la estrecha colaboración entre atención primaria y cardiología constituye un factor clave en el control de la enfermedad cardiovascular. El proyecto CAPaCERES (Colaboración AP-Cardiología en Cáceres) pretende mejorar la coordinación entre atención primaria y cardiología desde la perspectiva del conocimiento mutuo y la mejora de la comunicación entre los profesionales que la desarrollan, y con ello a mejorar la calidad de la asistencia al paciente crónico con enfermedad cardiovascular.
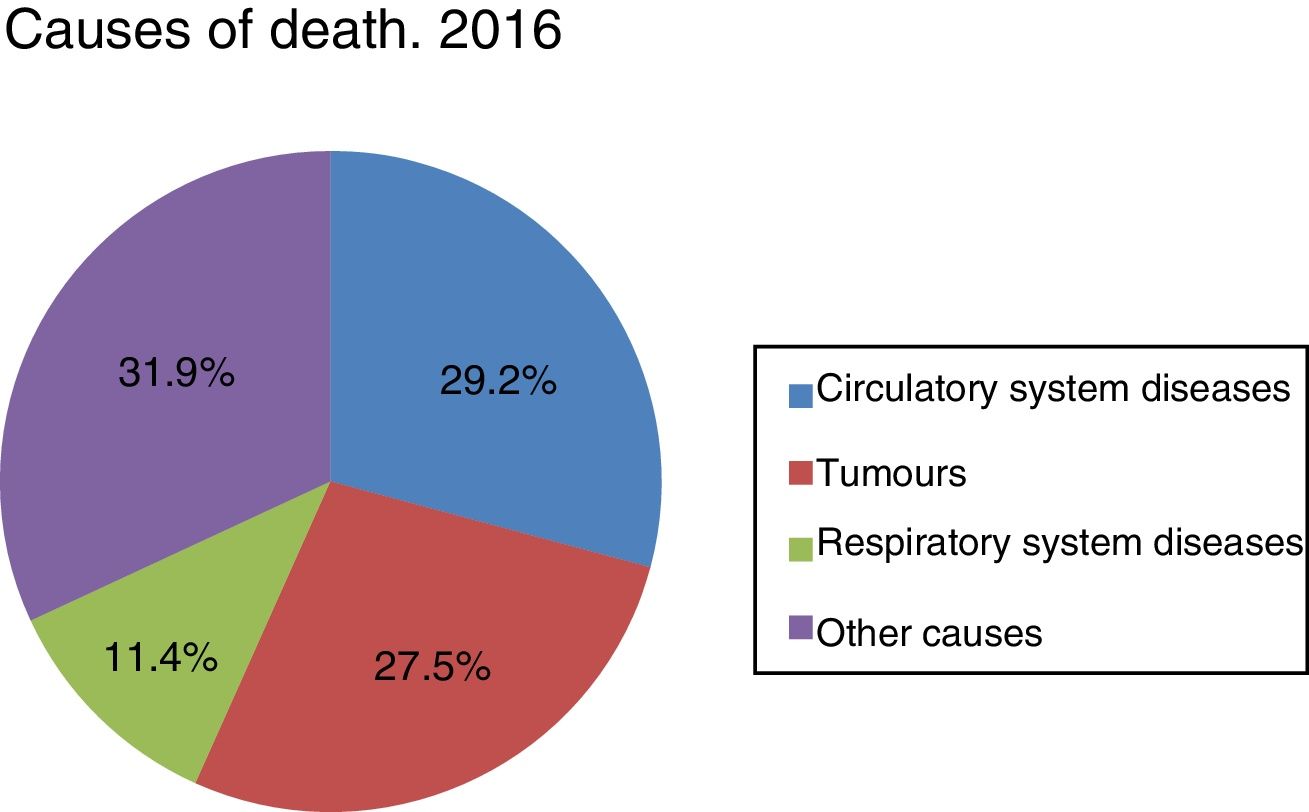
According to the recent report by the Instituto Nacional de Estadística [Spanish National Institute of Statistics] (INE) for 2016 on causes of death in Spain,1 cardiovascular disease (CVD) continues to be the leading cause of death, accounting for 29.2% of all deaths, ahead of cancer (27.5%) and respiratory system diseases (11.4%) (Fig. 1). In spite of this, deaths due to CVD fell by 3.6% on the previous year, and cardiovascular mortality has decreased by more than any other cause in the last ten years, having accounted for 32.5% of all deaths in 2006. This gradual reduction is most likely due to the high level and quality of health care and the introduction of technological and therapeutic innovation leading to increased effectiveness and efficiency of the healthcare system.
