Objective: To determine whether preoperative anemia in patients undergoing cardiovascular surgery is associated with higher mortality, renal failure, cerebrovascular accidents and cardiovascular events as compared to patients with normal preoperative levels of hemoglobin.
Methods: A systematic review and a meta-analysis of the cohort observational and of cases and control studies was conducted, exploring the association between the pre-surgical levels of hemoglobin and adverse outcomes in patients undergoing cardiovascular surgery. The MEDLINE, EMBASE, and COCHRANE data-bases up to the 50th week of 2010 were consulted. The studies that complied with the inclusion criteria were independently selected. The sources of heterogeneity among the studies were assessed, including publication bias.
Results: Of the total number of studies reviewed, 260 were identified; sufficient data could be extracted from 11 of them to combine the mortality outcome. Out of these studies, 6 were adjusted for severity and comorbidities, while the results of the remaining ones were not adjusted.
Conclusions: Anemic patients undergoing cardiac surgery have a higher risk of postoperative adverse events. There are several factors limiting the interpretation of the data, including a poor standardized definition of anemia, and the lack of studies explicitly designed to quantify the prevalence and the impact of anemia in patients with cardiovascular diseases.
© 2012 Sociedad Colombiana de Anestesiología y Reanimación. Published by Elsevier. All rights reserved.
Objetivo: Determinar si la anemia preoperatoria en los pacientes que son llevados a cirugía cardiovascular se asocia al aumento de la mortalidad, falla renal, accidentes cerebovasculares y eventos cardiovasculares cuando se comparan sus casos con los de pacientes con niveles de hemoglobina normales en el preoperatorio.
Métodos: Se realizó una revisión sistemática y un metaanálisis de los estudios observacionales de cohorte y de casos y controles que exploraron la asociación entre los niveles de hemoglobina prequirúrgica y los desenlaces adversos de los pacientes sometidos a cirugía cardiovascular. Se consultaron las bases de datos MEDLINE, EMBASE, y COCHRANE hasta la semana 50 de 2010; de manera independiente, fueron seleccionados los estudios que cumplieron con los criterios de inclusión. Se evaluaron las fuentes de heterogeneidad entre los estudios, como el sesgo de publicación.
Resultados: De los estudios revisados se identificaron 260; entre dichos estudios, de 11 se pudieron extraer los datos suficientes para combinar el desenlace de mortalidad. De esos estudios, 6 se ajustaron por severidad y comorbilidades, mientras que en los restantes sus resultados no fueron ajustados; aun así se observó un incremento en el riesgo de mortalidad cuando se considera la anemia como variable independiente.
Conclusiones: Los pacientes anémicos sometidos a cirugía cardiaca tienen un mayor riesgo de sufrir eventos adversos postoperatorios. Varios factores más también limitan la interpretación de los datos, incluyendo la falta de una definición uniforme de la anemia y la carencia de estudios expresamente diseñados para cuantificar la prevalencia y el impacto de la anemia en pacientes con enfermedades cardiovasculares.
© 2012 Sociedad Colombiana de Anestesiología y Reanimación. Publicado por Elsevier. Todos los derechos resevados.
The World Health Organization (WHO) defines anemia as a Hb<13 g/dl for men and Hb<12 g/dL for women. Some observational studies have established the association between preoperative anemia and increased post-surgical complications in patients undergoing non-cardiac surgery. Such increased risk is attributed to the confounding effect of transfusions and the interactions between the comorbidities and low Hb levels.
One of the first studies to report such association was Carson's et al., in 1958, which was conducted on Jehovah's Witnesses patients undergoing non-cardiac surgery.1, 2 The study determined that the low preoperative hemoglobin levels and the intraoperative blood loss, increased the risk of morbidity and mortality; the risk was much higher when the patients had cardiovascular disease.
Hardy et al.3 studied the association between the levels of hemoglobin 24 hours after surgery and morbidity in 2,664 heart surgery patients. These authors found that lower hemoglobin concentrations were associated with higher hemodynamic instability and renal failure, while Nelson et al.4 found that a postoperative hematocrit less than 28 was associated with significant myocardial ischemia and a higher number of cardiac events.
Other studies were unable to find increased cardiac or noncardiac related events associated with preoperative anemia in cardiovascular surgical patients,5 whilst treatment of anemia with red blood cells transfusion was associated with a 21% increased risk of adverse events per each unit of transfused red blood cells.4
The objective of this paper was to review the available evidence with respect to the association between anemia and adverse outcomes in patients undergoing cardiac revascularization surgery or valve replacement, as compared to normal hemoglobin patients.
