Physical exercise has become in an important tool in the reduction of cardiovascular risk.
ObjectivesTo evaluate the effectiveness of an unsupervised physical exercise programme that on the physical condition and the lipid profile.
MethodThe final sample included 49 sedentary men and women, who were non-smokers, with dyslipidaemia, overweight, and type 1 obesity. The 4-month programme included walking for 30–60min every day, and for three days a week, 30min of cycling at an intensity of 40–60% of maximum functional capacity, as well as isometric abdominals and static stretching. Anthropometrics, physical condition (6min test), and the lipid profile were evaluated before and after the physical exercise programme. The objective was to achieve a caloric expenditure between 1200 and 2000kcal/week.
ResultsAt the end of the programme it was observed, in both sexes, that there was a decrease in total cholesterol (p<0.02), LDL cholesterol (p<0.01), VLDL cholesterol (p<0.01), and triglycerides (p<0.05), and an increase HDL cholesterol (p<0.05). There was also an increase in the distance travelled in the 6min test of 52m in men and 39.5m in women (p<0.002), plus a decrease in the perception of fatigue on the Borg scale of 1.19 in men, and 0.96 in women (p<0.01). There were no anthropometric changes.
ConclusionsThe physical exercise improved physical condition and the lipid profile in the sample that has been studied, with 64% of participants continuing to do it.
El ejercicio físico (EF) se ha convertido en una herramienta de capital importancia en la reducción del riesgo cardiovascular (RCV).
ObjetivosEvaluar la eficacia de un programa de EF no supervisado sobre la condición física y el perfil lipídico.
DiseñoLa muestra final incluyó a 49 hombres y mujeres sedentarias con dislipemia, sobrepeso u obesidad tipo1 y no fumadores. Debían realizar durante 4meses: andar 30-60min cada día y 3días a la semana: 30min de bicicleta estática a una intensidad del 40-60% de la capacidad funcional máxima, abdominales isométricos y estiramientos estáticos. Antes y después de realizar el programa de EF se evaluó la antropometría, la condición física (Test de los 6min) y el perfil lipídico. El objetivo era conseguir un gasto calórico entre 1.200-2.000kilocalorías/semanales.
ResultadosAl finalizar el programa se observó en ambos sexos una disminución del colesterol total (p<0,02), del colesterol LDL (p<0,01), del colesterol VLDL (p<0,01), de los triglicéridos (p<0,05) y un aumento del colesterol HDL (p<0,05). También se constató un aumento de la distancia recorrida en el test de los 6min: hombres 52m (p<0,002) y mujeres 39,5m (p<0,002) y una disminución de la percepción de fatiga (escala de Borg): hombres en 1,19 (p<0,01) y mujeres en 0,96 (p<0,01). No hubo cambios antropométricos.
ConclusionesEl EF prescrito mejoró el perfil lipídico (alcanzando al final del estudio valores dentro de los rangos de normalidad) y la condición física en la muestra estudiada. Se consiguió una adherencia al mismo de un 64% de los participantes.
Atherosclerosis is a very common disease in our society and it is a serious threat to health. Clinical expressions of atherosclerosis are a varied collection of diseases, including ischaemic cardiomyopathy (myocardial infarction, angina, arrhythmia, syncope, sudden death, etc.), cerebrovascular accident and peripheral artery disease.1
Without a doubt, physical exercise (PE) has become a very important strategy not only in primary and secondary prevention of all of these, but also essential to achieving a healthier lifestyle.
Like diet, physical activity is another easily modifiable factor, with a clearly favourable effect on blood lipid concentrations.