Paradoxically, alongside this trend towards lower cardiovascular mortality, there is also an upward trend in the incidence of CVD due precisely to the improvement of treatments and the ageing of the population.
Cardiovascular preventionCVD is largely preventable, so the data shown are indicative of the extensive scope for improvement that remains.
The “cardiovascular disease continuum” is a concept that views CVD as a chain of episodes triggered by a series of related and unrelated cardiovascular risk factors (CVRFs), that progresses via numerous pathways and physiological processes to the development in the terminal stage of coronary heart disease. The significance of this concept is that intervention at any point in the chain of events leading to CVD could alter its progression, stop or slow down the pathophysiological process and protect heart health. In addition, the accumulated scientific evidence indicates that the events that lead to CVD progression are overlapping and interconnected, and do not always occur as a sequence of discrete or in tandem events. Moreover, although the original concept focused on CVRFs for coronary heart disease and its sequelae, the cardiovascular disease continuum has been expanded to include other sites such as cerebrovascular disease, peripheral vascular disease and kidney disease.2
It is known that CVRFs such as hypercholesterolaemia, hypertension, diabetes mellitus and tobacco use promote oxidative stress and cause endothelial dysfunction, triggering a cascade of phenomena that include alterations to vasoactive mediators, inflammatory responses and vascular remodelling, culminating in target organ lesion.3 To control CVD, it is therefore essential to act on CVRFs. The ultimate objective of cardiovascular prevention is to reduce morbidity and mortality and increase the quality of life of patients with CVD by making efficient use of the available resources.
Cardiovascular prevention should be considered and implemented in all social strata and in all healthcare contexts. This must include greater spending on prevention in the health field and on actions that result in a healthier community. All clinicians must consider the prevention and promotion of healthy lifestyles to be a professional responsibility. Patients also need to have the means, knowledge and support to make informed decisions and vigorously demand prevention efforts from healthcare groups and society.4
Clinical practice guidelines (CPGs) recommend a systematic focus for the assessment of the risk, giving priority to people who already have a higher risk. In patients with established CVD, specialised prevention programmes must be implemented, such as cardiac rehabilitation.4 Intensive and structured intervention in general practice contributes to the prevention of recurrent cardiovascular episodes and reduces hospital admissions in patients with CVD.5
Of all the actors playing a role in cardiovascular prevention, primary care (PC) physicians are the key figures to initiate, coordinate and provide long-term follow-up of cardiovascular prevention. In most countries, PC physicians are responsible for more than 90% of consultations, and most public medicine falls to them, including the prevention and monitoring of chronic diseases. In the case of CVD prevention, they play a unique role in identifying people at risk of CVD and deciding on their eligibility for interventions based on their global risk profile. Maximising treatment and adherence rates continues to be a problem, especially in people at higher risk.
With regard to secondary prevention, the PC physician is fundamental in following up patients with CVD, implementing the instructions in the discharge report, performing adequate cardiovascular prevention and not allowing inertia to take over, promoting a healthy lifestyle, and following up and pharmacologically managing acute coronary syndrome. All of this must be done in close collaboration between primary care and cardiology in order to detect and assess changes in clinical status and the course of the disease, modify the therapeutic strategy based on the clinical course, and immediately refer patients with previous heart attacks and suspected heart failure to cardiology for assessment.
The studies conducted among PC and other physicians in different European regions have found that most of them are aware of the existence of CPGs on cardiovascular prevention, but only 36–57% use them, and fewer than half of them perform comprehensive risk assessments. The main obstacle indicated by PC physicians was time, although other factors were also mentioned, such as the excessive number of CPGs, unrealistic targets for control of CVRFs, preference for relying on their own experience and lack of knowledge about the comprehensive risk assessment.6–9 Resources available online, mobile applications, pocket guides and summary tables may contribute to overcoming the challenges with regard to implementation.
On the other hand, a high percentage of patients with cardiovascular disease are treated by other specialties, including, but not limited to, internal medicine, PC or endocrinology. This diversity of specialties often leads to dissatisfaction, delays in care, lack of information in patient follow-up, excessive use of emergency departments or the feeling on the part of PC physicians that they lack information. The routine organisation of care in hospitals—based on fragmented specialties—and PC does not facilitate either continuity of care for patients or the multidisciplinary planning they need.