MethodsA systematic literature review was performed by consulting the digital data bases: MEDLINE, EMBASE, COCHRANE up until week 50 of the year 2010 and using the following search strategy:
(((((((((((revascularization)) OR ((cardiac surgery))) OR ((CPB))) OR ((cardiopulmonary bypass))) OR ((Bypass Graft Surgery))) OR ((ischemic heart disease)))) AND (((((Hb) OR ((Hemoglobin))) OR ((Hb concentration))) OR ((Hb))))) AND (((((((Death)) OR ((Mortality))) OR ((kidney failure))) OR ((outcomes))) OR ((Cardiovascular Outcome)))) AND ((Humans[Mesh]) AND (adult[MeSH])))) AND ((((Hemoglobin levels AND ((Humans[Mesh]) AND (adult[MeSH])))) OR ((Hemoglobin levels normal AND ((Humans[Mesh]) AND (adult[MeSH])))) AND ((Humans[Mesh]) AND (adult[MeSH])))) AND ((Humans[Mesh]) AND (adult[MeSH]))
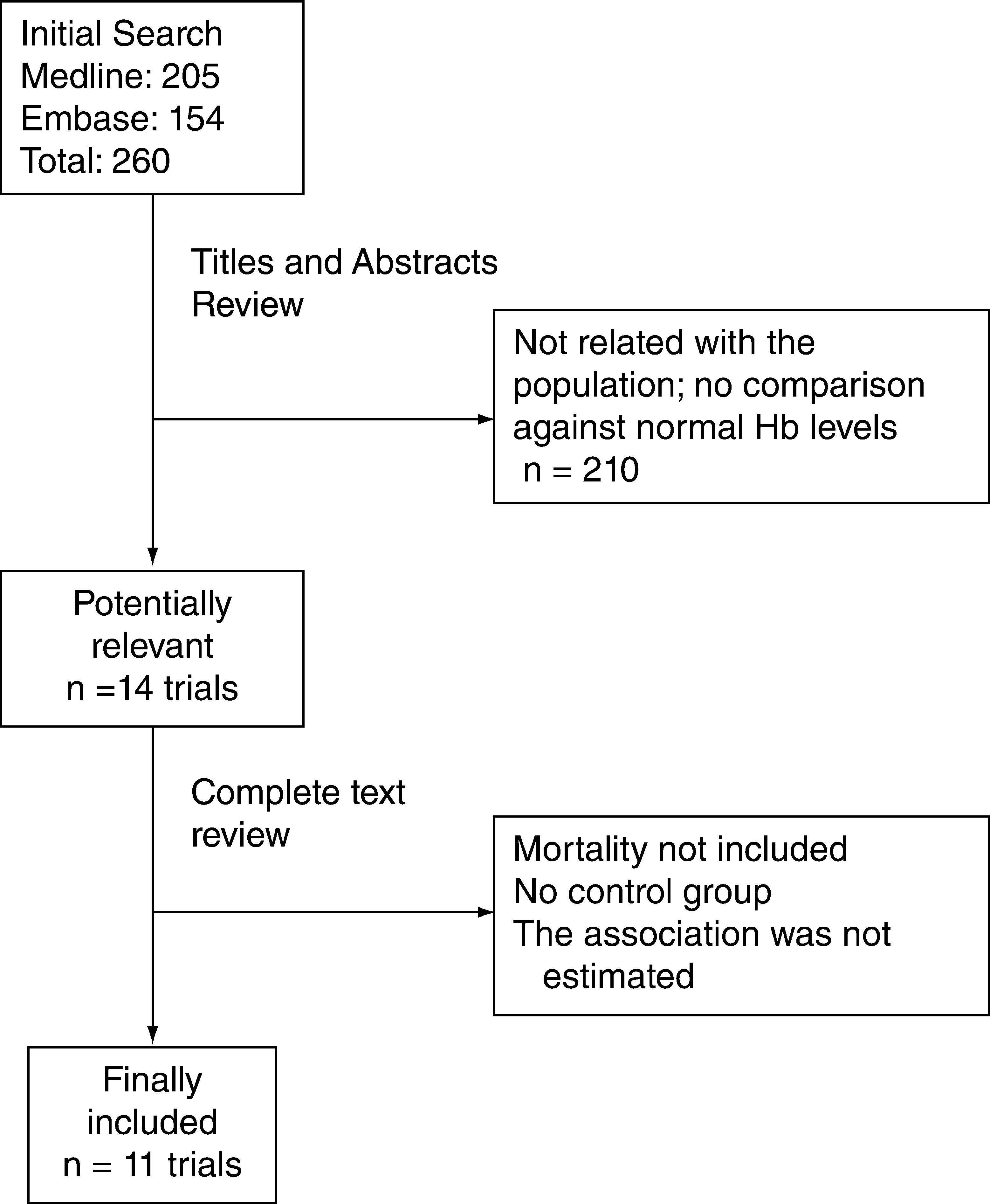
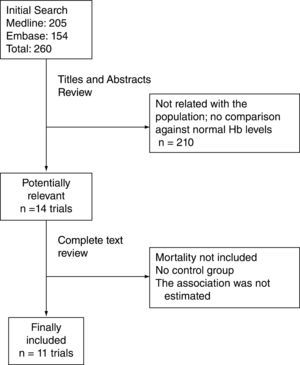
As seen from the flowchart (fig. 1), 260 studies were initially identified; 2 reviewers, HO and EB, independently verified all the abstracts, taking into account the following selection criteria: that the trials were case and control or cohort studies; that they included cardiac revascularization surgery or valve replacement and additionally, that suboptimal Hb levels were compared against normal Hb levels for outcomes of renal failure and ICU stay; the relevant studies were chosen to obtain the information.
Obtaining the InformationData on the type of population, the categories of comparative hemoglobin levels, the types of outcomes reported, and the levels of hemoglobin deemed normal, were all extracted from every trial. HO and EB completed these processes independently. Any disagreements were solved by consensus.
