To evaluate whether there were any differences in the risk factor profile associated with either the intima-media thickness (IMT) or the presence of carotid plaques.
MethodsCross-sectional study in 1475 subjects between 45 and 75years, randomly selected from the population of the Northwest area of Madrid (Spain). They had a physical exam, blood analysis, and ultrasound measurement of the IMT and of the presence of plaques.
ResultsMean IMT was 0.725±0.132mm. Forty seven percent of the participants had carotid plaques. In multivariate analysis, factors directly associated with the IMT were, age (β0.227, p<0.0001), sex (β0.104, p<0.0001), presence of hypertension (β0.082, p=0.002), diabetes (β0.130, p<0.0001) and current smoking (β0.107, p<0.0001), systolic blood pressure (SBP) (β0.219, p<0.0001) and LDL-cholesterol levels (β0.074, p=0.003), and inversely, diastolic blood pressure (DBP) (β−0.124, p=0.001), HDL-cholesterol (β−0.111, p<0.0001) and triglyceride levels (β−0.060, p=0.028). The presence of plaques was directly associated with age (OR 1.08; 95% CI: 1.05–1.10), sex (OR 1.95; 95% CI: 1.52–2.51), current smoking (OR 2.75; 95% CI: 1.92–3.95), history of hypertension (OR 1.58; 95% CI: 1.22–2.04) or diabetes (OR 1.84; 95% CI: 1.31–2.58), statin treatment (OR 1.56; 95% CI: 1.19–2.04) and SBP (OR 1.03; 95% CI: 1.02–1.05), and inversely with DBP (OR 0.98; 95% CI: 0.96–0.99).
ConclusionFactors associated with the IMT and the presence of plaques are similar, a finding that support a continuum between muscular layer hypertrophy and arteriosclerosis development.
Evaluar si existen diferencias en el perfil de factores de riesgo asociados con el grosor íntima-media (GIM) y la presencia de placas carotídeas.
MétodosEstudio transversal de base poblacional, en 1.475 sujetos de entre 45 y 75años de edad, seleccionados de forma aleatoria de los registros de Atención Primaria del área noroeste de Madrid. Se les realizó una exploración física, una analítica y se les determinó el GIM en carótida común y la presencia de placas mediante ecografía.
ResultadosEl GIM medio de la población fue de 0.725±0,132mm. El 47% presentaban placas carotídeas. En el análisis multivariante, los factores relacionados con el GIM fueron: edad (β0,227, p<0,0001), sexo (β0,104, p<0,0001), presencia de hipertensión (β0,082, p=0,002), diabetes (β0,130, p<0,0001) y tabaquismo activo (β0,107, p<0,0001), presión arterial sistólica (PAS) (β0,219, p<0,0001) y concentración de colesterol LDL (β0,074, p=0,003), y de forma inversa, presión arterial diastólica (PAD) (β−0,124, p=0,001) y concentraciones de colesterol HDL (β−0,111, p<0,0001) y triglicéridos (β−0,060, p=0,028). La presencia de placas se asoció de forma directa con edad (OR1,08; IC95%: 1,05-1,10), sexo (OR1,95; IC95%: 1,52-2,51), tabaquismo activo (OR2,75; IC95%: 1,92-3,95), antecedente de hipertensión (OR1,58; IC95%: 1,22-2,04) y de diabetes (OR1,84; IC95%: 1,31-2,58), consumo de estatinas (OR1,56; IC95%: 1,19-2,04) y PAS (OR1,03; IC95%: 1,02-1,05), y de forma inversa con PAD (OR0,98; IC95%: 0,96-0,99).
ConclusiónLos factores de riesgo asociados con el GIM y la presencia de placas son similares, un dato que apoya el continuo entre la hipertrofia de la capa muscular y el desarrollo de arteriosclerosis.