Communication between levels of careAs a result of all of the above, the existence of good coordination between the different levels of care is a fundamental factor for the development of efficient, quality health care.10,11 The reasons for a lack of coordination between PC and specialist care are diverse, but one that deserves a mention is poor use of protocols, overload in care, excessive administrative bureaucracy, lack of time and other systemic barriers. Nevertheless, there are two closely related and often overlooked qualitative aspects. These are a mutual lack of awareness of the work performed by each professional at the various levels, and poor communication between them.
There are few qualitative studies that analyse the relationships that exist between PC and specialised care professionals, as well as their points of view on the need to improve these relationships.12 In a document by the Department of Health of the Basque Country Regional Government, which analyses coordination between PC and specialised care from the perspective of the professionals, it is established that the most relevant areas for improvement correspond to communication between levels, that the human factor is fundamental to coordination, and that forums for mutual knowledge-sharing between professionals in both groups should be promoted.13
How can we improve communication between levels of care?The aim of our work is to communicate a local project coordinating between PC and cardiology from the perspective of knowledge-sharing and improvement of communication between the professionals involved in it, and thereby to contribute to improving integration between PC and cardiology and, through this, improve the quality of care for chronic patients with CVD.11
The basis for this project was to improve organisational strategy and communication between the different levels of care, and the professionals making up those levels, with regard to the care of patients with CVD.
Routinely, care pressure makes it difficult to find the time needed to facilitate contact and knowledge-sharing between professionals, one of the most significant barriers explaining the lack of communication between levels of care and related by some experts to the mutual lack of awareness and distrust that ultimately hinder the development of quality health care.14
The basic hypothesis that underpins our project rests on the idea that the continuous training intended to update and improve the knowledge, skills and attitudes of healthcare professionals with regard to scientific and technological developments could serve as a vehicle to make it possible to establish tools for communication and knowledge-sharing between healthcare professionals in both groups, with the ultimate aim of improving coordination between PC and cardiology.
The basic pillars of this project were:
- •
Improving the cardiology training of PC physicians, which translates into better implementation of CPGs and optimal referring of patients between specialties. In this regard, the role of the training strategy was to maintain and improve the qualification of PC professionals in the management of patients with CVD and the entire care process that goes along with it through training. The strategy designed rested on two pillars: (a) in-person activities, with the objective of organising clinical sessions and workshops about health targets in secondary prevention, symptomatic management of patients with CVD and the diagnosis of new pathologies; in-person sessions have the advantage that they can generate debate and discussion between the professionals themselves, which without doubt enriches the training, and (b) online training activities that sought to encourage training among professionals working in more isolated centres or for health centres that had difficulty organising in-person activities. Online courses with video tutorials and real practical cases were also offered.
- •
Developing tools for communication between the different levels of care: sharing clinical information and communicating better through knowledge-sharing between professionals through hospital rotations, work shadowing, online clinical sessions and telemedicine, among others.
The ultimate aim of the two strands was to reduce morbidity and mortality among cardiovascular patients and to improve their quality of life, while contributing to the sustainability of the healthcare system.
The CAPaCERES (PC-Cardiology Collaboration in Cáceres) projectThe CAPaCERES project to improve communication between PC and cardiology was launched in 2014 by the Cardiology Department of the Complejo Hospitalario Universitario de Cáceres and PC physicians.