Analysis of the InformationThe analysis of the results of the individual studies was done using the statistical packages, CMA (Biostat, 14 North Dean Street, Englewood, NJ 0763) and STATA 9.0. In order to obtain the summarized measures, the Odds ratios for occurrence of cardiac events and mortality were used when comparing patients with low Hb levels against normal Hb levels. These measures were combined using the fixed and random effects model for binary outcomes.
According to the plan, the subgroup analyses were done within various population categories, such as the different levels of hemoglobin considered for the measurements of the trials reporting mortality. The same approach was used for the studies that reported outcomes of adverse events.
The heterogeneity was assessed using Forest plots and Q and 12 tests, for each of the sub-groups analysis, in order to determine the sources of heterogeneity; likewise, a sensitivity analysis was done of the summary measurement for those trials where the results were adjusted for severity and comorbidity; this analysis was compared against the results of the non-adjusted trials.1, 6-15
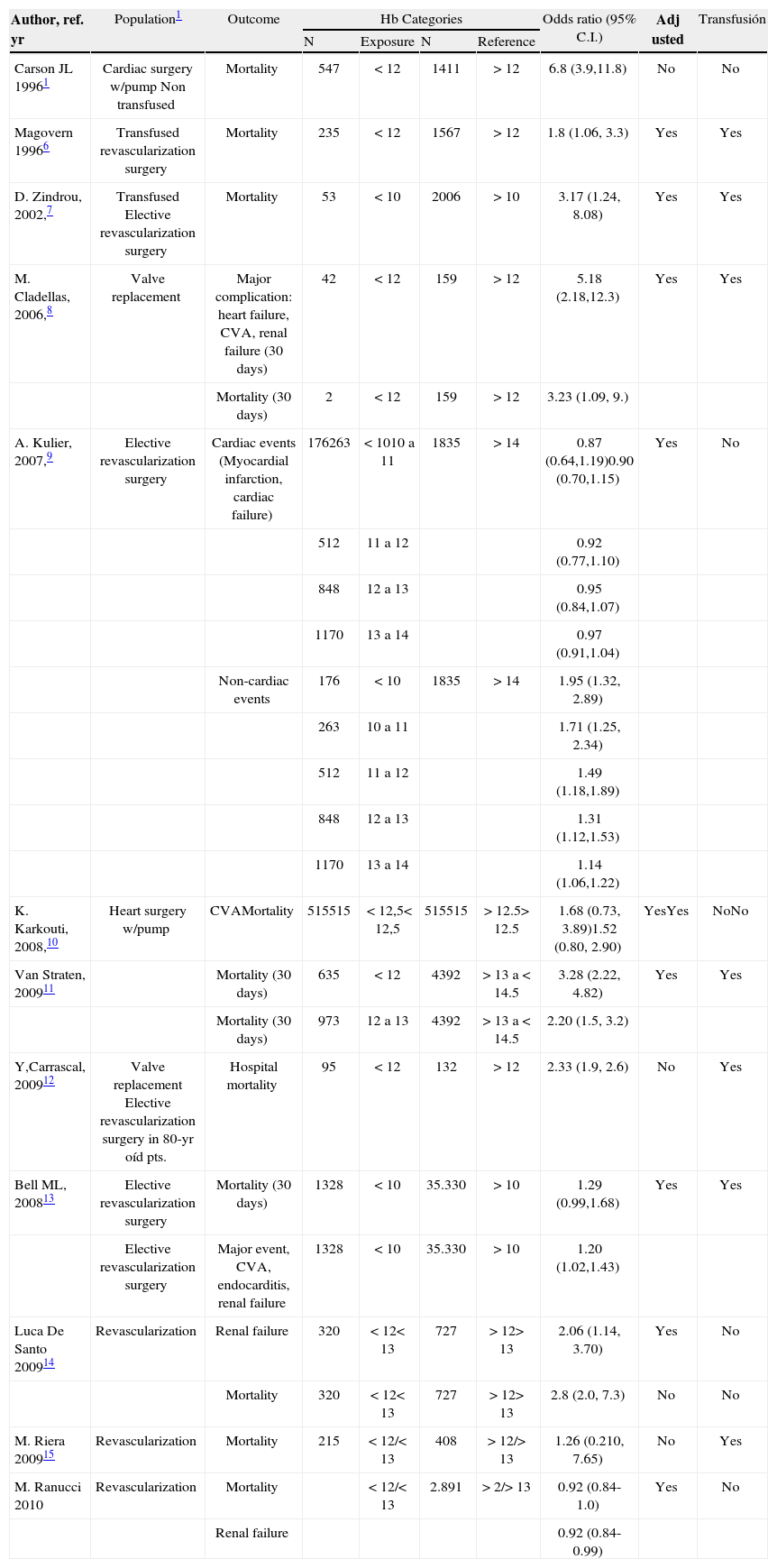
ResultsAs shown in the flowchart (fig. 1), 11 trials met the inclusion criteria; two of them included cardiac revascularization patients; two others did not discriminate the type of cardiac surgery and another included valve replacement patients.8
The studies also differed in terms of the variables considered for the adjustment, as well as the cut-off points for hemoglobin to compare anemic versus non-anemic patients (table 1). The study by Kulier's et al16 makes an adjustment based on the Euroscore <4 and ≥4, and the number of transfused units; hence, there is an association with cardiac and non-cardiac adverse events and a Hb level below 11 g/dl.
Studies published evaluatíng preoperative hemoglobin and cardiovascular surgical outcomes
| Author, ref. yr | Population1 | Outcome | Hb Categories | Odds ratio (95% C.I.) | Adj usted | Transfusión | |||