Numerous epidemiological studies have shown a direct relationship between the presence of carotid atherosclerosis, evaluated by measuring the intima-media thickness (IMT) or the presence of plaque, and the development of cardiovascular complications and death.1–3 It is estimated that for every 0.1mm increase in carotid IMT, the risk of myocardial infarction increases by 15% and the stroke risk increases by 18%.4 Likewise, carotid plaque increases the risk of infarction, stroke and death to varying degrees according to studies.5 Measuring IMT as a predictor of cardiovascular risk has also been evaluated in terms of changes over time.6,7
The clinical usefulness of IMT or carotid plaque detection, however, has been widely questioned. Given the close correlation between traditional risk factors and subclinical carotid disease, the incremental value of IMT in improving cardiovascular risk prediction, beyond risk equation estimates, is probably limited.8,9 Although some studies suggest that measuring IMT improves risk estimates,2,10 others consider improvements in predictions to be irrelevant.8,9 However, systematic reviews indicate that plaque detection is better than IMT5,11 for improving vascular risk estimates. European guidelines on cardiovascular disease prevention currently recommend determining the presence of plaque but not IMT12 in subjects at intermediate risk. American guidelines only mention IMT, but do not explicitly recommend its measurement.13
Numerous studies have suggested that IMT and plaque are two different entities with different pathophysiology.14 In fact, there is no agreement between the different studies as to which risk factors are best associated with which entity. One of the factors that has traditionally caused much confusion with regard to this association is the site of IMT measurement. Measurement at the carotid bulb or internal carotid artery is better associated with the presence of plaque and coronary heart disease risk than measurement at the common carotid artery.14
The objective of this study was to evaluate the degree of correlation between different traditional risk factors and either IMT measured at the common carotid artery or the presence of plaque in a random sample of the population, and to establish whether both measures of subclinical vascular disease could be differentially determined by the different risk factors.
Patients and methodsESPREDIA (Screening PRE-diabetes and type 2 DIAbetes) is a population-based prospective study conducted in the northwest part of Madrid. 2553 subjects of both genders, aged between 45 and 74, who were randomly selected from primary care health records databases, were invited to participate.15 Pregnant women, patients with terminal illnesses, patients receiving long-term steroid or antipsychotic drug therapy and institutionalised patients were excluded. A total of 1592 (62.4%) agreed to participate, and 1475 of them had a carotid ultrasound available and were included in this study.
Patients were scheduled to attend the Outpatient Clinic at Hospital Carlos III de Madrid after fasting overnight. On arrival, a medical history and body measurements were taken and a physical examination, fasting blood tests and a carotid ultrasound were performed.
Patients were considered smokers if they had regularly smoked over the last 6 months, regardless of the number of cigarettes smoked. Blood pressure was measured 3 times with a 5-min interval between each measurement, using the mean of the last 2 measurements as the result.
A Doppler ultrasound study of both carotid arteries was performed using a 7.5mHz transducer (SonoSite MicroMaxx Ultrasound, SonoSite Inc., Bothell, Washington, USA). Patients had to lie down in the supine position with their neck hyperextended and rotated away from the side being examined. Bilateral scans of the entire length of the common carotid artery, carotid bulb and internal and external carotid arteries were performed to study the presence of plaque. Carotid plaque was defined as a focal thickening >1.5mm or thickening >50% of the surrounding IMT.16 Images were obtained from the distal wall of the common carotid artery to 1cm prior to the bifurcation from 3 different steering angles. The intima-media thickness (IMT) was obtained using automated software (SonoSite, SonoCalc IMT Software, SonoSite Inc., Bothell, Washington, USA) as the maximum and mean IMT values for each of the 6 segments measured (3 different angles on the right and left sides).
Statistical analysisQuantitative variables were expressed as mean and standard deviation. Qualitative variables were expressed as percentages. Quantitative variables were compared using ANOVA and qualitative variables were compared using a chi-square test. Forward stepwise logistic regression analyses were performed to evaluate factors associated with the presence of carotid plaque. Forward stepwise linear regression analyses were performed to evaluate factors associated with IMT. Variables with p<0.10 in the bivariate analysis and clinically relevant variables were included in the model for both analyses to avoid overfitting. The magnitude of associations were expressed as OR and 95% CI for the logistic regression, and as standardised coefficients for the linear regression. Data were analysed using SPSS for Windows, version 9.0 (IBM Corp, Armonk, New York, USA).
