A number of complications exist with invasive mechanical ventilation and with the use of and withdrawal from prolonged ventilator support. The use of protocols that enable the systematic identification of patients eligible for an interruption in mechanical ventilation can significantly reduce the number of complications. This study describes the application of a weaning protocol and its results.
METHODS:Patients who required invasive mechanical ventilation for more than 24 hours were included and assessed daily to identify individuals who were ready to begin the weaning process.
RESULTS:We studied 252 patients with a median mechanical ventilation time of 3.7 days (interquartile range of 1 to 23 days), a rapid shallow breathing index value of 48 (median), a maximum inspiratory pressure of 40 cmH2O, and a maximum expiratory pressure of 40 cm H2O (median). Of these 252 patients, 32 (12.7%) had to be reintubated, which represented weaning failure. Noninvasive ventilation was used postextubation in 170 (73%) patients, and 15% of these patients were reintubated, which also represented weaning failure. The mortality rate of the 252 patients studied was 8.73% (22), and there was no significant difference in the age, gender, mechanical ventilation time, and maximum inspiratory pressure between the survivors and nonsurvivors.
CONCLUSIONS:The use of a specific weaning protocol resulted in a lower mechanical ventilation time and an acceptable reintubation rate. This protocol can be used as a comparative index in hospitals to improve the weaning system, its monitoring and the informative reporting of patient outcomes and may represent a future tool and source of quality markers for patient care.
Mechanical ventilation (MV) can cause complications in several systems that can subsequently extend the amount of time that MV is required. Consequently, MV can lengthen a patient's stay in the intensive care unit (ICU) and increase the risk of mortality. Both prolonged ventilation support and early withdrawal are associated with a number of complications (1,2).
Between 25% and 40% of extubated patients can develop respiratory failure (3,4), even when extubation is performed appropriately. Moreover, there are no established objective parameters for identifying patients who are at risk of failure during the MV weaning procedure, and 5 to 20% of extubated patients require reintubation due to associated complications (5,6).
It has been shown that systematic identification protocols can significantly decrease the duration of MV by identifying patients with suitable conditions for the interruption of MV, which serves to reduce the likelihood of ventilator-associated pneumonia, the MV times, the ICU and hospital stays and also the complications associated with prolonged ventilation and early withdrawal (7,8). Moreover, these recommendations must be followed to identify patients who may be eligible for spontaneous breathing testing and extubation. In practice, the implementation and monitoring of these recommendations are neither generally systematized nor well known in intensive care unit communities.
Our mechanical ventilation weaning protocol was developed according to recommendations from previous studies (7-9). The present study aims to describe the application of this protocol and the results of its use regarding MV time and the number of patients who required reintubation.
MATERIALS AND METHODSThis study was conducted at a 38-bed medical-surgical ICU of a private tertiary care hospital in São Paulo, Brazil. This is an open staffing-model ICU that annually admits approximately 2,200 patients, 28% of whom on average are submitted to invasive MV. Because our protocol had previously been standardized and is routinely applied in our ICU, the review board waived the requirement for ethical approval and informed consent.
In this retrospective study, data from the period between January 2009 and April 2010 (a total of 15 months) were analyzed. These data were obtained from a specific mechanical ventilation weaning chart.
For our study, we enrolled patients who required invasive MV for more than 24 hours. Patients who were tracheostomized, apneustic, had intense psychomotor agitation, and those who were accidentally extubated were excluded.
The patients were assessed daily to identify those who were able to commence the MV withdrawal process. This assessment was performed at least once per day, and clinical criteria and conditions were used to identify the patient's readiness for spontaneous ventilation. The patients were also submitted to daily interruption of sedation.
Each patient was assessed daily to determine whether he/she had begun to recover from the condition(s) that necessitated ventilatory support. For these assessments, the following parameters were evaluated: the adequacy of gas exchange (partial arterial pressure of oxygen [PaO2] higher than 60 mmHg, FiO2 lower or equal to 40%, and PEEP between 5 and 10 cm H2O); hemodynamic stability (in terms of adequate tissue perfusion, independence from or low-dose administration of vasopressors, the absence of acute coronary insufficiency or arrhythmias with hemodynamic repercussions), and the capacity to begin inspiratory efforts; hemoglobin levels above 8 g/DL; corrected metabolic and corrected electrolytic disorders; control of infection; and a body temperature lower than 38°C.
