Analysis of the death resulting from a deep sedation administered by a nonanesthetist physician who was convicted after a trial for manslaughter. A discussion is made of the potential impact of the adoption of the recently published recommendations for sedation by nonanesthetists, developed by the Sociedad Colombiana de Anestesiología (SCARE) along with other scientific societies.
© 2012 Sociedad Colombiana de Anestesiología y Reanimación. Published by Elsevier. All rights reserved.
Análisis del desenlace mortal de una sedación profunda por un médico no anestesiólogo, que después de un proceso legal terminó en una condena en los Estados Unidos. Se hace una discusión del potencial impacto de la implementación de las recomendaciones recientemente publicadas, para la sedación por no anestesiólogos, desarrolladas por la Sociedad Colombiana de Anestesiología (SCARE) en conjunto con otras sociedades científicas en la seguridad de estos procedimientos.
© 2012 Sociedad Colombiana de Anestesiología y Reanimación. Publicado por Elsevier. Todos los derechos resevados.
The development of recommendations for sedation by non-anesthesiologists is subject to serious discussions among the interested parties all over the world. Likewise, in Colombia, this has hampered the possibility of creating standards; however their need is obvious, as cases of lethal outcomes that could be prevented with adherence to explicit safety strategies, occasionally happen. Preventable lethal outcomes do not occur exclusively in developing countries. The recent death of a celebrity, Michael Jackson, in the United States has put the problem of not complying with appropriate safety standards during sedation under the spotlight. This review analyzes the case of the deceased artist from the perspective of the recently developed recommendations for sedation by non-anesthesiologists in Colombia.
Case recordAccording to the transcriptions available from the interview of his physician, the cardiologist Conrad Murray, with the police,1Michael Jackson had major sleeping problems. To address this situation, Jackson hired Murray two months before his death to provide combinations of medications, benzodiazepines and propofol, in order to sleep.
According to his own testimony, on June 25, 2009 the physician was managing Jackson's chronic insomnia. After prescribing 10 mg of oral diazepam without any sleep induction, he inserted an intravenous catheter in the leg, gave 2 mg of lorazepam, and after observing minimal effects he gave another 2 mg of midazolam, again without major effect.
In this situation the patient indicated he wanted “milk” (the denomination Jackson gave to propofol) to which Murray complied, administering 25 mg of propofol with lidocaine, to minimize injection pain. According to Murray the patient fell asleep with an oxygen saturation of 90%, and a heart rate of 70 bpm (measured with a finger oximeter, Nonin-Onyx).
The physician said he left the patient alone for a few minutes, and when he returned he found him in apnea with a femoral heart rate of 122 bpm. He described no further details on the pulse oximetry or on the electrocardiographic monitoring or capnography. He began cardiac compressions. Afterwards, he provided mouth-to-mouth resuscitation, administered flumazenil, and then called help on 911.
Paramedics arrived and after 20 min. of resuscitation maneuvers Jackson remained in pulseless electrical activity (PEA), for which they decided to pronounce him dead on site. However, because of Murray's insistence he was transferred to a medical center where after all types of maneuvers, including insertion of an aortic counter pulsation balloon, he was declared dead 40 min. later.1 Unfortunately, Murray did not inform the paramedics nor the physicians at the medical center of the medications administered to Jackson previous to his death.
The patient's autopsy revealed high blood levels (2.62 μg/mL) of propofol (it has to be considered that surgical anesthesia is achieved with levels below 2 μg/mL). High blood (169 ng/mL) and stomach levels of lorazepam were found which suggested almost simultaneous oral and intravenous administration. Lidocaine (0.84 mcg/mL) was found in blood, midazolam (4.6 ng/mL) and diazepam (less than 0.1 mcg/mL) were found in the heart. It should be noted that there was absence of any level of alcohol, barbiturates, cocaine, marijuana, amphetamines or any opioid. The autopsy also revealed excellent physical conditions of the patient and the absence of atherosclerosis.2
Several physicians participated in the trial, including a cardiologist, an internist expert in sleep disorders and two anesthesiologists, one as a witness of the prosecution and the other of the defense.
On November 7, 2011 the jury gave a guilty verdict to Conrad Murray. On November 27, 2011 the judge sentenced him to four years in jail stating that Murray had committed criminal negligence in medical care and on his insistence of not admitting these errors, he represented a danger to society.
Development of sedation recommendations in ColombiaIn Colombia, after a fatal outcome related to sedation in 2010, the health authorities of Bogota identified a total lack of recommendations or guidelines for sedation by non-anesthesiologists. Considering that anesthesiologists are by definition the experts in sedation, they requested the Sociedad Cundinamarquesa de Anestesiología (SCA) to develop safety recommendations for non-anesthesiologists.