Ethical considerationsThe study was approved by the Independent Ethics Committee of Hospital Carlos III de Madrid in compliance with the Declaration of Helsinki and international guidelines for epidemiological studies (Geneva, 1991). All participants signed an informed consent form.
ResultsThe mean IMT of the 1475 participants in the study was 0.725±0.132mm and the maximum IMT was 0.868±0.167mm. In men, values were 0.752±0.146 and 0.907±0.183mm, and in women they were 0.703±0.116 and 0.837±0.146mm, respectively.
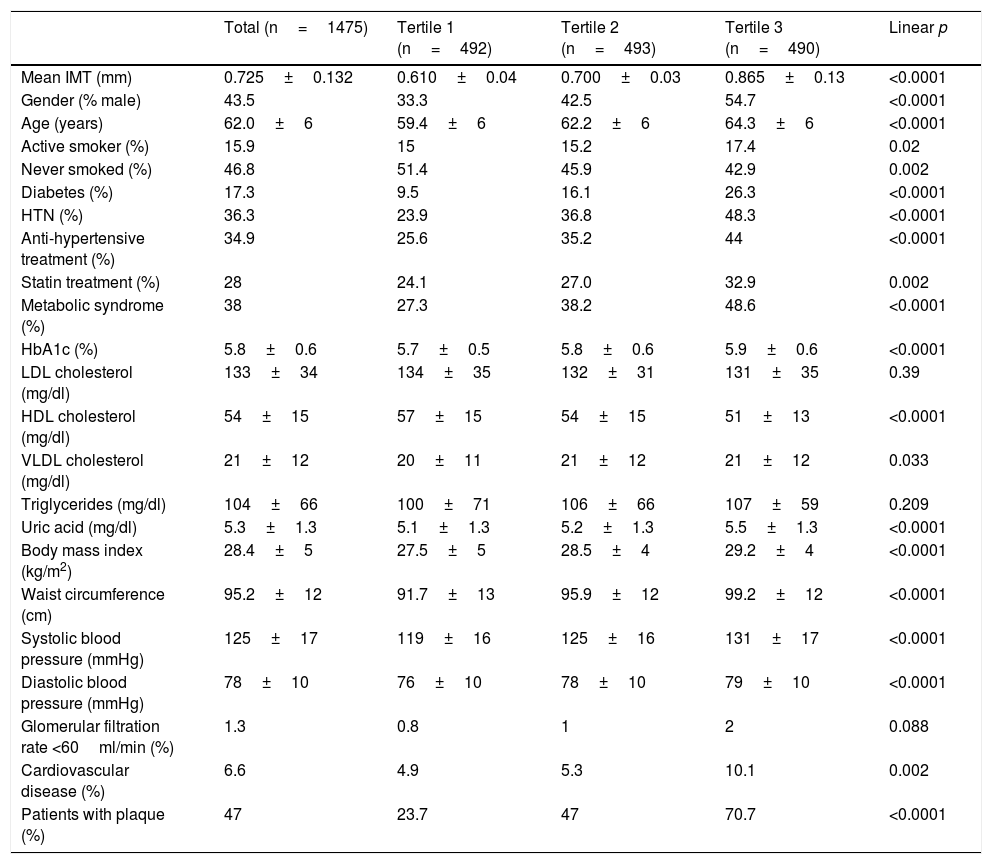
Population characteristics and risk factors (overall and according to tertiles of mean IMT) are shown in Table 1. Increasing age, male gender and the presence of various risk factors were associated with a greater IMT. Patients with a greater IMT were more likely to be treated with statins, which resulted in lower LDL cholesterol levels. On excluding patients treated with statins, the LDL cholesterol level according to tertiles of mean IMT was (from lowest to highest) 139±33, 140±28 and 141±31mg/dl; p=0.912.
