Nasotracheal intubation is usually the selected airway approach for oral and maxillofacial surgery to enable a free surgical field. It is an unusual intubation technique with a high success rate. However, it is not free from difficulties and complications in certain groups of patients, like those with oral, facial or cervical tumors.
The Airtraq® laryngoscope (Prodol Meditec, Vizcaya, Spain) is an optical device that facilitates tracheal intubation through the indirect visualization of the vocal cords, avoiding the need to align the oral, pharyngeal and laryngeal axis. It has shown to be useful in various difficult airway (DA) scenarios. There is a version of the device to assist with the nasal intubation technique.
Two oral brachytherapy treatment cases classified as DA are discussed; the nasotracheal intubation of the patient awake was successful using the Airtraq optical laryngoscope.
La intubación nasotraqueal suele ser el abordaje electivo de la vía aérea en cirugías orales y maxilofaciales, permitiendo así un campo quirúrgico libre. Se trata de una técnica de intubación poco habitual con alto índice de éxito. Sin embargo, no está exenta de dificultades y complicaciones en ciertos grupos de pacientes como aquellos con tumoraciones orales, faciales o cervicales.
El laringoscopio Airtraq® (Prodol Meditec, Vizcaya, España) es un dispositivo óptico que facilita la intubación traqueal mediante la visualización indirecta de las cuerdas vocales, sin necesidad de conseguir la alineación de los ejes oral, faríngeo y laríngeo. Ha demostrado su utilidad en diferentes escenarios de vía aérea difícil (VAD). Existe una versión del mismo diseñada para asistir en la técnica de intubación nasal.
Presentamos dos casos de tratamiento con braquiterapia oral, catalogados de VAD, cuya intubación nasotraqueal en paciente despierto fue realizada de forma exitosa mediante el laringoscopio óptico Airtraq.
The treatment of oral malignancies comprises various treatment approaches. Brachytherapy techniques using localized radiation with high dose regimes have been developed, achieving excellent local remission rates, minimizing the adverse effects resulting from a more extensive treatment.
Nasal intubation is usually the method of choice for managing the airway in oral and maxillofacial surgeries. It is a less frequent intubation technique with high success rates that is not exempt from difficulties and complications in certain groups of patients, such as those with oral, maxillofacial or cervical cancer, or in patients previously subject to radiation therapy in those areas.
The new optical devices for managing the airway progressively expand their indications to different difficult airway (DA) scenarios, both for expected as well as for unexpected difficult airway. However, these devices are rarely used for nasal intubation.
CasesCase 170-year-old male, drinks over 100g of alcohol per day, diagnosed with tongue neoplastic relapse. The patient was operated on 4 years ago with a diagnosis of squamous cell carcinoma of the tongue (left hemiglossectomy) with no adjuvant therapy. The patient had a relapse that affected the rest of the tongue with involvement of the floor of the mouth and was treated with external radiotherapy followed by interstitial brachytherapy with a 16Gy regime in 4 sessions.
Airway exploration: Mallampati III, 3cm mouth opening, obesity (BMI: 33kg/m2), snores, thyromental distance (TMD)>6cm, sternomental distance (SMD)>12cm, upper lip bite test (ULBT) III, radiated neck; cricothyroid membrane difficult to palpate.
The decision was made to proceed with nasotracheal intubation with the patient awake, using the Airtraq laryngoscope. If this failed, the alternate plan was to intubate with aScope-2 videoscope (Ambu A/S, Ballerup, Denmark) with the patient awake and using a nasal approach. The upper airway anesthesia was administered by placing cotton wicks soaked with 1% tetracaine with 3cc vasoconstrictor (adrenaline 1:10,000) on both nostrils, 2% lidocaine spray on the base of the tongue (up to 5cc) using the MADgic (LMA Inc, San Diego, CA, USA) spray and nebulized 4% lidocaine. The patient was sedated with intravenous midazolam (2mg) and continuous perfusion of remifentanil (0.1μgKg−1min−1).
Upon verification of good tolerance of the oral introduction of Airtraq, a 6.5mm internal diameter (ID) preformed nasal tube was inserted through the right nostril (Portex-Smiths Medical, St. Paul, MN, USA) that was advanced until visualization by the optical device. The tube was uneventfully guided to the glottic region. Once the tube passed beyond the lumen of the trachea the patient experienced a strong coughing episode that hindered the Airtraq vision but the endotracheal tube (ETT) was kept in place. Proper end-tidal CO2 outflow was verified and general anesthesia was induced.
Case 269-year-old male, smokes 30 cigarettes per day, with squamous cell carcinoma relapse of the floor of the mouth. The patient had been treated 27 years back with chemotherapy resulting in complete remission. Following this relapse, the patient was operated on (resection of the lesion on the floor of mouth+left supraomohyoid lymph node removal) followed by adjuvant external radiotherapy. The patient was then programed to complete treatment with high dose brachytherapy (6 3Gy sessions).
The results of the airway exploration were: Mallampati III, TMD>6cm, SMD>12cm, ULBT III, mouth opening 3cm and proper cervical extension. Radiated neck with surgical scar in the cervical and left mental region. The cricothyroid membrane is identified using palpation.