The SCA asked a group of sedation experts to develop them, and shortly thereafter this initiative was transferred to the Safety Committee of the Sociedad Colombiana de Anestesiología y Reanimación (SCARE) in which some of these experts continued their participation.
The work of this ad hoc sedation committee included an extensive review of many sedation recommendations previously published elsewhere; after which a document was written,3 to be used as the basis for public discussion in forums with authorized delegates from most of the scientific societies interested in the topic.
After almost 10 meetings (either held at the Secretaría de Salud del Distrito headquarters, at a forum in Congreso Colombiano de Anestesiología, in Medellín in March 2011, or virtual using the interactive resources of SCARE), 22 modifications where made until the final document was approved by the leadership of seven scientific societies on July 21, 2011. Simultaneously, the development of recommendations for sedation of patients under 12 years old by non-anesthesiologists was directed by the Pediatric Anesthesia committee of SCARE with support of the Safety committee. The main concepts of the adult sedation document are:
- a)
Consideration that with the adoption of safety recommendations most complications are preventable during sedation by non-anesthesiologists.
- b)
The adoption of international definitions of sedation levels and the restriction of sedation by non-anesthesiologist's to level I (anxiolysis) and level II (minor to moderate sedation). The compliance to this recommendation is easier with the recommendation of using only one medication for sedation.
- c)
Deep sedation (level III) can only be performed by a non-anesthesiologists when a list of strict criteria are met, this with the goal to effectively limit its practice. Otherwise this level of sedation can only be performed by an anesthesiologist.
- d)
Sedation must be provided by a trained individual different to whoever practices the procedure. Training is explicit and requires the passing of a theoretical-practical course specifically designed for the administration of sedation level I and II.
The final goal of this document is to regulate the chaotic practice of sedation in Colombia, where it is common that non-anesthesiologists provide deep sedations (level III), in which general anesthesia (level IV) can intermittently happen, exposing the patients to very high risks, as well as breaking the law, as general anesthesia is only allowed to be provided by graduated anesthesiologists in Colombia.
The recommendations published in this issue of the Colombian Journal of Anesthesia4 draw a middle line between the expectations of non-anesthesiologists who mistakenly extrapolate the international experience in sedation and consider that they should not be restricted in performing deep sedation,5 and the expectations of some anesthesiologists who consider that all sedation or the use of some medications, like propofol, be restricted to exclusive anesthesiologist practice.6,7
Even though there is abundant literature suggesting the safety of sedation (even deep sedation) by non-anesthesiologists, this same literature consistently addresses safety strategies that are not easily implemented in the country's practice (like expertise in advanced airway management, that requires periodical re-training; for example, how many gastroenterologists in Colombia, refresh their competencies briefly obtained during an ICU rotation? Or refresh formal training in sedation, monitoring expertise, including capnography, and biannual ACLS certification, among other competencies?).
There are in fact small local case series of sedation in endoscopy, including the use of propofol, that report proper safety, however these are small samples (in the literature death rates of 4/646,000 patients are reported among sedation by non-anesthesiologists are reported).8 In addition, these series described high standards of monitoring and training, which rarely are available in the country, a situation that can be related to the potentially preventable tragic outcomes which are not uncommon in the country.
In 2004 the Journal of the Asociación Colombiana de Gastroenterología grouped four papers about this topic, which conclude basically the same recommendations established in the consensus, which are: high levels of training (1), high levels of monitoring (SpO2, EKG and EtCO2) and backup support for the sedation. These, unfortunately, are not universal in the country.3,10-12
On the other hand, the anesthesiologist is, by definition, an expert in sedation, as general anesthesia is the end of the continuum of sedation. However, in no country in the world is sedation level I or II considered to be an exclusive activity of anesthesiologists. The argument that a single dose of any sedative can lead to deep sedation (or even general anesthesia) is possible, but the training proposed, intends to minimize this risk as much as possible.
Regarding propofol, the situation is different, as there are strong debates between those who consider it as an exclusive medication to be used by anesthesiologists and those who consider that it can be used by non-anesthesiologists with restrictions.
There are literature reports describing hundreds of thousands of cases using propofol for sedation during endoscopy with minimal morbidity. This has supported the development of guidelines for the use of propofol by non-anesthesiologists both in the United States13 and in Europe. In the United States, the use propofol by non-anesthesiologists is almost universal during endoscopy. However Medicare, the health care insurance for individuals above 65 years old, did not allow the use of propofol by non-anesthesiologists, related to the fact that the FDA (Food and Drug Administration, United States government agency regulating medications) has established that the drug insert explicitly indicates that whoever administers the medication should have anesthesia expertise.