Population characteristics according to tertiles of mean IMT.
| Total (n=1475) | Tertile 1 (n=492) | Tertile 2 (n=493) | Tertile 3 (n=490) | Linear p | |
|---|---|---|---|---|---|
| Mean IMT (mm) | 0.725±0.132 | 0.610±0.04 | 0.700±0.03 | 0.865±0.13 | <0.0001 |
| Gender (% male) | 43.5 | 33.3 | 42.5 | 54.7 | <0.0001 |
| Age (years) | 62.0±6 | 59.4±6 | 62.2±6 | 64.3±6 | <0.0001 |
| Active smoker (%) | 15.9 | 15 | 15.2 | 17.4 | 0.02 |
| Never smoked (%) | 46.8 | 51.4 | 45.9 | 42.9 | 0.002 |
| Diabetes (%) | 17.3 | 9.5 | 16.1 | 26.3 | <0.0001 |
| HTN (%) | 36.3 | 23.9 | 36.8 | 48.3 | <0.0001 |
| Anti-hypertensive treatment (%) | 34.9 | 25.6 | 35.2 | 44 | <0.0001 |
| Statin treatment (%) | 28 | 24.1 | 27.0 | 32.9 | 0.002 |
| Metabolic syndrome (%) | 38 | 27.3 | 38.2 | 48.6 | <0.0001 |
| HbA1c (%) | 5.8±0.6 | 5.7±0.5 | 5.8±0.6 | 5.9±0.6 | <0.0001 |
| LDL cholesterol (mg/dl) | 133±34 | 134±35 | 132±31 | 131±35 | 0.39 |
| HDL cholesterol (mg/dl) | 54±15 | 57±15 | 54±15 | 51±13 | <0.0001 |
| VLDL cholesterol (mg/dl) | 21±12 | 20±11 | 21±12 | 21±12 | 0.033 |
| Triglycerides (mg/dl) | 104±66 | 100±71 | 106±66 | 107±59 | 0.209 |
| Uric acid (mg/dl) | 5.3±1.3 | 5.1±1.3 | 5.2±1.3 | 5.5±1.3 | <0.0001 |
| Body mass index (kg/m2) | 28.4±5 | 27.5±5 | 28.5±4 | 29.2±4 | <0.0001 |
| Waist circumference (cm) | 95.2±12 | 91.7±13 | 95.9±12 | 99.2±12 | <0.0001 |
| Systolic blood pressure (mmHg) | 125±17 | 119±16 | 125±16 | 131±17 | <0.0001 |
| Diastolic blood pressure (mmHg) | 78±10 | 76±10 | 78±10 | 79±10 | <0.0001 |
| Glomerular filtration rate <60ml/min (%) | 1.3 | 0.8 | 1 | 2 | 0.088 |
| Cardiovascular disease (%) | 6.6 | 4.9 | 5.3 | 10.1 | 0.002 |
| Patients with plaque (%) | 47 | 23.7 | 47 | 70.7 | <0.0001 |
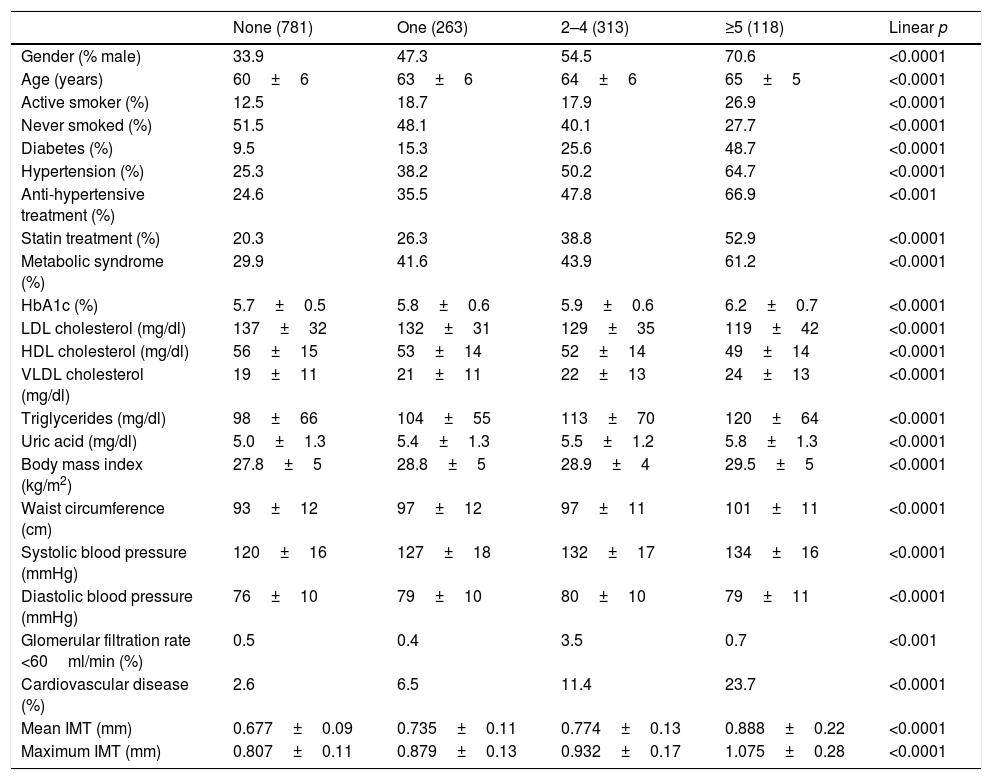
Forty-seven per cent (47%) of participants had carotid plaque: 17.8% had a single plaque, 21.2% had 2–4 plaques and 8% had 5 or more. Table 2 shows population characteristics according to the number of plaques.