There is an inverse dose–response relationship; thus, increasing physical activity is associated with proportionally lower rates of cardiovascular disease (CVD).2,3 It has been estimated that if physical inactivity is eliminated, heart disease would be reduced by 6% worldwide and life expectancy could increase by 0.68 years.4
The practice of PE has a positive effect on pathogenesis, symptoms and the physical shape of people with lipid profile abnormalities. Even improved physical condition, irrespective of weight loss, has a beneficial effect on the lipid profile.5
PE is associated with the following favourable changes:
- •
Increases HDL cholesterol (HDL-C) values by 5–14%, especially the HDL2 and HDL3 sub-fractions.6–8
- •
Decreases triglycerides (TG) by 7–15%.8
- •
Decreases LDL cholesterol (LDL-C), although not consistently in all studies (0–15%).8
- •
Increases HDL-C/LDL-C and HDL-C/total cholesterol (TC) ratios.8
- •
Decreases TC, VLDL cholesterol (VLDL-C) and apolipoprotein B by 7–18%.8
- •
Reduces the number and size of TG-rich lipoproteins.8
- •
Modifies the LDL-C pattern, changing to larger and less atherogenic particles.8
Exercise has the greatest benefit on HDL-C (as long as the person does not smoke, since the positive effect would be cancelled out by nicotine) in sedentary people 3–6 months after starting the exercise programme, which is further enhanced the greater the lipid abnormality.1
The effects of a physical activity programme are different depending on its type, intensity, frequency and duration.9
The regular practice of moderate-intensity aerobic PE along with favourable changes in the lipid profile is associated with a lower risk of coronary artery disease and cardiovascular mortality.10
A minimum weekly expenditure of 1200cal is required to achieve significant changes in the lipid profile,11 and an expenditure of 1500cal per week is necessary to achieve changes in the HDL2 sub-fraction. In individuals with atherosclerosis without lipid-lowering medication, expenditure of 2200kcal/week is required to generate certain atherosclerotic plaque regression benefits.12
The effect of physical activity on HDL-C is less than that which is achieved with lipid-lowering drugs.7
The positive effects of exercise on lipids are similar both in people with normal cholesterol levels and in those with high cholesterol.11
The accumulated epidemiological evidence suggests a dose–response relationship between the positive changes in lipid profile and the volume of exercise rather than the intensity, since a decrease in the LDL-C/HDL-C and TC/HDL-C ratios has been reported, as well as a linear increase in HDL-C when increasing distance covered.13,14
The objectives of this study were to evaluate the impact of an unsupervised PE programme on lipid profile and physical condition, in a sample of sedentary men and women with dyslipidaemia, who are overweight or have class 1 obesity, and do not smoke.
Material and methodsSubject screeningThe studied sample comprised 77 patients referred from other departments of the Hospital Universitario Sant Joan de Reus to the Sports Medicine Unit of the same hospital. Twenty-eight (28) patients were excluded due to not having completed the prescribed PE or not having come to the final evaluation; therefore the results were analysed for 49 patients (24 men and 25 women).
All patients, between the ages of 21 and 77 years, were seen at the Clinical Physiology practice of the Sports Medicine Unit. They were also sedentary (less than 30min per day of regular exercise, fewer than three days per week), non-smokers for more than one year and were overweight or had class 1 obesity and dyslipidaemia in the upper limit range. Patients with diagnosed psychiatric diseases, drug dependencies, oncological diseases or heart disease were excluded. The usual medication and diet of the patients were not modified.
Procedures and materialThe sample size was calculated based on the primary endpoint, the Six-Minute Walk Test, in which, based on a minimum of 371metres (m) per participant, an improved prognosis was shown if the subject increased their distance by 40m. Therefore, the sample had to include at least 35 participants.15,16
Informed consent was requested from each patient to participate voluntarily in the study and to use their biomedical data.
This study was conducted in accordance with the Declaration of Helsinki and the International Conference of Harmonization (ICH) Good Clinical Practice guidelines.