| N | Exposure | N | Reference | ||||||
| Carson JL 19961 | Cardiac surgery w/pump Non transfused | Mortality | 547 | <12 | 1411 | >12 | 6.8 (3.9,11.8) | No | No |
| Magovern 19966 | Transfused revascularization surgery | Mortality | 235 | <12 | 1567 | >12 | 1.8 (1.06, 3.3) | Yes | Yes |
| D. Zindrou, 2002,7 | Transfused Elective revascularization surgery | Mortality | 53 | <10 | 2006 | >10 | 3.17 (1.24, 8.08) | Yes | Yes |
| M. Cladellas, 2006,8 | Valve replacement | Major complication: heart failure, CVA, renal failure (30 days) | 42 | <12 | 159 | >12 | 5.18 (2.18,12.3) | Yes | Yes |
| Mortality (30 days) | 2 | <12 | 159 | >12 | 3.23 (1.09, 9.) | ||||
| A. Kulier, 2007,9 | Elective revascularization surgery | Cardiac events (Myocardial infarction, cardiac failure) | 176263 | <1010 a 11 | 1835 | >14 | 0.87 (0.64,1.19)0.90 (0.70,1.15) | Yes | No |
| 512 | 11 a 12 | 0.92 (0.77,1.10) | |||||||
| 848 | 12 a 13 | 0.95 (0.84,1.07) | |||||||
| 1170 | 13 a 14 | 0.97 (0.91,1.04) | |||||||
| Non-cardiac events | 176 | < 10 | 1835 | >14 | 1.95 (1.32, 2.89) | ||||
| 263 | 10 a 11 | 1.71 (1.25, 2.34) | |||||||
| 512 | 11 a 12 | 1.49 (1.18,1.89) | |||||||
| 848 | 12 a 13 | 1.31 (1.12,1.53) | |||||||
| 1170 | 13 a 14 | 1.14 (1.06,1.22) | |||||||
| K. Karkouti, 2008,10 | Heart surgery w/pump | CVAMortality | 515515 | < 12,5< 12,5 | 515515 | >12.5>12.5 | 1.68 (0.73, 3.89)1.52 (0.80, 2.90) | YesYes | NoNo |
| Van Straten, 200911 | Mortality (30 days) | 635 | < 12 | 4392 | >13 a <14.5 | 3.28 (2.22, 4.82) | Yes | Yes | |
| Mortality (30 days) | 973 | 12 a 13 | 4392 | >13 a <14.5 | 2.20 (1.5, 3.2) | ||||
| Y,Carrascal, 200912 | Valve replacement Elective revascularization surgery in 80-yr oíd pts. | Hospital mortality | 95 | < 12 | 132 | >12 | 2.33 (1.9, 2.6) | No | Yes |
| Bell ML, 200813 | Elective revascularization surgery | Mortality (30 days) | 1328 | <10 | 35.330 | >10 | 1.29 (0.99,1.68) | Yes | Yes |