Population characteristics according to number of carotid plaques.
| None (781) | One (263) | 2–4 (313) | ≥5 (118) | Linear p | |
|---|---|---|---|---|---|
| Gender (% male) | 33.9 | 47.3 | 54.5 | 70.6 | <0.0001 |
| Age (years) | 60±6 | 63±6 | 64±6 | 65±5 | <0.0001 |
| Active smoker (%) | 12.5 | 18.7 | 17.9 | 26.9 | <0.0001 |
| Never smoked (%) | 51.5 | 48.1 | 40.1 | 27.7 | <0.0001 |
| Diabetes (%) | 9.5 | 15.3 | 25.6 | 48.7 | <0.0001 |
| Hypertension (%) | 25.3 | 38.2 | 50.2 | 64.7 | <0.0001 |
| Anti-hypertensive treatment (%) | 24.6 | 35.5 | 47.8 | 66.9 | <0.001 |
| Statin treatment (%) | 20.3 | 26.3 | 38.8 | 52.9 | <0.0001 |
| Metabolic syndrome (%) | 29.9 | 41.6 | 43.9 | 61.2 | <0.0001 |
| HbA1c (%) | 5.7±0.5 | 5.8±0.6 | 5.9±0.6 | 6.2±0.7 | <0.0001 |
| LDL cholesterol (mg/dl) | 137±32 | 132±31 | 129±35 | 119±42 | <0.0001 |
| HDL cholesterol (mg/dl) | 56±15 | 53±14 | 52±14 | 49±14 | <0.0001 |
| VLDL cholesterol (mg/dl) | 19±11 | 21±11 | 22±13 | 24±13 | <0.0001 |
| Triglycerides (mg/dl) | 98±66 | 104±55 | 113±70 | 120±64 | <0.0001 |
| Uric acid (mg/dl) | 5.0±1.3 | 5.4±1.3 | 5.5±1.2 | 5.8±1.3 | <0.0001 |
| Body mass index (kg/m2) | 27.8±5 | 28.8±5 | 28.9±4 | 29.5±5 | <0.0001 |
| Waist circumference (cm) | 93±12 | 97±12 | 97±11 | 101±11 | <0.0001 |
| Systolic blood pressure (mmHg) | 120±16 | 127±18 | 132±17 | 134±16 | <0.0001 |
| Diastolic blood pressure (mmHg) | 76±10 | 79±10 | 80±10 | 79±11 | <0.0001 |
| Glomerular filtration rate <60ml/min (%) | 0.5 | 0.4 | 3.5 | 0.7 | <0.001 |
| Cardiovascular disease (%) | 2.6 | 6.5 | 11.4 | 23.7 | <0.0001 |
| Mean IMT (mm) | 0.677±0.09 | 0.735±0.11 | 0.774±0.13 | 0.888±0.22 | <0.0001 |
| Maximum IMT (mm) | 0.807±0.11 | 0.879±0.13 | 0.932±0.17 | 1.075±0.28 | <0.0001 |
A multivariate analysis was performed to determine factors associated with a greater IMT and the presence of plaque.