The heated debate on regulating sedation is long-standing. In the United States sedation guidelines for non-anesthesiologists14 have been subject of great criticism, and achieving the balance between positions is complex.15
In Europe, in December 2010, the European Societies of Gastroenterology and Endoscopy, jointly with the European Society of Anesthesia (ESA), published guidelines for the use of propofol by non-anesthesiologists.16 Interestingly these guidelines generated a major uproar by 21 national European societies of anesthesia, who condemned them and in a general assembly, the sponsorship of these guidelines was voted to be withdrawn.17 However three major national societies (German, English and French) did not adhere to this position. Several distinguished anesthesia professors questioned this prohibition of propofol use by non-anesthesiologists as a fundamentalist and populist measure, because even though it seems reasonable, it has no literature support.18
When these recommendations for Colombia were developed, there was a consideration that propofol use among endoscopists is popular, so instead of prohibiting its use, it was regulated, specifying that it should be used only to achieve sedation level I and II, and that it should not be used with other medications commonly used, like opioids and benzodiazepines, because the combination of medications increases exponentially the risk of complications, and whoever administers sedation in Colombia rarely has the competencies to avoid clearly preventable complications, which can lead to fatal or serious adverse outcomes, as has effectively happened in the country with rates higher than those reported in the literature. This is a reality that developed countries had 20 years ago, when almost a hundred of deaths with sedation were reported, almost all by non-anesthesiologists, and clearly related to poor safety standards.19
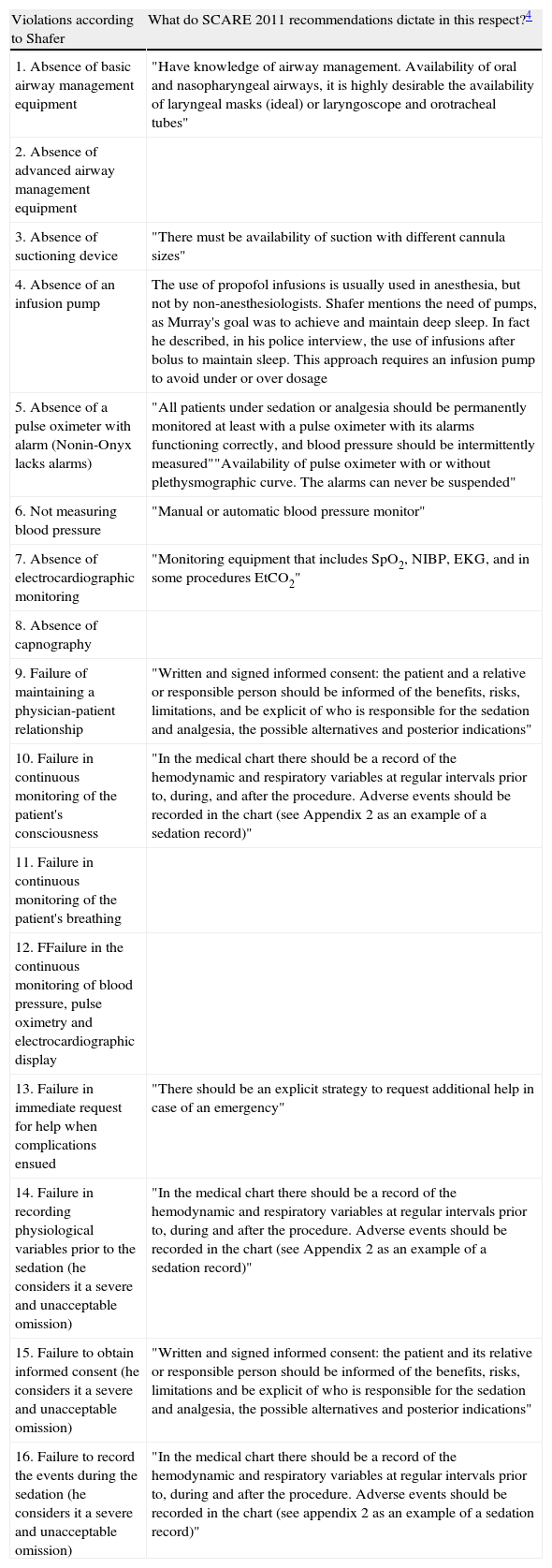
Case analysisThe case described above is appropriate to discuss the relevance of adherence to safety recommendations in sedation. Steven Shafer, an anesthesiologist expert witness for the prosecution, Professor of Anesthesia at Columbia University, and a renowned authority in the pharmacology of intravenous agents, as well as author of the insert of the propofol ampoules available in the United States, made an excellent analysis of the safety standards Conrad Murray breached. This author describes 17 flagrant violations from his point of view, of which 16 are relevant for the issue of sedation (table 1).20
List of the safety violations identified by Steven Shafer related to the SCARE recommendations
| Violations according to Shafer | What do SCARE 2011 recommendations dictate in this respect?4 |
| 1. Absence of basic airway management equipment | "Have knowledge of airway management. Availability of oral and nasopharyngeal airways, it is highly desirable the availability of laryngeal masks (ideal) or laryngoscope and orotracheal tubes" |
| 2. Absence of advanced airway management equipment | |
| 3. Absence of suctioning device | "There must be availability of suction with different cannula sizes" |
| 4. Absence of an infusion pump | The use of propofol infusions is usually used in anesthesia, but not by non-anesthesiologists. Shafer mentions the need of pumps, as Murray's goal was to achieve and maintain deep sleep. In fact he described, in his police interview, the use of infusions after bolus to maintain sleep. This approach requires an infusion pump to avoid under or over dosage |
| 5. Absence of a pulse oximeter with alarm (Nonin-Onyx lacks alarms) | "All patients under sedation or analgesia should be permanently monitored at least with a pulse oximeter with its alarms functioning correctly, and blood pressure should be intermittently measured""Availability of pulse oximeter with or without plethysmographic curve. The alarms can never be suspended" |
| 6. Not measuring blood pressure | "Manual or automatic blood pressure monitor" |
| 7. Absence of electrocardiographic monitoring | "Monitoring equipment that includes SpO2, NIBP, EKG, and in some procedures EtCO2" |
