Pregnancy at an advanced maternal age has become a reality. The acceptance rate of an unwanted pregnancy in this age group is lower, resulting in a higher proportion of pregnancy interruptions. This study aims to characterize abortion by request (AR) in advanced maternal age.
MethodsDescriptive study of AR requested by women aged 40 years old or older, over a period of six years, in an Obstetrics service of a Portuguese tertiary hospital. Descriptive data analysis was performed using SPSS® version 26.
Results194 women were included in the study (n=194), with a median age of 42 years, most of them Portuguese (94.3%) and with no history of performing AR (75.2%). The contraceptive methods used prior to AR were used oral contraception (47.0%) and barrier contraception (39.1%). Medical abortion was performed in the entire sample, with a success rate of 96.9%. After AR, intrauterine contraception (44.3%), oral contraception (22.7%) and the vaginal ring (7.2%) were the preferred contraceptive methods.
Discussion/ConclusionsChanges in women's health and contraceptive needs motivate new approaches and contraceptive strategies. After AR, a significant percentage of woman chose long-term and non-user-dependent methods. Particularly in women aged 40 or over, these methods, in addition to their highly effective and safe contraceptive role, may bring additional non-contraceptive benefits, namely the therapeutic effect in abnormal uterine bleeding.
El embarazo a una edad materna avanzada se ha convertido en una realidad. La tasa de aceptación de un embarazo no deseado en esta edad es menor, lo que se traduce en una mayor proporción de interrupciones del embarazo. Este estudio tiene como objetivo caracterizar la interrupción voluntaria del embarazo (IVE) en edad materna avanzada.
MétodosEstudio descriptivo de las IVE solicitadas por mujeres de 40 años o más, durante un período de 6 años, en un servicio de obstetricia de un hospital terciario portugués. El análisis descriptivo de los datos se realizó con SPSS® versión 26.
ResultadosSe incluyeron en el estudio 194 mujeres (n=194), con una mediana de edad de 42 años, la mayoría portuguesas (94,3%) y sin antecedentes de realización de IVE (75,2%). Los métodos anticonceptivos utilizados antes de la IVE fueron la anticoncepción oral (47,0%) y la anticoncepción de barrera (39,1%). El aborto médico se realizó en toda la muestra, con una tasa de éxito del 96,9%. Después de la IVE, la anticoncepción intrauterina (44,3%), la anticoncepción oral (22,7%) y el anillo vaginal (7,2%) fueron los métodos anticonceptivos preferidos.
Discusión/conclusionesLos cambios en la salud de las mujeres y las necesidades anticonceptivas motivan nuevos enfoques y estrategias anticonceptivas. Después de la IVE, un porcentaje significativo de mujeres eligió métodos a largo plazo y no dependientes de la usuaria. Particularmente en mujeres de 40 años o más, estos métodos, además de su función anticonceptiva altamente efectiva y segura, pueden traer beneficios adicionales no anticonceptivos, por ejemplo, el efecto terapéutico en el sangrado uterino anormal.
Safe abortion by request (AR) is a fundamental part of women's health care. It is a public health indicator that reflects not only the fertility of the population, but also the accessibility to contraception care.1 According to the World Health Organization (WHO), nearly half of pregnancies – 121 million – are unplanned annually. Of these, 6 out of 10 are interrupted by woman's choice.2
In Portugal, AR was decriminalized in 2007 and is allowed up to the first 10 completed weeks of pregnancy.3 The realization of AR, by medication or surgical procedure, takes place in three periods.3–5
- 1.
First appointment – It comprises a detailed medical, gynecological and obstetrical history, including contraceptive methods used and reasons of failure, and counseling is provided regarding abortion procedure and future contraception methods.3
- 2.
Day of the procedure – It takes place after a mandatory period of reflection (minimum of 3 days), during which the woman can request psychological support/counseling or social support.3
- 3.