| Elective revascularization surgery | Major event, CVA, endocarditis, renal failure | 1328 | <10 | 35.330 | >10 | 1.20 (1.02,1.43) | |||
| Luca De Santo 200914 | Revascularization | Renal failure | 320 | <12<13 | 727 | >12>13 | 2.06 (1.14, 3.70) | Yes | No |
| Mortality | 320 | <12<13 | 727 | >12>13 | 2.8 (2.0, 7.3) | No | No | ||
| M. Riera 200915 | Revascularization | Mortality | 215 | <12/<13 | 408 | >12/>13 | 1.26 (0.210, 7.65) | No | Yes |
| M. Ranucci 2010 | Revascularization | Mortality | <12/<13 | 2.891 | > 2/>13 | 0.92 (0.84-1.0) | Yes | No | |
| Renal failure | 0.92 (0.84-0.99) | ||||||||
Zindrou7 determined patient mortality with Hb≤10 g/dl and compared it against patients with Hb>10 g. Also, Cladellas8 studied 201 patients undergoing valve replacement with a view to determinining the Hb value that best predicts mortality; he identified a Hb cut-off point of 12 g/dl; thus, Hb<12 g/dl was an independent risk factor for mortality in this group of patients.
Karkouti10 used a cut-off point of Hb less than 12.5 g/dl; patients with this value were considered anemic and were compared against the non-anemic patients in terms of CVA hospital mortality or acute renal failure, when adjusted for confounding variables such as comorbidity, surgical factors, institution or transfusion.
Finally, Melanie L. Bell13 used different Hb categories in the population studied; she found no differences in mortality, but there were differences in morbidity with Hb>10 adjusted for comorbidity.
The above information shows that each trial used different cut-off points to define anemia. Furthermore, each trial included different variables for statistical adjustment; moreover, none of them established the time frame for the occurrence of preoperative anemia, and this could be the result of an acute or a chronic condition.