After identifying patients who were eligible to begin ventilatory weaning, maximum inspiratory pressure (MIP) was monitored (starting at the residual functional capacity) using a manovacuometer that was connected to a unidirectional valve. Maximum expiratory pressure (MEP) was measured (starting at the patient's total pulmonary capacity) using a manovacuometer that was connected to a unidirectional valve. Spontaneous tidal volume was measured using a ventilometer that was connected directly to the airway. Minute ventilation (liters), respiratory frequency and the rapid shallow breathing index (RSBI) were also used as indicators of readiness for MV weaning. The RSBI is a predictive index of weaning used to reduce the occurrence of extubation failure, and this index seems to be the most accurate predictive index available (10,11). The RSBI values are calculated dividing the respiratory rate by the tidal volume (L), values bellow 104 bpm/L indicated a likelihood of success. RSBI is a good predictive index of weaning success, but not weaning failure (11).
After the above mentioned procedures were performed, the patients were submitted to the spontaneous breathing test (SBT), which was performed in the ventilatory mode with pressure support ventilation (PSV) between 5 and 7 cmH2O, PEEP levels between 5 and 10 cmH2O and FiO2 values between 30 and 40% for 30 to 120 minutes. The patients who did not present any signs of intolerance to the SBT were extubated.
The cuff-leak test previously described by Bast et al. (12) was used to assess possible airway obstructions. The patients were briefly ventilated using the volume-predetermined (assist-controlled) mode, and the volume expired through the endotracheal tube was monitored with the cuff inflated and deflated. The gas leak around the tube was monitored, and the difference between the expired volume with the cuff inflated and deflated was observed. Patients with a positive test result (i.e., a gas leak around the endotracheal tube less than 15.5%) caused by airway obstructions were kept on MV, and a bronchoscopy exam was considered to ensure a safe extubation.
Patients with signs of intolerance to the SBT resumed the comfort ventilatory mode, and there was a 24-hour waiting period before revaluation. The following were considered signs of SBT intolerance: (I) hemodynamic instability, such as heart rate (HR) higher than 120 bpm or HR more than 20% above the initial value, systolic pressure higher than 180 mmHg, and mean arterial pressure more than 20% above the initial value or hypotension; (II) respiratory discomfort, as indicated by a respiratory rate (RR) higher than 30 bpm or more than 50% above the initial rate; (III) pulse oximetry lower than 90%; (IV) PaO2 lower than 60 mmHg; (V) pH lower than 7.32; (VI) a greater than 10 mmHg increase in the partial arterial pressure of carbon dioxide (PaCO2) relative to the initial values; or (VII) agitation, sudoresis, or alteration of the level of consciousness.
Patients diagnosed with chronic obstructive pulmonary disease (COPD), congestive heart failure (CHF), acute respiratory distress syndrome or other clinical indications were extubated, and NIV was promptly instituted (13,14). NIV was administered for a minimum of 24 hours, and the patients also received three physical therapy sessions consisting of techniques for maintaining adequate bronchial hygiene, lung expansibility, and functional activities. The patients who were extubated received oxygen therapy if necessary and underwent the same three daily physiotherapy sessions, although these sessions also included intermittent positive pressure exercises. Patients who were reintubated up to 48 hours after extubation were considered to represent weaning failure.
To implement and enforce this MV weaning protocol and ensure that its standards were met, the team of professionals involved (physical therapists and physicians) underwent training that consisted of teaching and case discussions. The MV records were examined daily to ensure protocol compliance, and all data collected from these records were reported every three months to the multidisciplinary teams.
Statistical analysisCategorical variables were expressed as absolute and relative frequencies (percentages). Quantitative variables were expressed as the means and 95% confidence intervals (95% CI) if normally distributed or as median and interquartile ranges (IQR) if conversely distributed. To evaluate differences in parametric variables between patients who survived and those who did not, the Student's t-test was used; for nonparametric variables, the Mann-Whitney test was used. R software Version 10.1 was used for the statistical analysis.