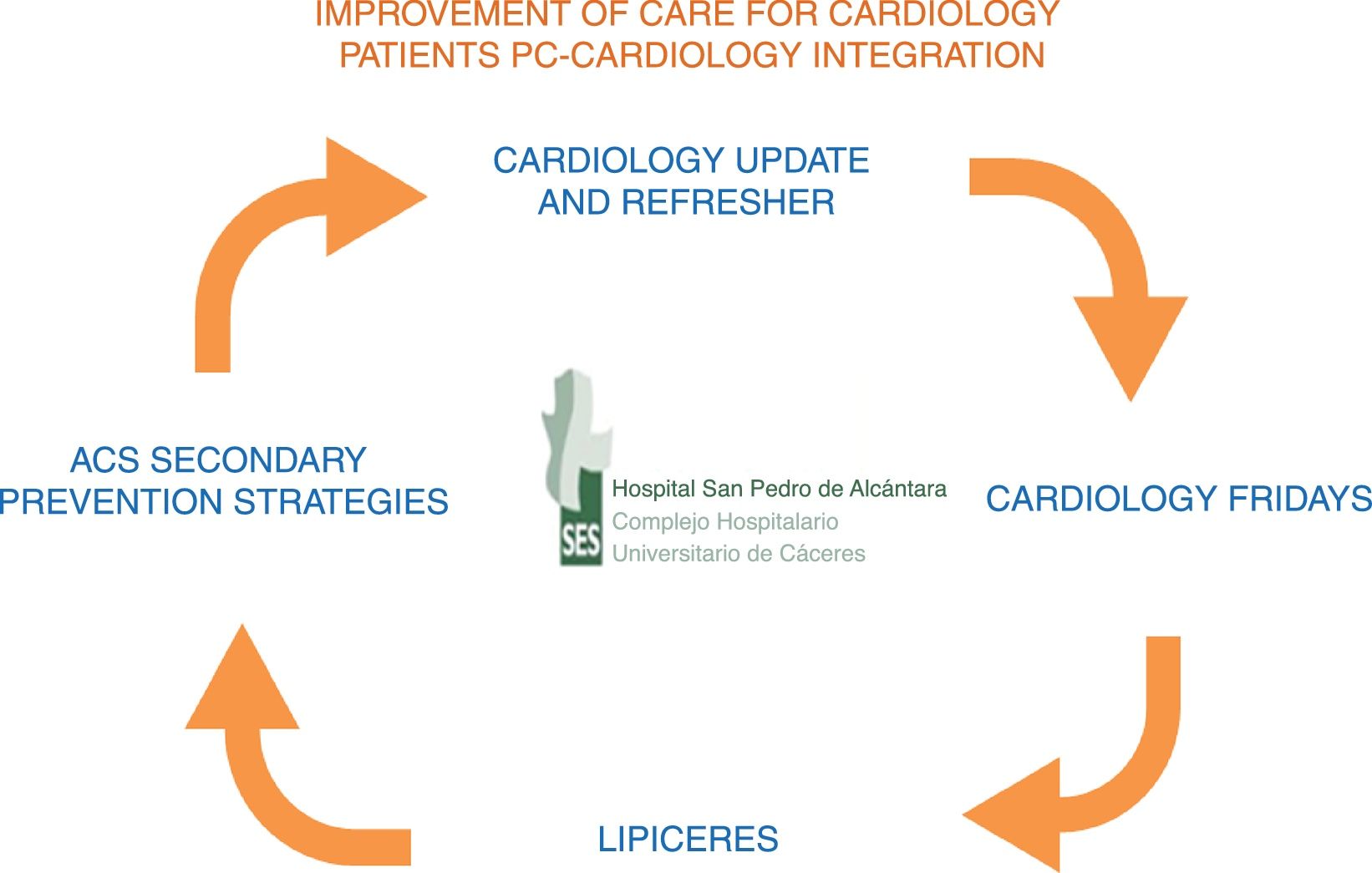
The methodology used consisted of three parts (Fig. 2):
- 1.
The eminently practical and participatory “Cardiology update and refresher programme for PC physicians”, accredited by the Escuela de Ciencias de la Salud de Extremadura [Health Sciences School of Extremadura]. This was held annually for 15 PC physicians each year. It consisted of an initial theory training session during which the coordinating cardiologist explained the programme and members of the cardiology department gave practical presentations on the most prevalent cardiac pathologies, with particular focus on secondary prevention of CVDs. At the end of the programme, a closing session was held in which the PC physicians presented real clinical cases of cardiac pathologies seen in practice and reviewed the subject, followed by a very enriching debate. The practical part of the programme was held over two morning shifts in the cardiology department, rotating through the various areas (ward and consultations) and attendance at daily clinical sessions, with one late shift spent shadowing the cardiologist.
- 2.
Weekly joint clinical sessions held via videoconferencing with a health centre, where case reports from daily practice, ECGs, CPGs or the latest news in cardiology were discussed interactively (which we called “Cardiology Fridays” because of the day they were held on).
- 3.
