Laparoscopic surgery as a minimally invasive technique has shown considerable benefit in terms of patient outcomes. However, major complications have been described, including spontaneous pneumothorax, with a 0.4% incidence. An unusual crisis in laparoscopic surgery – spontaneous bilateral pneumothorax – and an updated literature review are discussed with a view to identify the factors related to its occurrence and the prevention and management measures involved.
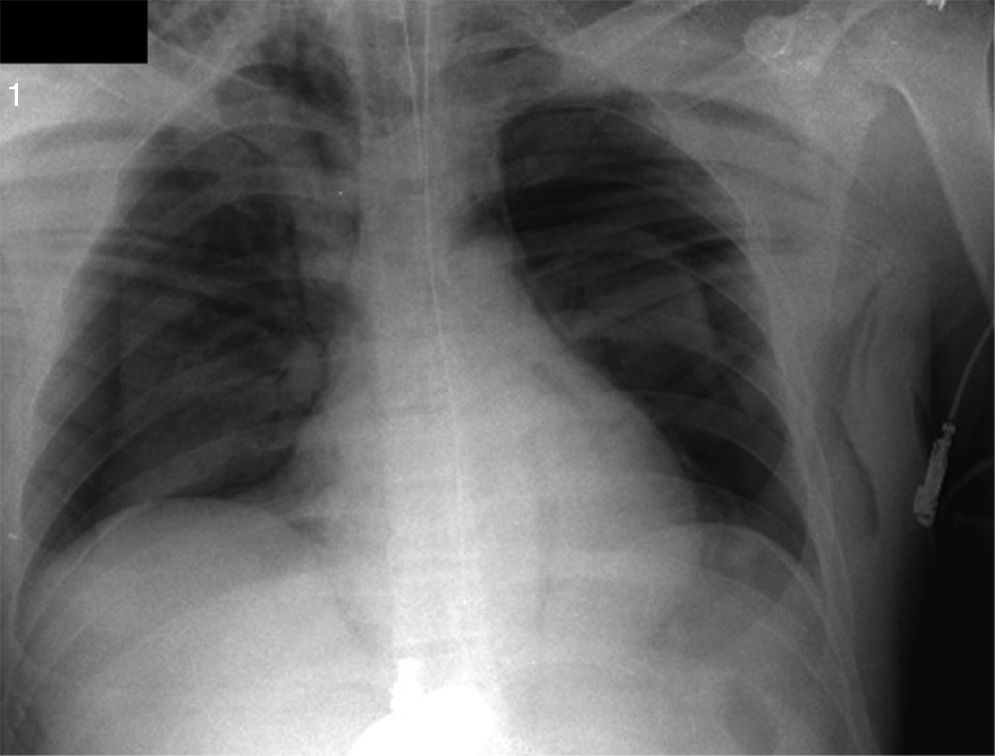
Case presentationA young man undergoing emergency laparoscopic surgery for abdominal pain. During the intraoperative period the patient developed respiratory impairment and subcutaneous emphysema. Bilateral pneumothorax was documented on chest X ray, though the etiology could not be established. Early diagnosis allowed for timely management with bilateral thoracotomy and extubation at the end of surgery.
ConclusionSpontaneous pneumothorax has been recognized as a potential crisis in laparoscopic procedures. There are multiple cases of this intraoperative complication reported in the literature since 1939. It is worth highlighting that to this date, and despite the advances in surgical techniques, monitoring and anesthetic agents, few elements may be manipulated and only an insightful anesthesiologist may prevent the condition from evolving into major hemodynamic and respiratory morbidity and even death. Few factors such as establishment of pneumoperitoneum and pressure, length of the procedure and type of surgery have been identified. Early diagnosis is based on a high suspicion due to subtle changes in respiratory and hemodynamic parameters that require radiographic confirmation if the patient's condition permits, followed by immediate decompression through thoracotomy.
la cirugía laparoscópica como técnica quirúrgica mínimamente invasiva ha demostrado importantes beneficios en el desenlace de los pacientes. Sin embargo, se han descrito complicaciones mayores como el neumotórax espontáneo, con una incidencia de 0,4%. Se presenta una crisis inusual en cirugía laparoscópica, como el neumotórax espontáneo bilateral y una revisión actualizada de la literatura que permita identificar los factores relacionados con su presentación y las medidas de prevención y manejo.
Presentación del casoun hombre joven llevado a cirugía laparoscópica de urgencia por dolor abdominal, en el periodo intraoperatorio presentó deterioro respiratorio y enfisema subcutáneo, documentándose un neumotórax bilateral en una radiografía de tórax, cuya etiología no fue posible establecer. Su rápido diagnóstico permitió el oportuno manejo con toracostomía bilateral y extubación al finalizar la cirugía.