Because of the patient's history and the surgical requirements, the decision was made to intubate the patient awake through a nasal approach. The patient was sedated following the same regime as in the previous case. Upon preparing both nostrils with a mixture of local anesthetic and vasoconstrictor, and anesthetizing the base of the tongue, the oropharynx and the hypopharinx, a disposable Fastrack ETT (LMA Inc., San Diego, CA, USA) was introduced through the right nostril. The ETT was guided uneventfully introducing an Airtraq optical laryngoscope by mouth for nasal intubation until it was placed in front of the interarytenoid notch. Using the MADgic laryngeal sprayer, and under the vision provided by Airtraq, a final instillation of local anesthetic was administered (2cc of 2% lidocaine) at the level of the vocal cords and the glottic introitus. After 2min, the ETT was smoothly advanced to its intratracheal position, with excellent patient tolerance.
DiscussionThe difficult airway concept includes difficulty during laryngoscopy, during intubation and difficult manual ventilation.1 The incidence of failed intubation, i.e., failure to place a ETT is 0.05% among the general population, between 0.15 and 0.3% in the obstetric population and may be up to 20% in patients with maxillofacial and ENT tumors.
The treatment of oral and maxillofacial malignancies requires a multimodal approach. Early stage oral carcinomas (T1 and T2), usually exhibit an excellent response in terms of local control of the disease following surgery or high dose interstitial brachytherapy. Brachytherapy is a high dose local radiation regime administered over a few sessions. The key advantage is the absence or lower intensity of adverse events. If after surgery the patient continues to present positive margins, external radiotherapy of the affected area shall follow, with the resulting side effects (xerostomia, mucositis, dysphagia, necrosis, fibrosis, etc.).2 When local relapses develop, such as the patients discussed, brachytherapy is listed as a final supplementary treatment to external radiotherapy.
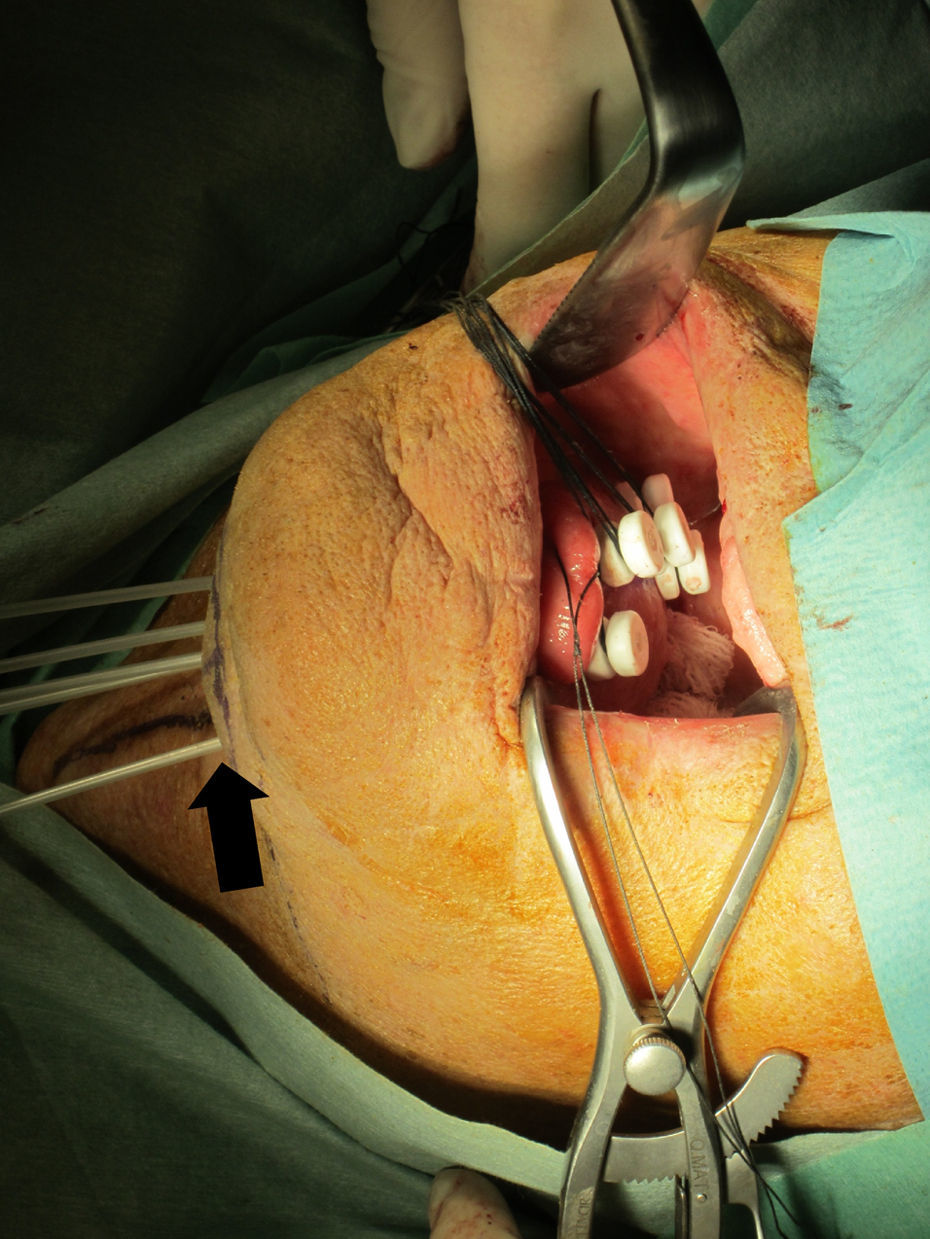
These oral brachytherapy techniques require placing some needles across the affected area to connect then to the radiation source using external probes (Fig. 1). Evidently, these procedures require general anesthesia with endotracheal intubation to facilitate the job of cancer radiotherapists and maxillofacial surgeons.