Prior to the start of the exercise programme, a sports physical examination was performed, which included:
- •
Patient history, examination using instruments, measuring of blood pressure, ECG at rest and anthropometry: weight (Año Sayol Scales, 0–150kg, 100g precision), height (Año Sayol height rod, 55–200cm, 1mm precision), body mass index (BMI) and bioelectrical impedance analysis (Body Composition Analyzer, Type BC-418 MA III), which calculates the body fat percentage (fat %).16
- •
Six-Minute Walk Test following the procedures indicated in the scientific literature, on a marked walkway longer than 30m.17 The distance covered was measured. The following were also assessed before and after the test: blood pressure, heart rate, oxygen saturation and, at the end of the test, perceived exertion (Borg scale).18 Material: Riester sphygmomanometer. Casio stopwatch. Philips SureSigns VS3 vital signs monitor (pulse oximeter, heart rate). Borg visual analogue scale (1–12).
- •
Eight-hour fasting blood test: complete blood count, glucose, TC, HDL-C, LDL-C, VLDL-C and TG. These were determined using enzymatic methods with Olympus AU 5400 analysers (Olympus Diagnostica, Hamburg, Germany). The analyses were conducted in accordance with the recommendations of the Sociedad Española de Arteriosclerosis (Spanish Arteriosclerosis Society, SEA).19
- •
Four-month Exercise Programme, which comprised: walking 30–60min daily in 10–15min sessions, exercise bike three days/week, 30min/session, at an intensity of 40–60% of maximum functional capacity (heart rate reserve), isometric abdominal exercises and static stretches. The objective was to achieve caloric expenditure between 1200 and 2000kcal/week.
Throughout the four months of the PE programme, monthly visits were completed to assess adherence to the exercise plan and to motivate the participants, while also checking that no medical problems of interest had arisen.
At the end of the study, after the four-month PE programme, the anthropometric study, the blood tests and the Six-Minute Walk Test were repeated with the same methodology described.
StatisticsMean and standard deviation of each parameter studied. To compare the evolution of the parameters of each sample, the data were processed with Student's t-test to compare means of paired data. To compare parameters in different samples (men vs women), Student's t-test was used to compare unpaired data means, and the two controls were verified using Wilcoxon's matched-pairs signed-rank (non-parametric) test. The statistical package used was SPSS version 19.0 for Windows. p<0.05 was considered positive.
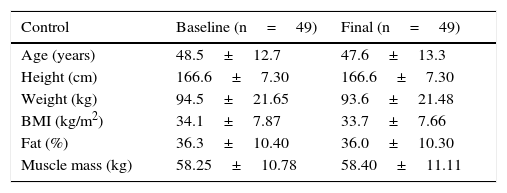
ResultsTable 1 shows the demographic and anthropometric characteristics of the sample. Weight, BMI and body fat percentage decreased slightly, which was not statistically significant.
Demographic and anthropometric characteristics of the sample.
| Control | Baseline (n=49) | Final (n=49) |
|---|---|---|
| Age (years) | 48.5±12.7 | 47.6±13.3 |
| Height (cm) | 166.6±7.30 | 166.6±7.30 |
| Weight (kg) | 94.5±21.65 | 93.6±21.48 |
| BMI (kg/m2) | 34.1±7.87 | 33.7±7.66 |
| Fat (%) | 36.3±10.40 | 36.0±10.30 |
| Muscle mass (kg) | 58.25±10.78 | 58.40±11.11 |
BMI: body mass index; SD: standard deviation.
Averages±SD.
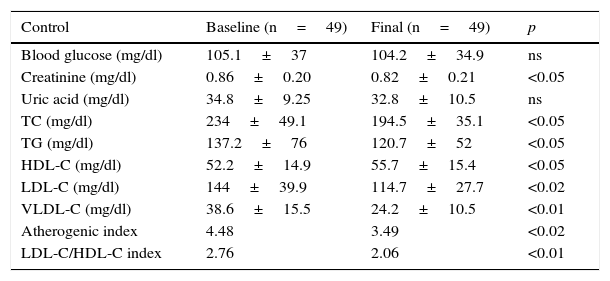
Upon analysing the lipid profile, a significant decrease in TC (p<0.05), LDL-C (p<0.02), VLDL-C (p<0.01), TG (p<0.05) and lipid index (p<0.02), and an increase in HDL-C (p<0.05) were observed in the sample as a whole, as shown in Table 2.