Improving strategies for the secondary prevention of acute coronary syndrome (ACS), as this is a population at very high cardiovascular risk with elevated mortality and recurrent ischaemic episodes. The actions undertaken were incorporating the recommendations on healthy lifestyle and control of CVRFs in the CPGs in the discharge reports of patients with ACS and raising awareness in PC of cardiac rehabilitation as a comprehensive and multidisciplinary action.
The CAPaCERES project's results are difficult to evaluate due to the use of qualitative variables that are difficult to measure. As an indicator of the immediate results we have measured the satisfaction scores of the professionals with a five-question survey for PC physicians using a five-point Likert scale; all the results were between four and five points. What we can do is extract some impressions that we transcribed at the end as conclusions.
An indirect way to measure the results of this project, with the appropriate reservations, lies in the creation of registries, which are an important tool for epidemiological research and measure the effectiveness of the procedures we apply in a real care setting. An important indicator of cardiovascular health at population level is the degree of control of CVRFs in the patients in our healthcare area shared with PC, above all in those with very high cardiovascular risk, such as those with established CVD.
Recently, in the LIPICERES study,15 we analysed the degree of control of LDL-C during 2013–2015 in 741 coronary patients admitted to the cardiology department over the previous six years. The results demonstrated that the coronary patients at very high risk achieved the therapeutic target of LDL-C <70mg/dl in more than 50% of cases. Never before in Spain had similar control data been published, with lipid control among coronary patients reaching only 26% in previous studies.16 Very recently, the results of the EUROASPIRE V registry17 conducted in 27 European countries during 2016–2017 were presented at the European Atherosclerosis Society Congress; the objective of the EUROASPIRE registry, which has been active since 1995, is to determine how the European CPGs on cardiovascular prevention are implemented in clinical practice in patients with coronary heart disease. The EUROASPIRE V results concerning the overall degree of attainment of the therapeutic target of LDL-C <70mg/dl are 32%, with intensive use of lipid-lowering therapy standing at 60%, while in Spain the degree of lipid control is 49%, which differs wildly from the latest publications in Spain16 and is very similar to the degree of control of the LIPICERES patients.15 We consider these good results—which we already reported in 2017—to be due, at least in part, to an improvement in PC-cardiology coordination in our healthcare area through the CAPaCERES project, the impact of which has been an improved degree of control for coronary patients in our healthcare area.
Towards an integrated care modelThe lack of coordination between PC and specialised care has a negative effect on continuity of care. It brings along with it significant and unfavourable implications such as increased delays in care, lack of information on patient follow-up, the use of the “emergency pathway” to meet needs, unjustified referrals to hospital care, patient misinformation, medical errors and unnecessary repetition of diagnostic procedures.
In an attempt to improve coordination between levels, various initiatives have been carried out in recent years, among which it is worth noting the integration of the consulting cardiologist within the health centre, the creation of joint action protocols, update sessions, the optimisation of communication channels and systems, the improvement of clinical reports both at hospital discharge and in consultations, and electronic medical record sharing, among others. The shared aim of all these strategies lies in achieving better integration between cardiology and PC, and all have had positive results for heart disease patients.11,18,19
In view of these local initiatives for coordination between cardiology and PC, which have all given such good results in their respective healthcare areas, the Sociedad Española de Cardiología [Spanish Society of Cardiology] has established as one of its strategies the SEC-PRIMARIA project, which has the ultimate objective of reducing mortality and improving the quality of life of heart disease patients, with efficient use of the available resources, by improving the use of care protocols and communication between the different levels of care in the context of the PC-hospital relationship.20
ConclusionsKnowledge-sharing among professionals is an essential factor for integration between levels of care. Cardiology department rotations for PC physicians and joint participation in training sessions facilitate close communication between cardiologists and PC physicians, while also serving as a potential teaching tool.
Improved reciprocal knowledge, the establishment of communication channels and shared continuous training undoubtedly contribute to improving professionals’ satisfaction and their assessments of care quality for patients with chronic cardiovascular disease.
The results of this coordination can be seen in the degree of implementation of the CPGs, which is essentially reflected in the degree of attainment of CVRF control targets and adherence to treatment.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Gómez-Barrado JJ, Gómez-Turégano P, Ortiz-Cortés C, Lezcano-Gort LE, Kounka Z, Romero-Castro MJ. Comunicación entre niveles asistenciales: una oportunidad de mejora en la prevención cardiovascular. Clín Investig Arterioscler. 2018. https://doi.org/10.1016/j.arteri.2018.09.003