Usually, nasal intubation is done through direct laryngoscopy with the conventional Macintosh laryngoscope and using the Magill forceps to guide the preformed nasal tube onto the trachea.3 When dealing with a known difficult airway that requires a nasal approach, the gold standard for endotracheal intubation is still the flexible fiberscope with the patient awake. Several optical devices that have shown excellent results in nasal intubation of patients with no difficult airway predictors,4,5 have also proven to be a valid alternative to the fiberscope in difficult airway cases.3,6,7 The successful resolution of these situations with such devices, their portability and ease-of-use, lower costs and easy to learn have gradually replaced the flexible fiberscope when it is not available or when the fiberscope technique is not mastered. Endotracheal intubation using optical devices with the patient awake is currently widely used; the requirements for using such intubation technique are a proper local upper airway anesthesia, mild sedation and adequate mouth opening to introduce the device (18mm for the Airtraq).
Both techniques, the fiberoptic assisted and videolaryngoscope intubation are not mutually exclusive; the knowledge of both devices may allow for their simultaneous and combined use for intubation in complex scenarios, even when the patient is awake. There are papers describing the use of the Airtraq optical laryngoscope to provide adequate vision for anesthetizing the airway using the spray-as-you-go technique, and to facilitate intubation with the flexible fiberscope following failed intubation attempts.8,9
This evidences a change in the anesthesiologist approach to the difficult airway, and greater confidence in the use of safer and widely accessible new tools. Numerous scientific societies are gradually accepting and introducing optical devices to their difficult airway management algorithms.1
The Airtraq laryngoscope is an optical rigid and disposable device using a set of lenses and mirrors to facilitate the indirect visualization of the glottis. It has proven to be useful under various difficult airway scenarios, both in awake and anesthetized patients, regardless of whether it is used by experts in airway management, by inexperienced staff or paramedics.10 There is a slightly modified version of the Airtraq to facilitate the nasotracheal intubation technique; the absence of a lateral canal and the anatomic design of the blade allow for guiding the ETT toward the glottis and enable the oral introduction of any accessory elements if needed.11 As compared to the classical technique using the Macintosh laryngoscope for nasal intubation, the Airtraq provides more favorable intubation conditions, is less time consuming, fewer attempts are needed, resulting in minimal hemodynamic changes during the procedure, optimal visualization of the glottis, less maneuvers for external assistance and limited use of the Magill forceps to guide the ETT.5,12
In our first case we decided to use the Airtraq device for intubating the patient because the flexible fiberscope was unavailable, and because the patient had an inter-incisor distance that allowed for its introduction. The oral insertion was well tolerated and had an acceptable vision; however, since the tracheal mucosa had not been anesthetized, the stimulus of the ETT caused considerable coughing.
There have been some cases reported of intubation in awake patients only receiving local anesthetic with sprayed particles; the local anesthetic deposited over the tracheal mucosa is usually minimal because it decreases as the distance increases and may not be effective enough for the patient to tolerate the maneuver or to attenuate the resulting hemodynamic response. This problem was solved in the second case by pulverizing the anesthetic agent at the entrance of the trachea facilitated through the Airtraq vision, avoiding the discomfort of transtracheal topical anesthesia.13
Similarly, in the first case we chose a preformed nasal ETT, following the routine of the standard nasal intubation, and we overlooked the intubation failures with such ETT or other complications (keep in mind that the introduction of the flexible fiberscope through a preformed nasal ETT is usually extremely difficult). In the second case – having the flexible fiberscope available as rescue tool – we chose a Fastrach reinforced ETT considering the possibility of introducing the fiberscope if the Airtraq technique failed.
ConclusionIn our opinion the Airtraq optical laryngoscope is a useful and safe alternative versus direct laryngoscopy and the flexible laryngoscope for nasotracheal intubation in patients with identified difficult airways, and specifically, for surgical procedures involving oral brachytherapy.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
FundingThe authors have not received any funding for producing this article.
Conflicts of interestNone.
Please cite this article as: Pascual MC, Ramírez ET, Ares AB, García JPJ, Gastón MB, Basarte EH. Intubación nasotraqueal con laringoscopio óptico airtraq en dos casos de braquiterapia oral. Rev Colomb Anestesiol. 2015;43:167–170.