Control appointment – It takes place 2–3 weeks after the procedure and ultrasound examination is provided to confirm treatment efficacy. This moment is also an opportunity for clarification and advice on contraceptive methods.3
According to the Portuguese AR registration report, in 2021, the total of AR in the first 10 weeks was 11,640, corresponding to 95.8% of the total of abortions performed in Portugal, maintaining the downward trend since 2012.4 Official statistics from most countries that have provided data indicate that about half of all abortions are carried out using medication, a reality that also occurs in Portugal.4,5
Complications resulting from unsafe abortion are one of the main causes of maternal morbidity and mortality worldwide. However, when an experienced medical professional performs this procedure, mortality from an AR is much lower comparing to maternal mortality from a full-term pregnancy.6
Pregnancy at an advanced maternal age has become a reality, particularly in developed countries.7 Although fertility declines after 40 years old, the acceptance of an unwanted pregnancy in this age group is also lower, with a higher proportion of pregnancy interruptions.8,9
This study aims to analyze pregnancies interrupted by choice by women with advanced maternal age, including sociodemographic characteristics and contraceptive practices.
Material and methodsIt was performed a descriptive observational study, through the analysis of a questionnaire carried out to women of advanced maternal age who performed AR, between January 1st of 2015 and December 31st of 2020 (six years), in an Obstetrics center from a Portuguese tertiary hospital.
The study sample identification was made through a pre-existing database, in which the data related to AR is registered anonymously and prospectively.
Inclusion criteria were: women aged≥40 years who had AR and completed an anonymous questionnaire at that time.
The following variables were analyzed: age, nationality, educational qualifications, marital status, parity, previous AR, access to health care, contraception prior to abortion, waiting time for the first appointment, reflection time, gestational age ate the first appointment, reasons for asking the abortion, type of abortion, contraception after abortion.
A descriptive analysis of the data was made using two tools: IBM SPSS Statistics® version 26 for Windows.
ResultsA total of 1914 pregnancy interruptions were carried out by woman's choice during the selected period, and 194 of them met the inclusion criteria, constituting the study sample (n=194).
The median age was 42 years old [40–48] and the sociodemographic characterization is represented in Table 1.
Sociodemographic characterization.
| Study sample (n=194) | |
|---|---|
| n (%) | |
| Nationality | |
| Portuguese | 183 (94.3%) |
| Other | 11 (5.7%) |
| Educational qualifications | |
| Basic education | 49 (25.3%) |
| Secondary education | 64 (33.0%) |
| University education | 78 (40.2%) |
| Unknown | 3 (1.5%) |
| Marital status | |
| Married | 118 (60.8%) |
| Single | 45 (23.2%) |
| Divorced | 30 (15.5%) |
| Widow | 1 (0.5%) |
| Parity/number of children | |
| Nulliparous | 12 (6.2%) |
| 1 Child | 49 (25.3%) |
| 2 Children | 102 (52.6%) |
| ≥3 Children | 27 (13.9%) |
| Unknown | 4 (2.0%) |
| Number of prior abortions | |
| 0 | 146 (75.2%) |
| 1 | 36 (18.6%) |
| ≥2 | 11 (5.7%) |
| Unknown | 1 (0.5%) |
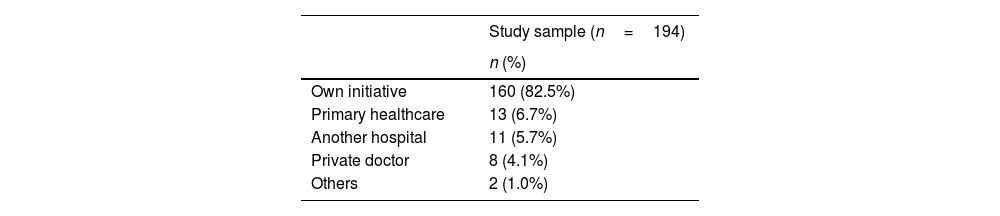
Regarding access to health care, most women resorted to the first appointment on their own initiative, as shown in Table 2. When asked about having family planning (FP) appointment in the previous year, 67,0% (n=130) reported have not attended this appointment. Of the women who had FP (n=58), primary health care and the private hospital were the institutions where this evaluation was mostly carried out, respectively in 37.9% (n=22) and 51.7% (n=30).