| 8. Absence of capnography | |
| 9. Failure of maintaining a physician-patient relationship | "Written and signed informed consent: the patient and a relative or responsible person should be informed of the benefits, risks, limitations, and be explicit of who is responsible for the sedation and analgesia, the possible alternatives and posterior indications" |
| 10. Failure in continuous monitoring of the patient's consciousness | "In the medical chart there should be a record of the hemodynamic and respiratory variables at regular intervals prior to, during, and after the procedure. Adverse events should be recorded in the chart (see Appendix 2 as an example of a sedation record)" |
| 11. Failure in continuous monitoring of the patient's breathing | |
| 12. FFailure in the continuous monitoring of blood pressure, pulse oximetry and electrocardiographic display | |
| 13. Failure in immediate request for help when complications ensued | "There should be an explicit strategy to request additional help in case of an emergency" |
| 14. Failure in recording physiological variables prior to the sedation (he considers it a severe and unacceptable omission) | "In the medical chart there should be a record of the hemodynamic and respiratory variables at regular intervals prior to, during and after the procedure. Adverse events should be recorded in the chart (see Appendix 2 as an example of a sedation record)" |
| 15. Failure to obtain informed consent (he considers it a severe and unacceptable omission) | "Written and signed informed consent: the patient and its relative or responsible person should be informed of the benefits, risks, limitations and be explicit of who is responsible for the sedation and analgesia, the possible alternatives and posterior indications" |
| 16. Failure to record the events during the sedation (he considers it a severe and unacceptable omission) | "In the medical chart there should be a record of the hemodynamic and respiratory variables at regular intervals prior to, during and after the procedure. Adverse events should be recorded in the chart (see appendix 2 as an example of a sedation record)" |
It should be noted that in this case Conrad Murray's goal was to achieve deep sedation (Level III) or general anesthesia (Level IV) and not Level I or II sedation. When this case is analyzed considering the recommendations approved in Colombia, it is clear that almost all the safety issues identified by Shafer, which according to his testimony could all independently be lethal, could be preventable with adherence to these published recommendations.
It is important to pin point that anesthesiologists who provide sedation are subject to the 2009 SCARE Minimal Standards for anesthesia practice in Colombia,21 which are more strict, as the sedation by anesthesiologists can be as deep as level IV (general anesthesia), and therefore the safety standards are higher. For example they require permanent monitoring of capnography and the electrocardiograph, among others. Several recent studies show the adherence to these standards in anesthesiologist administered sedations in Colombia.20,22
ConclusionsSafe sedation is a goal that should be actively pursued, as most of the morbidity is related to poor adherence to established recommendations.
The efforts of the Safety Committee of SCARE, jointly with the other seven societies interested in the topic has made the published consensus possible with the intention of regulating the practice of sedation by non-anesthetists in Colombia.
The concerns of health authorities are such that in the process of updating resolution 1043 of institutional certification, these recommendations will be included as mandatory to obtain permission to offer these services. It is expected that as result of this initiative, the patient's safety during sedation will improve significantly in Colombia.
Competing InterestsPedro Ibarra is coauthor of the National Consensus: Recommendations for the sedation and analgesia by non-anesthesiologist physicians and dentists in patients older than 12.
Funding sources: The author's own resources.