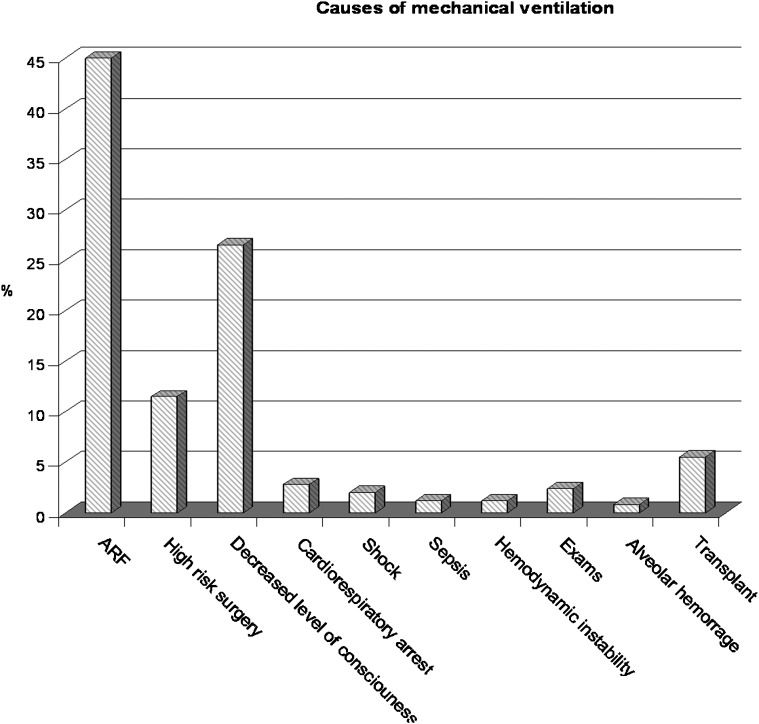
RESULTSThis study was conducted over a 15-month period. Two hundred fifty-two patients who were on MV and complied with the weaning protocol when they became eligible for the SBT and extubation were included. The median age of these patients was 64 years (IQR: 16 to 96 years), most patients were male (64.4%), and there was a median APACHE II score of 22 (95% CI: 21-23) (Table 1). Acute respiratory failure was the primary reason for orotracheal intubation (45%; Figure 1). The patients had a median MV time of 3.7 days (IQR: 1 to 23 days), a median RSBI of 48 bpm/L (IQR: 14 to 190), a median MIP of -40 cmH2O (IQR: -20 to -120 cmH2O), and a median MEP of 40 cmH2O (IQR: 12 to 120 cmH2O). Thirty-two patients (12.7%) required reintubation, which was considered to represent weaning failure (Table 1). There were no positive cuff-leak test results and no signs of airway obstruction prior to extubation.
Characteristics of the 252 mechanically ventilated patients treated at Albert Einstein Jewish Hospital during a 15-month period.
| Age (years) – median (IQR) | 64 (16-96) |
|---|---|
| Gender – n (%)FemaleMale | 83 (35.6)150 (64.4) |
| APACHE II score – median (IQR) | 22 (21-23) |
| MV time (days) – median (IQR) | 3.7 (1-23) |
| RSBI (bpm/L)– median (IQR) | 48 (14-190) |
| MIP (cmH2O) – median (IQR) | -40 (20-120) |
| MEP (cmH2O) – median (IQR) | 40 (12-120) |
| NIV after extubation – n (%) | 170 (73.2) |
| Reintubation rate – n (%) | 32 (12.7) |
IQR: interquartile ratio; MV: mechanical ventilation; RSBI: respiratory shallow breathing index; MIP: maximum inspiratory pressure; MEP: maximum expiratory pressure; NIV: noninvasive ventilation.
Of the 252 patients who were studied, 170 (73%) were administered NIV postextubation; of these, 26 (15%) required reintubation and were considered weaning failures.
The reasons for weaning failure were identified for the group of reintubated patients (12.7%). The most common reasons for reintubation included reduced consciousness (37.5%), acute respiratory failure (37.5%), and a lack of upper airway protection (15.3%) (Figure 2). However, there were no differences in age, RSBI, MIP, MEP, NIV use, MV time, and APACHE II score between the patients who required reintubation and those who did not (Table 2).