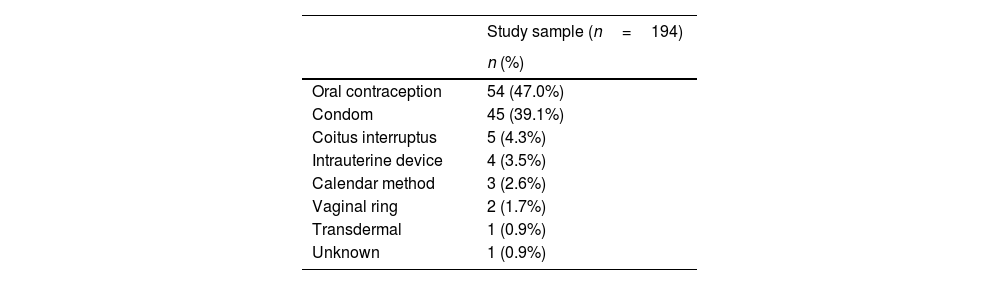
Contraception before abortionRegarding the use of contraceptive methods prior to the abortion, 59.3% (n=115) mentioned their use. The used methods are represented in Table 3. As for possible causes of unwanted pregnancy, forgetting to use of the method (20.9%, n=24), the correct use with failure of the method (18.3%, n=21) and irregular use (10.4%, n=12) were the most mentioned factors.
Only 2.1% (n=4) reported having used emergency contraception after unprotected sexual intercourse.
Appointment for procedureThe median of waiting time for the first appointment was 2 days [0–13] and the median of the reflection period was 4 days [0–14].
The median cranial–caudal length at the first visit was 6.5mm [1.0–32.0], corresponding to a median gestational age of 7 weeks [5–10].
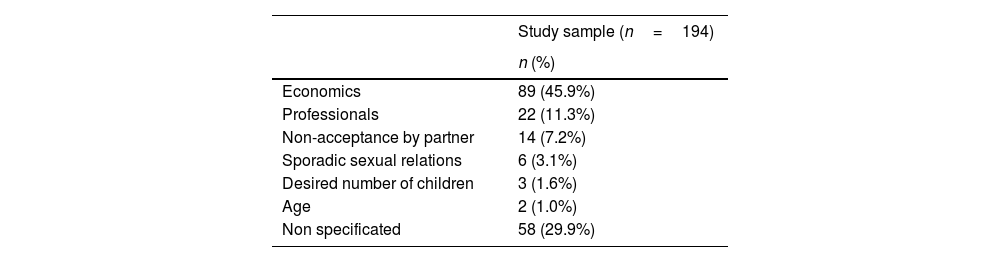
The reasons mentioned for performing the AR are shown in Table 4.
AR by medication was performed in all cases (100%, n=194). At the time of the third appointment, 3.1% (n=6) had retained ovular material. Of these, 50.0% (n=3) solved with a new application of vaginal misoprostol and 50.0% (n=3) required surgical uterine evacuation.
The median time of expulsion of products of conception was 4h [0–20] and the median pain scale (between 0 and 10) experienced was 5 [0–10].
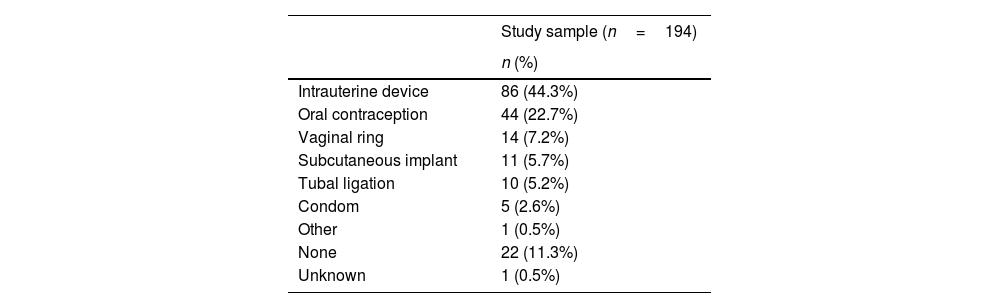
Contraception after abortionAfter performing the AR, contraceptive advice was reinforced in the third appointment. 27.5% of women chose maintain their previous contraceptive method. Table 5 shows the contraceptive choice after performing AR.
In the sample, the rate of non-attendance to the third appointment was 8.2% (n=16).
DiscussionIn this study, the AR performed in women aged 40 years and over represented 10.1% of the total of AR performed in the studied period. Although fertility decreases after this phase of a woman's life, the frequency of unwanted pregnancies is still significant and may represent a possible target for intervention.8,9
Most women in the sample reported having at least one child, which may be related to the fact that, in this age group, most women have already completed their reproductive project and an unwanted pregnancy represents unanticipated difficulties. On the other hand, when analyzing the reasons for the AR, most of them cited economic reasons as the main difficulty, with age and the desired number of children being reasons mentioned by a small percentage. These data may point to the fact that pregnancy after the age of 40 is socially well-accepted that other circumstantial conditions are more preponderant in the decision than the age itself.