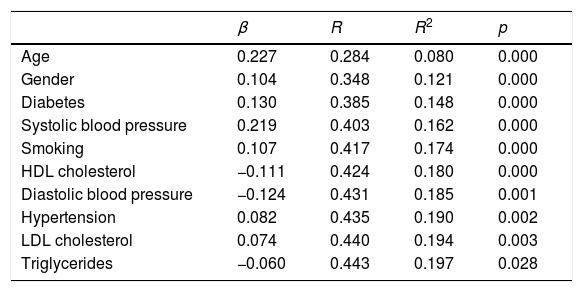
IMT was directly associated with age, male gender, the presence of hypertension, diabetes and active smoking, systolic blood pressure and LDL cholesterol level. It was inversely associated with diastolic blood pressure and HDL cholesterol and triglyceride levels (Table 3). These variables explained 19.7% of the variability found in mean IMT. Analyses were repeated after excluding patients treated with statins and after excluding patients with cardiovascular disease. Mean IMT-related risk factors were not modified in either analysis, except for triglyceride level, which was left out of the model in both circumstances.
Multiple linear regression analysis evaluating the factors associated with mean IMT.
| β | R | R2 | p | |
|---|---|---|---|---|
| Age | 0.227 | 0.284 | 0.080 | 0.000 |
| Gender | 0.104 | 0.348 | 0.121 | 0.000 |
| Diabetes | 0.130 | 0.385 | 0.148 | 0.000 |
| Systolic blood pressure | 0.219 | 0.403 | 0.162 | 0.000 |
| Smoking | 0.107 | 0.417 | 0.174 | 0.000 |
| HDL cholesterol | −0.111 | 0.424 | 0.180 | 0.000 |
| Diastolic blood pressure | −0.124 | 0.431 | 0.185 | 0.001 |
| Hypertension | 0.082 | 0.435 | 0.190 | 0.002 |
| LDL cholesterol | 0.074 | 0.440 | 0.194 | 0.003 |
| Triglycerides | −0.060 | 0.443 | 0.197 | 0.028 |
Body mass index, uric acid, statin treatment, waist circumference, glomerular filtration rate and metabolic syndrome are not included in the model.
Factors associated with maximum IMT were the same as those associated with mean IMT, explaining the 19.9% in variability.
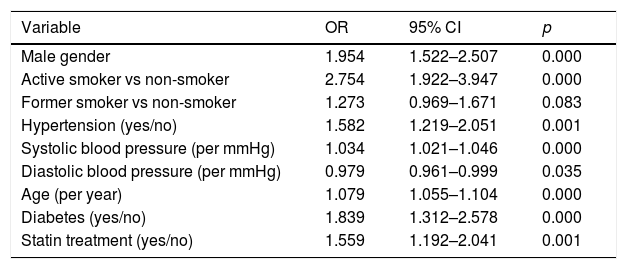
The presence of plaque was directly associated with age, male gender, smoking, a history of hypertension and diabetes, statin use and systolic blood pressure, and was inversely associated with diastolic blood pressure (Table 4). HDL cholesterol was excluded from the model with an OR of 0.992 (95% CI: 0.982–1.002; p=0.069). When the analyses were repeated after excluding patients treated with statins and those with cardiovascular disease, factors associated with the presence of plaque were the same, except for diastolic blood pressure, which was left out of both models.