Evolution of laboratory values.
| Control | Baseline (n=49) | Final (n=49) | p |
|---|---|---|---|
| Blood glucose (mg/dl) | 105.1±37 | 104.2±34.9 | ns |
| Creatinine (mg/dl) | 0.86±0.20 | 0.82±0.21 | <0.05 |
| Uric acid (mg/dl) | 34.8±9.25 | 32.8±10.5 | ns |
| TC (mg/dl) | 234±49.1 | 194.5±35.1 | <0.05 |
| TG (mg/dl) | 137.2±76 | 120.7±52 | <0.05 |
| HDL-C (mg/dl) | 52.2±14.9 | 55.7±15.4 | <0.05 |
| LDL-C (mg/dl) | 144±39.9 | 114.7±27.7 | <0.02 |
| VLDL-C (mg/dl) | 38.6±15.5 | 24.2±10.5 | <0.01 |
| Atherogenic index | 4.48 | 3.49 | <0.02 |
| LDL-C/HDL-C index | 2.76 | 2.06 | <0.01 |
Atherogenic index: TC/HDL-C; HDL-C: HDL cholesterol; LDL-C: LDL cholesterol; ns: not significant; TC: total cholesterol; TG: triglycerides; VLDL-C: VLDL cholesterol.
Student's t-test, comparison of means, paired data; means±SD.
Statistical significance: p<0.05.
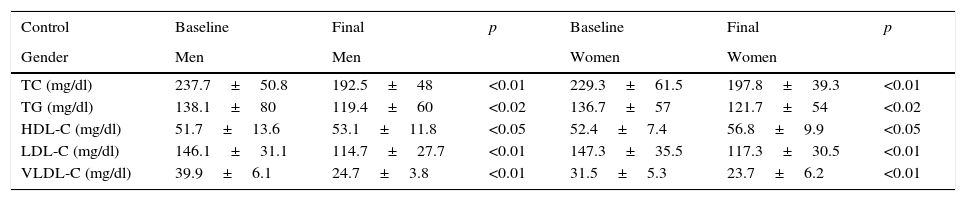
Table 3 presents the results of the gender analysis, and in both men and women similar changes occurred, with a significant decrease in TC (p<0.01), LDL-C (p<0.01), VLDL-C (p<0.01) and TG (p<0.02), and a significant increase in HDL-C (p<0.05).
Evolution of lipid profile by gender.
| Control | Baseline | Final | p | Baseline | Final | p |
|---|---|---|---|---|---|---|
| Gender | Men | Men | Women | Women | ||
| TC (mg/dl) | 237.7±50.8 | 192.5±48 | <0.01 | 229.3±61.5 | 197.8±39.3 | <0.01 |
| TG (mg/dl) | 138.1±80 | 119.4±60 | <0.02 | 136.7±57 | 121.7±54 | <0.02 |
| HDL-C (mg/dl) | 51.7±13.6 | 53.1±11.8 | <0.05 | 52.4±7.4 | 56.8±9.9 | <0.05 |
| LDL-C (mg/dl) | 146.1±31.1 | 114.7±27.7 | <0.01 | 147.3±35.5 | 117.3±30.5 | <0.01 |
| VLDL-C (mg/dl) | 39.9±6.1 | 24.7±3.8 | <0.01 | 31.5±5.3 | 23.7±6.2 | <0.01 |
HDL-C: HDL cholesterol; LDL-C: LDL cholesterol; TC: total cholesterol; TG: triglycerides; VLDL-C: VLDL cholesterol.
Student's t-test, comparison of means, paired data; means±SD.
Statistical significance: p<0.05.
At the beginning of the study, the entire sample, and the sample differentiated by gender had TC, LDL-C and VLDL-C levels above normal ranges, while after the study, the values were within normal ranges.20 The HDL-C and TG values both overall and differentiated by gender were normal before and after the study.