Conclusiónel neumotórax espontáneo es reconocido como una potencial crisis en procedimientos laparoscópicos, y desde 1939 la literatura reporta múltiples casos de esta complicación intraoperaroria. Es de resaltar que al presente, a pesar de los avances en la técnica quirúrgica, monitoria y medicamentos anestésicos, pocos elementos pueden ser manipulados y solo la suspicacia del anestesiólogo puede prevenir su evolución a una mayor morbilidad hemodinámica y respiratoria o la muerte. Solo factores como la instauración y presión del neumoperitoneo, duración del procedimiento y tipo de cirugía han sido relacionados. Su rápido diagnóstico reposa en un alto índice de sospecha ante cambios sutiles en parámetros respiratorios y hemodinámicos que deben llevar a una confirmación radiográfica si el estado del paciente lo permite, con posterior descomprensión inmediata con toracostomía.
Abdominal laparoscopic surgery encompasses a broad range of procedures that have gained popularity because of the advantages in terms of patient recovery, low morbidity (1.07–0.3%) and low mortality rates (0.03%).1
Despite these encouraging statistics, there are however potential intraoperative complications not to be overlooked, such as cardiac arrhythmia, gas embolism, intestinal trauma, hemorrhage, pneumothorax, pneumomediastinum, and subcutaneous emphysema that may arise in this type of procedures.2 Other important complications affecting the cardiovascular system have been described, including advanced atrioventricular blocks. 3
Since 1939 pneumothorax has been reported as a laparoscopic complication with an incidence of 0.01–0.4%.4,5 Currently, despite the advances in the surgical technique, this complication is rather unusual, and even more so bilateral involvement.
The case presented is an unusual intraoperative crisis caused by bilateral spontaneous pneumothorax during a laparoscopic procedure in a young man. Though the outcome was not fatal, the situation was life-threatening for the patient and resulted in additional morbidity and a longer hospital stay. Spontaneous pneumothorax should be kept in mind as a potential crisis in laparoscopic surgery, with proper identification of risk factors, early suspicion and prompt diagnosis and management.
Case report36-year old man admitted to the emergency room with intense and poorly characterized, localized abdominal pain for the last 12h and nausea. The patient had a history of GI bleeding from peptic ulcer one year ago and high blood pressure managed with Losartan; previous knee arthroscopy and uncomplicated lumbar laminectomy, cigarette smoking and occasional alcohol use. The physical examination findings were hypertension (blood pressure of 130/100), heart rate (HR) 20bpm, oxygen saturation (SpO2) 97%, body temperature 37°C, normal cardiopulmonary auscultation, abdominal guarding, painful palpation of the right iliac fossa, positive Blumberg sign and positive Rowsing.
The paraclinical tests reported leukocytosis, normal platelet count and normal hemoglobin. The patient was diagnosed with appendicitis and laparoscopic appendectomy was indicated.
The pre-anesthesia evaluation indicated a functional class>4 METS, with no predictors of difficult airway.
A rapid induction sequence was used with lidocaine 60mg, propofol 150mg and succinylcholine 80mg followed by orotracheal intubation. 150mcg of fentanyl were then administered and 15min after the induction with rocuronium 20mg. Maintenance was provided with Sevofluorane 2V%, pressure control mechanical ventilation 15cmH2O, PEEP 5mmHg, RR 12×′, FiO2 0.7, tidal volume (Vt) 8ml/kg. Following the insufflation of the pneumoperitoneum with carbon dioxide (CO2) at a maximum pressure of 15mmHg, the inspiratory pressure was adjusted to 22cmH2O, maintaining Vt between 6 and 8ml/kg, RR 16×′, and the expired CO2 (ETCO2) was maintained between 30 and 35mmHg, documented via capnography. During the surgical procedure the appendix looked healthy but a systematic abdominal examination identified turbid fluid in the peritoneal cavity, multiple gallbladder membranes and a perforated duodenal ulcer. Multimodal analgesia was administered using dipyrone 2.5g and morphine 4mg. One hour into the anesthesia a progressive elevation of ETco2a 49mmHg was identified, decreased tidal volumes and declining SaO2 to 89%. The hemodynamic condition was not impaired. The physical examination revealed subcutaneous emphysema in the neck and bilateral hypoventilation that led to the interruption of the laparoscopic procedure and a chest X-ray that showed spontaneous bilateral pneumothorax of approximately 40% (Fig. 1). A bilateral thoracotomy was performed followed by complete SaO2 recovery and improved tidal volume. The procedure was then completed through an open approach, with laparotomy, duodenal suture and duodenal ulcer repair using a Graham patch.
At the end of the procedure the patient was extubated free of complications and was transferred awake to the ICU where he received medical management and respiratory therapy, and 24h later was transferred to the in-patient floor. The patient continued to evolve with no respiratory or hemodynamic impairment and was discharged after five days.