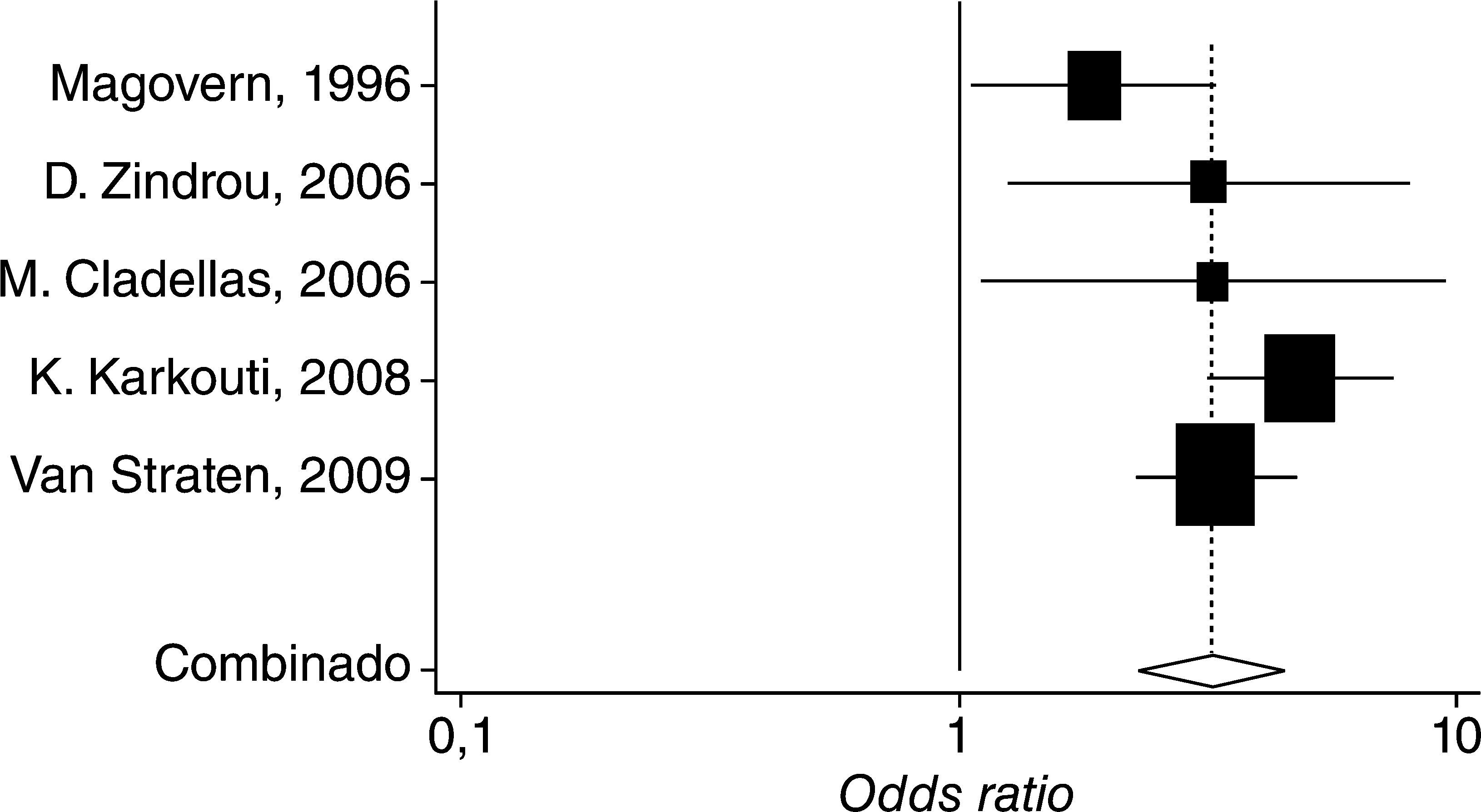
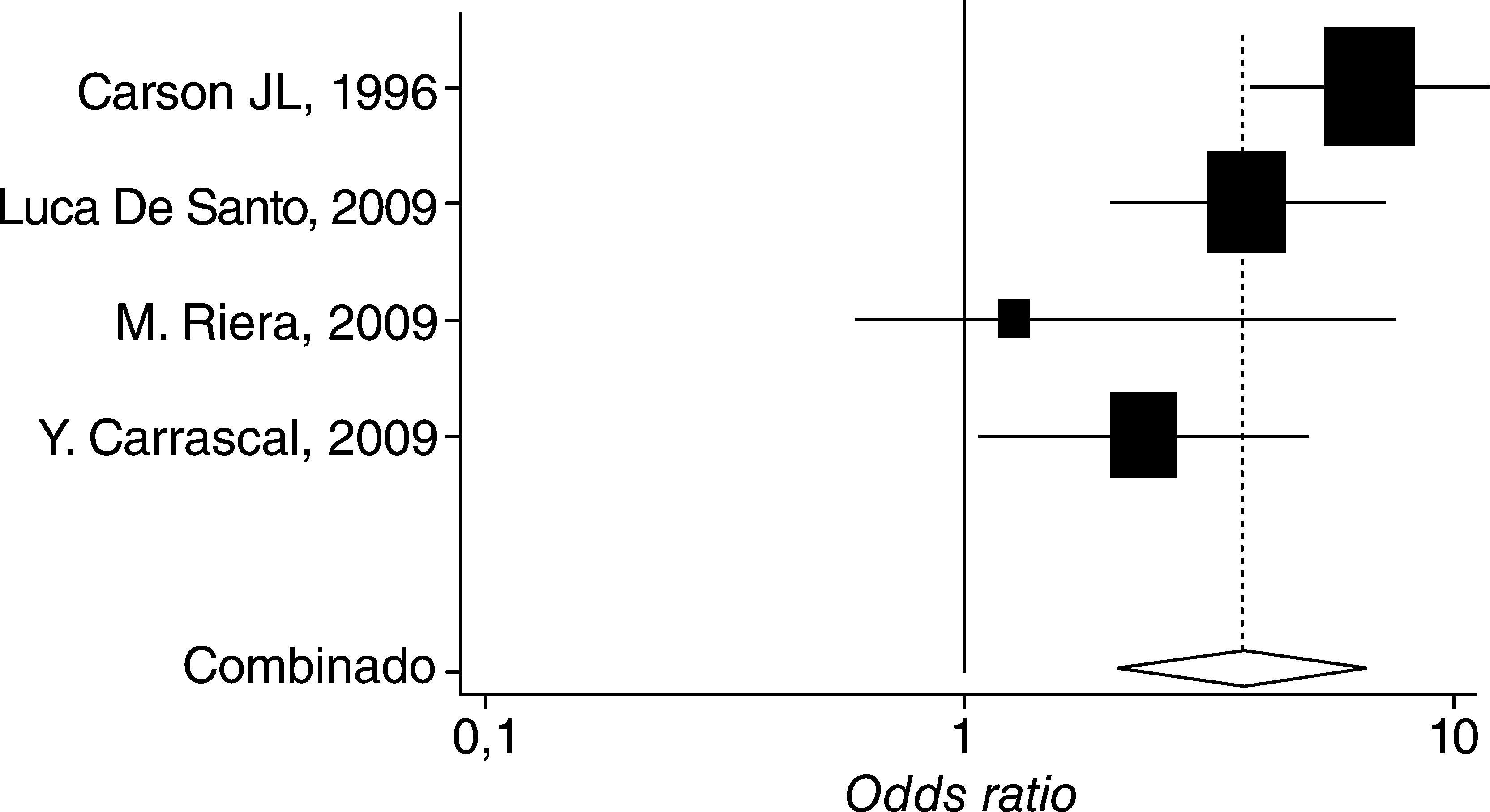
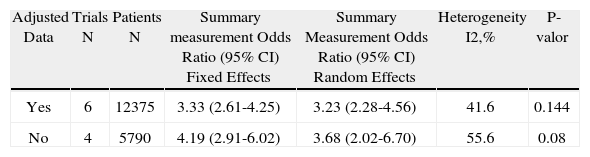
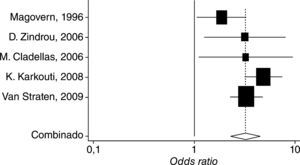
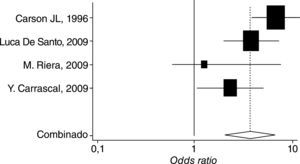
This can also be explained in terms of the heterogeneity of the results, which differ widely among the various trials, as shown in figure. 2 and table 2, using the Forest plot,8 the summary measurements for the various trials that reported mortality independently, adjusted and non-adjusted results for severity and comorbidity, in addition to the estimated values obtained with the fixed and random effect models.