Comparison of the characteristics of patients who did and did not require reintubation.
| Reintubation(n = 32) | No Reintubation(n = 220) | p-value | |
|---|---|---|---|
| Age (years) – median (IQR) | 71 (60-84) | 64 (52-77) | 0.122 |
| RSBI (bpm/L) – median (IQR) | 52 (33-57) | 48 (35-64) | 0.800 |
| MIP (cmH2O) – median (IQR) | -40 (-38 to -48) | -40 (-38 to -60) | 0.650 |
| MEP (cmH2O) – median (IQR) | 40 (30-54) | 40 (35-47) | 0.720 |
| NIV use – n(%) | 26 (81) | 144 (65) | 0.070 |
| MV time (days) – median (IQR) | 4 (2-8) | 3 (2-6) | 0.180 |
| APACHE II score – median (IQR) | 23 (10-42) | 25 (23-37) | 0.484 |
IQR: interquartile range; RSBI: respiratory shallow breathing index; MIP: maximum inspiratory pressure; MEP: maximum expiratory pressure; NIV: noninvasive ventilation; MV: mechanical ventilation.
The mortality rate of the reintubated patients was 8.73% (22), and there were no significant differences in age, gender, MV time, and MIP between the survivors and nonsurvivors (Table 3).
Comparison of patient characteristics between survivors and nonsurvivors.
| Variables | Survivors | Nonsurvivors | p-value |
|---|---|---|---|
| Age (years) - median (IQR) | 65 (36-100) | 66 (35-98) | 0.487 |
| Gender – n (%)MaleFemale | 138 (65.1)74 (34.9) | 12 (57.1)10 (42.9) | 0.4680.468 |
| MV time (days) – median (IQR) | 3.73 (1-23) | 4.2 (1-12) | 0.345 |
| RSBI (bpm/L) – median (IQR) | 48.75 (5-190) | 46 (21-132) | 0.944 |
| MIP (cmH2O) – median (IQR) | 40 (16.3-120) | 40 (28-72) | 0.585 |
| MEP (cmH2O)- median (IQR) | 40 (12-120) | 38 (20-80) | 0.728 |
| Use of NIV – n (%) | 158 (68.7) | 12 (54.4) | 0.176 |
| Reintubation rate – n (%) | 30 (13.04) | 2 (9.1) | 0.594 |
IQR: interquartile range; MV: mechanical ventilation; RSBI: respiratory shallow breathing index; MIP: maximum inspiratory pressure; MEP: maximum expiratory pressure; NIV: noninvasive ventilation.
p-value<0.05 for significant differences between the variables of survivors and nonsurvivors.
Of the 252 patients studied, 58 (23%) were surgical patients. When we compared the surgical and medical patients, we found a significantly lower MV time among the surgical patients (a median of three days and an IQR of one to five days vs. a median of four days and an IQR of two to seven days; p =0.03). Although the surgical patients were younger than the medical patients (a median of 57 years and an IQR of 43 to 67 years vs. a median of 70 years and an IQR of 55 to 80 years; p =4.65, e-05), we found no differences in terms of the MIP, MEP, RSBI, and reintubation rate between these subgroups of patients.
DISCUSSIONThis study found that patients on MV who participated in the weaning protocol and were eligible for the SBT and extubation remained on invasive MV for an average of 3.7 days. Of these patients, 12.7% required reintubation, which represented weaning failure. Postextubation NIV was used in 73% of the patients, and 15% of these patients were reintubated.
Some studies have shown that unplanned strategies that identify patients who are not eligible for ventilatory support removal result in extended MV times (15-18). According to the results of these studies, assessments should be performed routinely in a standardized, formal and programmed manner, as this was shown to reduce the duration of MV (8) by up to two days in comparison to the MV time for patients who do not undergo routine, standardized assessments. Other protocols, such as the daily awakening protocol that includes a daily interruption of sedation, have previously been shown to predict reduced ventilatory support duration and shorter ICU and hospital stays (15,19,20) and should be applied in conjunction with the weaning protocol.