Logistic regression analysis evaluating factors associated with the presence or absence of carotid plaque.
| Variable | OR | 95% CI | p |
|---|---|---|---|
| Male gender | 1.954 | 1.522–2.507 | 0.000 |
| Active smoker vs non-smoker | 2.754 | 1.922–3.947 | 0.000 |
| Former smoker vs non-smoker | 1.273 | 0.969–1.671 | 0.083 |
| Hypertension (yes/no) | 1.582 | 1.219–2.051 | 0.001 |
| Systolic blood pressure (per mmHg) | 1.034 | 1.021–1.046 | 0.000 |
| Diastolic blood pressure (per mmHg) | 0.979 | 0.961–0.999 | 0.035 |
| Age (per year) | 1.079 | 1.055–1.104 | 0.000 |
| Diabetes (yes/no) | 1.839 | 1.312–2.578 | 0.000 |
| Statin treatment (yes/no) | 1.559 | 1.192–2.041 | 0.001 |
LDL cholesterol, HDL cholesterol, VLDL cholesterol, body mass index, uric acid and glomerular filtration rate are not included in the model.
A total of 97 subjects (6.6%) had cardiovascular disease: 52 with coronary heart disease, 33 with cerebrovascular disease and 19 with peripheral artery disease. Patients with cardiovascular disease had a greater mean IMT (0.793±0.205 vs 0.720±0.124mm, p<0.0001) and maximum IMT (0.958±0.268 vs 0.861±0.155mm, p<0.0001) than those patients with no cardiovascular disease. Likewise, the percentage of patients with plaque was higher among participants with cardiovascular disease than among patients with no cardiovascular disease (79.6% vs 44.7%, p<0.0001).
Patients with plaque had a higher prevalence of cardiovascular disease after adjusting for age, gender, smoking, hypertension, systolic and diastolic blood pressure, statin use, lipid levels and diabetes (OR 2.40; 95% CI: 1.35–4.27, p=0.003). Likewise, the association between mean IMT and cardiovascular disease remained significant after adjusting for all the variables included in the multivariate model (beta coefficient 0.059, p=0.02).
DiscussionOur results show that both IMT measured at the common carotid artery and presence of carotid plaque share the same vascular risk factors and support the idea that intima-media thickening occurs just prior to atheromatous plaque development.17
There is major controversy concerning the relationship between IMT, plaque and cardiovascular risk prediction, which is probably greatly influenced by the site at which IMT is measured. IMT comprises the endothelial layer, connective tissue and the smooth muscle layer, and is the site of lipid deposition in plaque formation. It is thought that measurement of IMT at the common carotid artery is more an indicator of smooth muscle cell hypertrophy or hyperplasia, while measurement of IMT at the carotid bulb and internal carotid artery, and the presence of plaque, are indicators of previously established atherosclerosis. In fact, some authors have found that the risk factors most closely associated with IMT at the common carotid artery are age and blood pressure,18 which are also closely associated with a risk of stroke. However, IMT measured at the carotid bulb and internal carotid artery are associated with classic cardiovascular risk factors, plaque and coronary risk.3,14 Measurement of IMT at these sites is, however, technically more complex and results in greater variability, making it less common in epidemiological studies.
In our study, all risk factors were associated to similar degrees with IMT and the presence of plaque. Although lipid variables disappeared in the plaque prediction model, they were of borderline statistical significance, reaching almost significant OR. In fact, other studies that, like our own, have measured IMT at the common carotid artery, have also found associations between this variable and age, gender, smoking, diabetes, blood pressure and LDL cholesterol.19,20 In studies evaluating the impact of risk factors on IMT at the common carotid artery, such risk factors only account for 17% of the variability in IMT,21 which is similar to the figure found in our study.
Statin use was directly associated with IMT in the univariate model due to the fact that statins were used more often in patients with diabetes and established cardiovascular disease, populations with a higher prevalence of intima-media thickening. The inverse relationship between IMT and number of plaques and diastolic blood pressure has been found in previous studies and has been attributed to the association between vascular disease and arterial stiffness, which is accompanied by increases in systolic blood pressure and decreases in diastolic blood pressure.22
The fact that IMT measured at the common carotid artery has not been shown to improve prediction of the risk of cardiovascular events above traditional risk factors23 does not mean that it is not an indicator of early atherosclerosis. The appearance of plaque from intima-media thickening may require more severe risk factors, longer progression time or other additional factors. Once plaque appears, its association with the risk of cardiovascular events becomes more evident and allows improved prediction of the risk indicated by classic risk factors. In fact, not only the presence of plaque, but also the number of plaques observed, has been associated with the risk of coronary complications.24 In this sense, our study has also shown that greater prevalence and more severe risk factors are associated with a greater number of plaques.