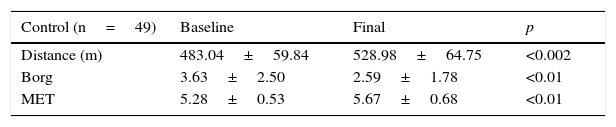
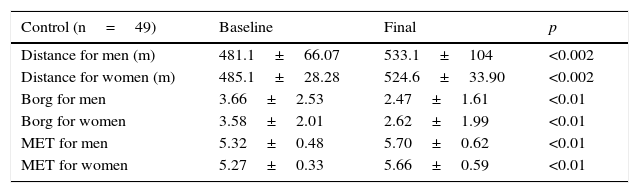
Physical conditionTable 4 records the improved distance covered (in metres) by the entire sample assessed by the Six-Minute Walk Test (p<0.002), the evolution in perceived exertion assessed using the Borg visual analogue scale (p<0.01) and the variations in metabolic equivalents (MET) at the beginning and end of the exercise programme (using formulas derived from the Six-Minute Walk Test) (p<0.01).21
Six-Minute Walk Test. Evolution of distance and perceived exertion.
| Control (n=49) | Baseline | Final | p |
|---|---|---|---|
| Distance (m) | 483.04±59.84 | 528.98±64.75 | <0.002 |
| Borg | 3.63±2.50 | 2.59±1.78 | <0.01 |
| MET | 5.28±0.53 | 5.67±0.68 | <0.01 |
Borg: perceived exertion scale; MET: metabolic equivalent.
Student's t-test, comparison of means, paired data; means±SD.
Statistical significance: p<0.05.
Table 5 shows the above variables by gender, as well as the findings from the entire sample; differences between the first and second measurement are statistically significant.
Six-Minute Walk Test. Evolution of distance, perceived exertion and MET.
| Control (n=49) | Baseline | Final | p |
|---|---|---|---|
| Distance for men (m) | 481.1±66.07 | 533.1±104 | <0.002 |
| Distance for women (m) | 485.1±28.28 | 524.6±33.90 | <0.002 |
| Borg for men | 3.66±2.53 | 2.47±1.61 | <0.01 |
| Borg for women | 3.58±2.01 | 2.62±1.99 | <0.01 |
| MET for men | 5.32±0.48 | 5.70±0.62 | <0.01 |
| MET for women | 5.27±0.33 | 5.66±0.59 | <0.01 |
Borg: perceived exertion scale; MET: metabolic equivalent.
Student's t-test, comparison of means, paired data; means±SD.
Statistical significance: p<0.05.
Although there are no significant differences when comparing between genders, men made the biggest improvements.
An improvement of at least 35m in the Six-Minute Walk Test is a substantial change with clinical significance.16 This improvement occurred both in the studied sample as a whole and differentiated by gender.
An increase in the distance covered was seen, with an average improvement of 45.94m (p<0.002), with marked differences observed between the distances covered by men and by women, although not statistically significant, as well as a decrease in perceived exertion on the Borg scale (p<0.01).
We also observed an improvement in physical condition that, although slight, was statistically significant, expressed in MET (p<0.01).
DiscussionAs in previous studies conducted at our site in patients with similar characteristics, it was observed that a large number of subjects recruited for the study withdrew: 28 subjects out of a total of 77, 36% of the initial sample. Given that this is a clinical study, the importance of adherence to the regular practice of therapeutic PE by patients becomes a significant problem to consider. Adherence to the PE programme in this study was 64%.
The monthly check-ups, in addition checking for any abnormalities that could arise, are also a motivational support and a good tool to ensure adherence over time to the PE programme.
We propose an easy-to-prescribe PE programme that does not require complicated or complex additional tests and is easy to follow by the patients for whom it is intended, both in the type of exercise to perform and in intensity (it must be remembered that these are sedentary patients). An increase in caloric exertion between 1200 and 2000kcal per week should be aimed for in order to achieve positive changes in the lipid profile.