Sub-Group Analysis of mortality Odds Ratio depending on whether the results of the trials are adjusted or not
| Adjusted Data | Trials N | Patients N | Summary measurement Odds Ratio (95% CI) Fixed Effects | Summary Measurement Odds Ratio (95% CI) Random Effects | Heterogeneity I2,% | P-valor |
| Yes | 6 | 12375 | 3.33 (2.61-4.25) | 3.23 (2.28-4.56) | 41.6 | 0.144 |
| No | 4 | 5790 | 4.19 (2.91-6.02) | 3.68 (2.02-6.70) | 55.6 | 0.08 |
I2%, Percent Variance attributed to heterogeneity of studies
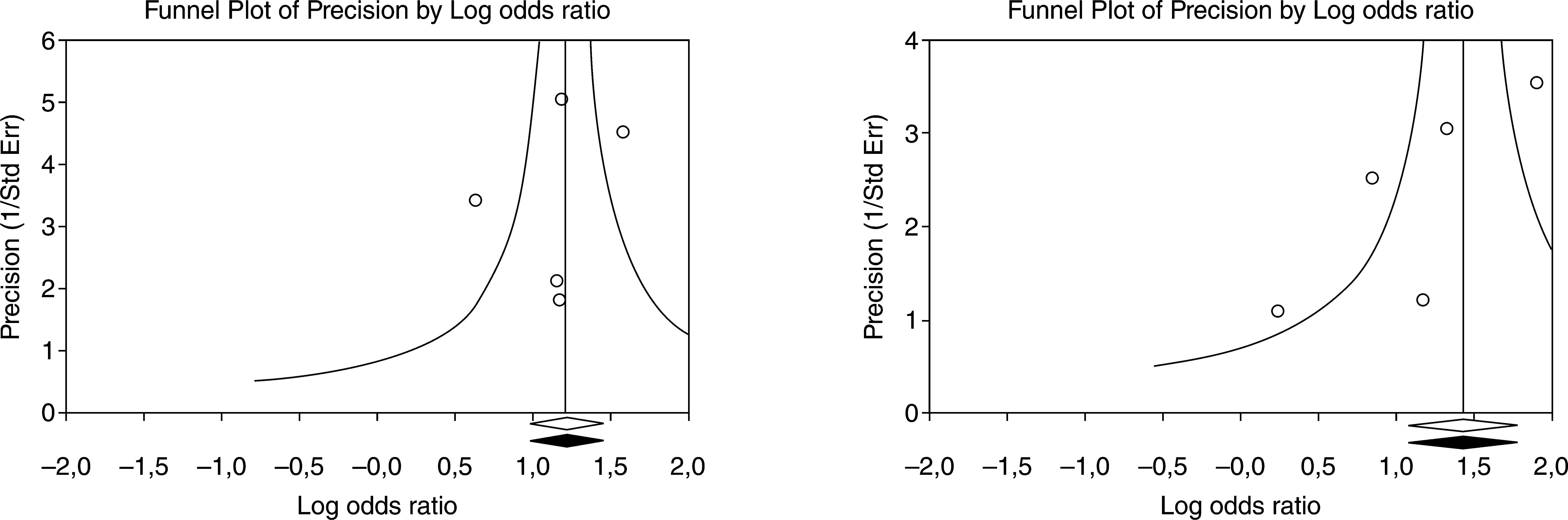
Finally, the publication bias was explored with a graphic representation of the scatter of the trials, taking into account the distance with regards to the summary measurement in accordance with its accuracy, as shown in figure 3.
Several trials with cardiovascular patients support the finding that preoperative anemia is associated with an increased number of adverse events; however, such results may be confounded by the pump effect and the comorbidities present in these patients.1, 4, 7, 17-20
The results of the combined studies are also derived from studies that evaluated the preoperative hemoglobin and adjusted based on the various comorbidities. The specific risk estimate is conclusive, in that the low levels of preoperative hemoglobin represent a risk factor for mortality and morbidity in patients undergoing cardiovascular surgery.
The benefit of correcting preoperative anemia has been shown in cancer patients and in orthopedic surgery; the rate of postoperative complications has been lowered with erythropoietin treatment.21 However, the Hb level to determine the need for transfusion has not been clearly established; as has been thoroughly documented, transfusion increases the risk of developing adverse events.22 The overall recommendation is to transfuse whenever the Hb level is below 7–8 g/dl.
Moreover, in a study with 179 surgical cardiovascular patients, Karkouti10 found no differences in terms of the risk of adverse outcomes with these levels of preoperative Hb; however, there were differences when the Hb level dropped 50% from its baseline level.23
The risk of mortality in anemic patients decreases when adjusted for confounding variables such as age, peripheral vascular disease, renal failure and a history of myocardial infarction or chronic obstructive pulmonary disease (COPD).13 Even though it is not easy to control the bias associated with the indication in the studies that report an association between anemia and adverse events in patients who need to be transfused, it is important to highlight the number of studies in which transfusion is associated with adverse events, such as: pneumonia, mediastinitis, renal dysfunction, mortality and decreased survival.
Conflict of interestNo disclosures
Financing Source: the author's own resources