One limitation of our study is its cross-sectional design, which makes it impossible to establish causal relationships. Nevertheless, it has been conducted under carefully controlled conditions by a single ultrasound technician using automated software, which, unlike some earlier studies, has allowed very precise measurements.
We can conclude that risk factors associated with IMT measured at the common carotid artery and the presence of plaque are similar, which supports the continuum between muscle cell hypertrophy and the development of atherosclerosis.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed complied with the ethical standards of the responsible human experimentation committee and with the World Medical Association and the Declaration of Helsinki.
Confidentiality of dataThe authors declare that they have followed the protocols implemented in their place of work regarding the publication of patient data.
Right to privacy and informed consentThe authors obtained informed consent from the patients and/or subjects referred to in this article. The corresponding author is in possession of this document.
FundingThe study has been partially funded by a grant from Novo Nordisk and from the Fundación para el Fomento y Desarrollo de la Investigación Clínica [Foundation for the Promotion and Development of Clinical Research] (FYDIC).
Conflicts of interestThe authors have no conflicts of interest.
The following authors have helped with data collection and analysis:
Carmen de Burgos-Lunar, Paloma Gómez-Campelo, Belén Fernández Puntero, Luís Montesano Sánchez, David Vicent López, Pedro J. Fernández García, Jesús Castro Toro, Vanessa Sánchez Arroyo and Pedro Patrón Barandío.
We would like to thank all the doctors from the ESPREDIA group for their collaboration:
Concepción Aguilera Linde (CS Ciudad Periodistas), Álvaro R. Aguirre de Carcer Escolano (CS La Ventilla), Patricio Alonso Sacristán (CS Ciudad Periodistas), M. Jesús Álvarez Otero (CS Dr. Castroviejo), Paloma Arribas Pérez (CS Santa Hortensia), María Luisa Asensio Ruiz (CS Fuentelarreina), Pablo Astorga Díaz (CS Barrio Pilar), Begoña Berriatua Ena (CS Dr. Castroviejo), Ana Isabel Bezos Varela (CS José Marva), María José Calatrava Triguero (CS Ciudad Jardín), Carlos Casanova García (CS Barrio Pilar), Ángeles Conde Llorente (CS Barrio Pilar), Concepción Díaz Laso (CS Fuentelarreina), Emilia Elviro García (CS Ciudad Periodistas), Orlando Enríquez Dueñas (CS Fuentelarreina), María Isabel Ferrer Zapata (CS El Greco), Froilán Antuña (CS Ciudad Periodistas), María Isabel García Lázaro (CS Ciudad Periodistas), María Teresa Gómez Rodríguez (CS Barrio Pilar), África Gómez Lucena (CS La Ventilla), Francisco Herrero Hernández (CS La Ventilla), Rosa Julián Viñals (CS Dr. Castroviejo), Gerardo López Ruiz Ogarrio (CS Barrio Pilar), María del Carmen Lumbreras Manzano (CS José Marva), Sonsoles Paloma Luquero López (CS Ciudad Periodistas), Ana Martínez Cabrera Peláez (CS Barrio Pilar), Montserrat Nieto Candenas (CS La Ventilla), María Alejandra Rabanal Carrera (CS Barrio Pilar), Ángel Castellanos Rodríguez (CS Ciudad Periodistas), Ana López Castellanos (CS La Ventilla), Milagros Velázquez García (CS Barrio Pilar) and Margarita Ruiz Pacheco (CS Dr. Castroviejo).
Members of the ESPREDIA Group are listed in Appendix.
Please cite this article as: Mostaza JM, Lahoz C, Salinero-Fort MA, Laguna F, Estirado E, García-Iglesias F, et al. Factores de riesgo asociados con el grosor íntima-media y la presencia de placas en arteria carótida: Estudio ESPREDIA. Clin Investig Arterioscler. 2018;30:49–55.