AnthropometryA trend towards improvement was observed in the anthropometric data but it was much less marked than in the other parameters evaluated, although recent studies highlight that improvement in physical condition is more important for health and decreasing cardiovascular risk (CVR) than anthropometric data.22 This study did not include the measurement of waist circumference, a measurement that would probably better reflect the changes that occurred in intra-abdominal fat and body composition in the study subjects.
Lipid profileIn a 2007 meta-analysis which studied the effect of training on HDL-C, the observed minimum amount of physical activity necessary to cause a positive effect was 120min per week to achieve an expenditure of 903kcal/day. The duration was more important than intensity; thus, for each 10min in increased duration, the HDL-C level increased by an average of 1.4mg/dl.
Various studies have shown that partaking in sports such as football and volleyball, in which the exercise is intermittent and of high intensity with 60% and 70% aerobic periods, respectively, with the high joint impact and eccentric contractions, can exponentially increase the risk of CVD, since high values of LDL-C, ApoB and lipoprotein (a) have been found.23
Conversely, activities such as swimming, which involve continuous exercise with 95% aerobic periods, concentric muscle contractions and low joint impact would be beneficial for the lipid profile.23
Various factors could explain these discrepancies: baseline serum lipid and lipoprotein levels and their methods of analysis, the different physical conditions of the subjects and their maximum oxygen consumption (VO2 max), body weight and percentage of body fat, ethnicity, gender, age and the characteristics of the exercise practised (type, volume, duration and intensity), dietary changes or lack thereof and the use or non-use of lipid-lowering drugs.
The improvement in lipid profile in sedentary patients with dyslipidaemia, when adherence is achieved, occurs with resistance exercise, with the combination of strength and resistance, and with diet and physical activity recommendations.24
Beta-adrenergic sensitivity must increase in adipose tissues, causing greater consumption of fatty acids as a source of energy. This adaptive phenomenon reaches its peak four months after having started a resistance training programme.
If we consider that the lipid and apolipoprotein response to PE extends up to 48h after the PE, when prescribing exercise, the frequency should be at least one session every 48h to maintain responses over time and obtain the necessary metabolic adaptations over months.
The presence of other CVRFs, such as obesity, diabetes and high blood pressure, may require modifications in the PE prescription.
When dyslipidaemia is of genetic origin, the PE will have little or no effect on lipids, but even in these patients, changes continue to occur that will benefit their health.
Just as occurred in the sample in this study, in overweight and obese adults, the increase in HDL-C occurred with both moderate and vigorous physical activity, while low-intensity PE would be sufficient to decrease the LDL-C level.
There is no consensus—and the level of evidence is low—regarding the influence of strength exercises on the lipid profile, with published cases of both decreases and increases in HDL-C and decreases in TG and LDL-C without effect on HDL-C.24
Although the results of recent meta-analyses and systematic reviews indicate that PE, when done with sufficient frequency and intensity, induces favourable changes in LDL-C and HDL-C, more research is necessary to better understand exercise patterns (frequency, lesser intensity, type of exercise) that may be associated with improvements in lipid profile.
Overall, the patients (both men and women) included in this study improved their lipid profiles, reaching TC, LDL-C and VLDL-C levels within reference ranges considered optimal.
Physical conditionThe scientific evidence recognises that physical condition is an excellent predictor of life expectancy and quality of life. In recent years, numerous studies have shown an inverse association between physical condition and morbidity and mortality in the population, which is particularly striking in patients with CVRFs. Improvements were observed not only in physical health, but also in mental health: self image, self control and anxiety.25–27
An almost linear relationship was observed between the decrease in mortality and improved physical condition (MET). Thus, each MET of improvement leads to a 12% increase in life expectancy in men and 17% in women.25–27
Current studies show the prognostic value of the results obtained from the Six-Minute Walk Test. In subjects that covered shorter distances, a greater risk of all-cause mortality, especially from CVD, heart failure and dementia are observed. The risk increases significantly when the distance covered is less than 400m, remaining high with distances less than 460m.28
Thus, according to these studies, poor physical condition (as assessed by the Six-Minute Walk Test), as presented by our patients at the beginning of the study, is an added CVRF, in addition to being a predictor of morbidity and mortality.