Ely et al. (8) showed that patients with a mean APACHE II score of 19.8 and whose spontaneous breathing capacity was assessed daily stayed on MV for 4.5 days (median) and presented a reintubation rate of 6%. Other authors (21,22) reported that up to 18% of patients who are removed from MV require reintubation within 72 hours. In our study, the median invasive MV time was 3.7 days, the median rate of reintubation was 12.7%, and the median APACHE II score was 22. Moreover, our study found that 73.2% of the patients studied were extubated and that NIV was used to assist in the ventilatory weaning process, which may help to explain the differences between our results and those of other studies.
In his review, Neil MacIntyre (9) addresses the fact that studies (20) presenting reintubation rates between 10 and 15% reflect the typical rates at most ICUs. Therefore, reintubation rates significantly higher or lower than those described in the literature should be assessed. A very low reintubation rate may reflect a routine that is too cautious and consists of a longer time period before the patients are taken off the ventilator. In contrast, a very high reintubation rate may represent a more aggressive routine that may remove patients from ventilation too soon. In our study, the percentage of reintubated patients was similar to that previously reported in the literature.
In the case of patients who were reintubated following successful SBT, the literature does not describe the various reasons as to why these patients required MV or the severity of these cases, and there is also no consensus as to the standard duration of MV or the presence of gas exchange disturbances (21). Only one study (22) reported differences between reintubated and successfully extubated patients according to age and found that older patients were more likely to require reintubation. In this study, there was no significant correlation between MV time and age, APACHE II score, RSBI, MIP, MEP, or the use of NIV postextubation.
In general, the most common reasons for reintubation are related to airway obstruction or acute respiratory failure (24). In this study, the reasons for reintubation varied, although the most common reasons included reduced consciousness, acute respiratory failure, and a lack of upper airway protection. Additionally, some authors have found the need for reintubation to be correlated with a greater incidence of MV-related pneumonia (6,25).
NIV can be used for the early treatment of patients with respiratory failure postextubation, and NIV has been proposed as a means to facilitate weaning from invasive MV. Reports in the literature have shown that for selected patients, predominantly those with COPD, NIV can decrease the number of deaths, reduce MV-related pneumonia rates, reduce the length of ICU and hospital stays, and reduce MV time. However, NIV has not been shown to affect weaning failures or MV time in relation to weaning (11,24). In this study, postextubation NIV was used in 73% of the patients, and 15% of these patients required reintubation and represented weaning failure.
The mortality rate in the studied patients was 8.73% (22 patients), and there was no correlation between the variables obtained from survivors and nonsurvivors. The reported hospital mortality rate of patients submitted to a weaning protocol ranges from 10 to 48%, although these studies used widely heterogeneous initial weaning criteria and protocols. Moreover, the reported mortality rates of patients submitted to a weaning protocol versus a conventional weaning process were not significantly different.
Few studies have reported data regarding the duration and success of MV for protocols that used planned strategies for selecting patients who would be eligible for the SBT, extubation and reintubation. If made available, these data could be used as a comparative index for different hospitals. Furthermore, programmed strategies systematized through medical protocols, training and continuing education for use in multidisciplinary teams, monitoring and informed outcome reports represent a future tool and source of quality markers of patient care.
The application of a specific weaning protocol resulted in low mechanical ventilation times and acceptable reintubation rates. Thus, this protocol can be used as a comparative index in hospitals to improve the MV weaning system and the monitoring and informative reporting of outcomes. Furthermore, this protocol may represent a future tool and quality marker for patient care.
We thank Oscar Fernando Pavão dos Santos for supporting the implementation of this weaning protocol in the hospital's ICU; Lucas Yutaka for helping to design the weaning protocol at the beginning of the project; the ICU's physical therapists for helping to implement and collect the data used in this retrospective study; and Alexandre Rodrigues Marra for reviewing the manuscript.
No potential conflict of interest was reported.
Silva CS and Timenetsky KT participated in the study design and data collection, performed the statistical analysis, and wrote the manuscript. Taniguchi C participated in the study design, data collection and manuscript writing. Calegaro S, Azevedo CS and Stus R participated in data collection. Matos GF, Eid RA and Barbas CSV participated in the study design. All of the authors read and approved the final manuscript.