When analyzing the frequency of FP appointments in the year before the abortion, it appears that most women did not have access to or did not request it. In addition, in the cases of women who had the FP appointment, only 38% of cases were performed in primary health care. This point can be an object of improvement in the provision of health care and its accessibility.
Contraception before abortionIn the study sample, 59.3% were using contraceptive method when they became pregnant, and the most mentioned reasons for the cause of the unwanted pregnancy were forgetting to take/use it, failure and irregular use of the method. When evaluating the contraceptive methods before the AR, it appears that most are user-dependent, in particular oral contraception, the most used method globally.10
Emergency contraception was used in only 2.1% of cases. This low use may reflect a lack of knowledge about its existence, efficiency, the correct period for its use and safety. Although the regular use of a contraceptive method is the best strategy for preventing unwanted pregnancies, in case of unprotected sexual intercourse, the option of emergency contraception significantly reduces the possibility of an unwanted pregnancy.11 For these reasons, it can be useful, in the FP appointments, to reinforce information to the population about this alternative.
Contraception after abortionHealth care provided during AR should include contraceptive counseling and the availability of the woman's chosen method.12,13 Considering that woman's fertility returns quickly after the interruption, the timing of contraceptive counseling and prescription or application of the method elected are also decisive factors.14
In cases of unwanted pregnancy in women already using a contraceptive method, it is important to discuss the reasons for failure and the possibilities for improving and/or changing the method.13
As previously mentioned, in the third appointment of the AR process, contraceptive advice is reinforced and, if the woman wishes, the chosen method can be started immediately.3
In this population, there was a high rate of attendance at the control appointment, and this resulted in changes in contraceptive preferences after the procedure. It should be highlighted the high frequency of choice of long-term and non-user dependent methods, particularly intrauterine contraception, vaginal ring and subcutaneous etonogestrel implant, and a lower preference of methods that are highly dependent on their use (condoms and oral contraception). These preferences are similar with the preferences of the general Portuguese population, in which long-acting reversible contraception (LARCs) has been increasing significantly.15 Furthermore, it is similar to literature in the context of choosing contraception after abortion (there is a high adherence to initiation or changing the contraceptive method to a user-independent method).16–18
The role of LARCs in reducing unwanted pregnancies and the consequent pregnancy interruptions have been discussed in several publications, which is why LARCs have been proposed as the first-line contraceptive after an AR.19 In fact, Keene et al. reported an increased preference for LARCs in the immediate post-abortion period. In this follow-up, they revealed the need to remove barriers to access to these methods. The convenience of their application is also an advantage in clinical practice, as these methods can be early initiated when taking mifepristone in the case of implants or after expulsion the in case of intrauterine devices.20
After 40 years old, women can benefit from non-contraceptive benefits of these long-acting contraceptive methods, such as treatment of abnormal uterine bleeding, dysmenorrhea, and vasomotor symptoms.21 These methods can also play an important role in protecting bone mineralization and reducing the risk of ovarian and colorectal cancers.22 Particularly when the option is the intrauterine device, the convenience of its use, its acceptance, the possible application at the control visit, and its non-contraceptive benefits highlight the importance of this contraceptive option, particularly in this population.
ConclusionsThe occurrence of unwanted pregnancies after 40 years old and the need to interrupt the pregnancy by woman's choice are frequently found in clinical practice. Particularly in this age group, an unwanted pregnancy can be unexpected and difficult to manage; enhancing the importance of adopting a patient centered approach. This includes identification of the contraceptive needs and other concomitant clinical situations that can be managed together, increasing adherence to therapy and greater user satisfaction. In this process, it is also important to find a balance between the professional's expectations about the method considered more appropriate and the setting of realistic and woman-centered goals.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Patient consentThe authors declare that the procedures were followed according to the regulations established by the Clinical Research and Ethics Committee and to the 2013 Helsinki Declaration of the World Medical Association. The authors declare having followed the protocols in use at their working center regarding patients’ data publication. Informed consent was obtained from all subjects involved in the study.
FundingThis research received no external funding.
Conflict of interestThe authors declare no conflict of interest.