DiscussionAlthough the pneumothorax may have various etiologies, the pathophysiology involves increased intrapleural pressures versus the atmospheric pressure, resulting in pulmonary collapse with oxygenation and ventilation impairment and cardiovascular involvement due to a disruption in ventricular filling and cardiac output. Spontaneous pneumothorax in laparoscopic surgery is an unusual complication described in about 0.4% of the cases. Its diagnosis is based on the identification of the pathophysiological events described above that may be masked due to the effects of anesthesia. Some events, including increased airway pressure, a drop in SaO2, and changes in the ETco2, may be some of the early and subtle changes during the course of the crisis. Hemodynamic changes may be delayed and are related to the severity of the pneumothorax. In our patient, the gradual changes in ventilation parameters triggered a comprehensive examination that revealed subcutaneous emphysema in the neck and pulmonary hypoventilation leading to the suspicion of an intraoperative crisis such as spontaneous pneumothorax. A high rate of suspicion is the key factor in the diagnosis of this condition, since the clinical manifestations may be misinterpreted for more frequent intraoperative conditions such as selective intubation, airway obstruction, low inspired oxygen fraction, inadequate plane of anesthesia, drug-mediated vasodilatation, etc. Moreover, there are some cases described in the literature of pneumothorax-induced complete lung collapse, unrelated to increased airway pressure, ETco2 variations or desaturation.4 The broad range of presentations relates with the patient's cardiovascular condition, and with how fast and how severe the pneumothorax establishes.
It has been known that any procedure performed in the region of the diaphragm such as fundoplication, adrenalectomy, etc., involve a high risk of pneumothorax due to an accidental structural injury.5,2,6,7 Other mechanisms that cause pneumothorax are not related to any iatrogenic injury of the diaphragm and raise the level of difficulty to prevent such crisis. The migration of the pneumoperitoneum gas into the chest cavity through other routes such as a congenital diaphragmatic defect, i.e. foramen of Morgani or Bochdalek,8,9 the esophageal and aortic hiatus or through any other procedure with the potential to injure the falciform ligament, are some of the other theories suggested. The insufflated CO2 may also dissect the retroperitoneum, become disseminated and reach the structures of the neck as was the case with this patient. It may also reach the pleura.
The perforation of the duodenum has also been associated in the literature with unilateral or bilateral pneumoperitoneum because this condition usually presents in the retroperitoneum and associated with certain procedures such as ERCP – endoscopic retrograde cholangiopancreatography. The finding of a duodenal perforation in our patient could be the reason for the pneumothorax. Some reports describe the development of subcutaneous emphysema following a laparoscopic extraperitoneal inguinal hernia repair and its extension into the thoracic cavity or the mediastinum, causing a pneumothorax or a pneumomediastinum.10,11 Consequently, the presence of subcutaneous emphysema in laparoscopic surgery should lead to suspect a spontaneous pneumothorax, even in the absence of clinical signs. In the case under discussion, the subcutaneous emphysema accompanied by signs of respiratory decompensation raised the suspicion of spontaneous pneumothorax that resulted in the interruption of the procedure and the pneumoperitoneum and the indication for a X-ray that confirmed the diagnosis of the spontaneous bilateral pneumothorax (Fig. 1).
Other risk factors have been described for the development of pneumothorax in laparoscopic surgery, such as extended surgical times (usually beyond 200min), ETco2 of 50mmHg, old age and inexperienced surgeon.12,13 Other options have been suggested including gasless laparoscopy in which the peritoneal cavity expands using an abdominal retractor that prevents hemodynamic and respiratory changes with increased intra-abdominal pressure and all the consequences of using intra peritoneal CO2.14–16 However, there is no evidence of any impact that the manipulation of these factors may have on the occurrence of this complication. The patient did not exhibit any risk factors that could alert about the potential development of spontaneous pneumothorax. It was only the clinical signs during the intraoperative period that raised the suspicion of the crisis.
The spontaneous bilateral pneumothorax that our patient presented was not accompanied by hemodynamic instability so that there was the opportunity to make a radiological diagnosis and further treatment with bilateral thoracotomy. However, when hemodynamic stability occurs during the intraoperative crisis, management with tension pneumothorax should not be delayed waiting for a radiographic confirmation. These situations require either immediate decompression using an angiocatheter inserted at the second intercostal space of the hemithorax involved or emergency thoracotomy. Rapid diagnosis and management of this patient's complication prevented the occurrence of a fatal outcome, but the conversion to open surgery resulted in increased morbidity and extended hospital stay.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
FundingNone.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Mendoza KC, Suarez GC, Suguimoto A. Crisis anestésica en cirugía laparoscópica: neumotórax espontáneo bilateral. Diagnóstico y manejo, reporte de caso. Rev Colomb Anestesiol. 2015;43:163–166.