In this study, the initial average distance covered in metres (483.04±59.84) is lower than the values found in the literature for patients in the same age range (average of 531±74m). With the improvement that patients experienced after the re-training period, the distance covered in metres (average of 528.98±64.75m) is close to the theoretical reference distance considered normal in patients.29
The Six-Minute Walk Test essentially assesses endurance or cardiorespiratory resistance, that is, exercise tolerance, which is potentially of greater interest in patients enrolled in this study, given that it defines the aptitude to work regularly at a sub-maximal percentage of VO2 max.
From a functional point of view, the endurance (aerobic resistance) quality of patients is more useful than the quality of performance, given that it allows for greater adaptation to the energy demands of daily life.
In the studies referenced, there are clear differences in the distance covered between men and women, with values that vary between 59 and 84m in favour of men.29 In this study, the distance covered at baseline was low and similar for men (481.6±66.07m) and women (485.1±28.28m), while after the exercise period, although both subgroups improved, men improved by an average of 52±60m, while women only improved by an average of 39.5±41m.
Although the improvement is within the theoretical estimated optimal range for patients for both genders (31–75m), in women, the recommendations, motivation and follow-up should be reinforced. It is important to mention that these reference data are from studies of patients with pulmonary conditions, therefore they may not fully correspond to the characteristics of the sample in this study, but they are the only data available, or at least to which we had access at the time.29
A slight but significant improvement was observed in the calculated maximum MET (increase of 0.35±0.39 MET on average). The data indicate that both aerobic potential (to a lesser extent) and endurance (to a greater extent) improved.
This increase in aerobic potential and endurance is very evident in the improvement in perceived exertion measured using Borg's scale.
The experience acquired over the years, along with the data collected and references consulted, lead us to consider the need to include evaluation of physical condition and prescription of PE globally and systematically in the treatment of patients with CVRFs, together with clinical follow-up.
Based on the available data, people with dyslipidaemia should perform PE at an intensity of 40–70% of heart rate reserve (HRR) or 60–85% of maximum heart rate or 55–75% of VO2 max, for 60min per day, 5 days per week, and maintain it throughout their lives, given that the effects on lipid metabolism are reversible and can disappear.7,30,31
One of the causes attributable to the lack of weight loss could be that the caloric exertion of the PE programme conducted was less than 2000kcal/week.
Despite the heterogeneity of the sample, the prescribed PE achieved positive changes in physical condition and lipid profile.
Although it was not done in this study, we believe it is necessary to measure waist and hip circumference.
ConclusionsAn individualised, unsupervised PE programme is economical, easy to do and achieves good adherence (64%) from participants.
In our studied sample, both genders achieved improvements in the lipid profile: decreased TC, LDL-C, VLDL-C and TG and an increase in HDL-C, reaching values within normal limits by the end of the study.
Aerobic strength (MET) and, more strikingly, aerobic resistance-exercise tolerance slightly improved, while perceived exertion decreased.
A slight, insignificant decrease in weight and BMI was also observed. This could potentially improve with dietary recommendations.
As a result of the improvement in lipid profile and physical condition, CVRFs will decrease and the morbidity and mortality and quality of life of these patients will improve.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed adhere to the ethical standards of the responsible human experimentation committee and are to the World Medical Association and the Declaration of Helsinki.
Confidentiality of dataThe authors declare that they have followed their centre's protocols regarding the publication of patient data.
Right to privacy and informed consentThe authors have obtained informed consent from the patients and/or subjects referred to in this article. This document is held by the corresponding author.
Conflicts of interestThe authors declare that there are no conflicts of interest.
Please cite this article as: Rubio Pérez FJ, Franco Bonafonte L, Ibarretxe Guerediaga D, Oyon Belaza MP, Ugarte Peyron P. Efecto de un programa de ejercicio físico individualizado sobre el perfil lipídico en pacientes sedentarios con factores de riesgo cardiovascular. Clin Invest Arterioscler. 2017;29:201–208.