The presence of truncus arteriosus represents just 1.2–3% of all complex congenital heart pathologies and if not corrected, less than 20% survive beyond one year of life. When the disease progresses patients usually develop severe pulmonary hypertension and may even develop into Eisenmenger's syndrome. The paper discusses a case of a schoolboy with a diagnosis of uncorrected truncus arteriosus type I, and severe pulmonary arterial hypertension undergoing non-cardiac surgery.
Case discussionThis is a 9-year old schoolboy with complex heart disease and similar pulmonary and systemic blood pressures, undergoing elective orthopedic surgery under regional anesthesia, with lumbar plexus block and posterior sciatic block. This anesthetic approach provided adequate anesthesia with hemodynamic stability and no impact on vascular resistance.
ConclusionThe choice of the anesthetic technique should be a planned decision based on the cardiovascular pathophysiology of the truncus arteriosus, the level of pulmonary hypertension, and the surgical procedure to be performed. Patients with severe pulmonary hypertension are at increased risk of developing suprasystemic pulmonary pressures with considerable hemodynamic involvement. Consequently, the anesthetic technique chosen shall provide adequate anesthesia and ensure the least hemodynamic impact. Whenever possible, it is important to consider the peripheral nerve block as the first line approach for orthopedic surgery.
La presencia de tronco arterioso representa únicamente del 1.2 al 3% de las cardiopatías congénitas complejas y de no ser corregida, menos del 20% sobreviven después del año de vida. Si la patología progresa usualmente desarrollan hipertensión arterial pulmonar severa y pueden manifestarse incluso como un Síndrome de Eisenmenger. Se presenta un caso de un escolar con diagnóstico de tronco arterioso tipo I no corregido e hipertensión arterial pulmonar severa llevado a cirugía no cardiaca.
Presentación del casoEscolar de 9 años de edad con cardiopatía compleja y presión arterial pulmonar similar a la presión arterial sistémica sometido a cirugía ortopédica electiva bajo anestesia regional con bloqueo de plexo lumbar y bloqueo ciático posterior. Esta técnica anestésica nos proporcionó una adecuada anestesia con estabilidad hemodinámica sin repercusión en las resistencias vasculares.
ConclusiónLa elección de la técnica anestésica debe ser planeada en base a la fisiopatología cardiovascular del tronco arterioso, del grado de hipertensión pulmonar y del procedimiento quirúrgico a realizarse. Los pacientes con hipertensión pulmonar severa tienen mayor riesgo de manifestar presiones pulmonares suprasistémicas con compromiso hemodinámico importante, por lo que la técnica anestésica elegida será aquella que produzca una adecuada anestesia y menor repercusión hemodinámica. Es importante considerar de ser posible, el bloqueo de nervios periféricos como primera elección en cirugía ortopédica.
Congenital heart disease continues to be one of the primary anomalies at birth. About 30% of these patients may require some type of non-cardiac surgery during their first year of life and it is estimated that up to 80% grow up to become adults in the United States.1 Unfortunately in our environment there is a large number of children with congenital heart disease. Late diagnosis and lack of treatment result in severe complications that significantly increase perioperative morbidity and mortality.
Truncus arteriosus represents only 1.2–3% of the complex congenital heart diseases. If uncorrected, less than 20% of these patients will survive their first year of life.2 The development of pulmonary hypertension is a serious complication of this type of condition and is characterized by a mean pulmonary artery pressure above 25mmHg at rest and above 30mmHg during exercise.3 Our objective is to discuss a case report of a schoolboy diagnosed with uncorrected truncus arteriosus and severe pulmonary hypertension undergoing an elective orthopedic procedure.
Case presentation9-year old male patient with a diagnosis of uncorrected truncus arteriosus type I, and severe pulmonary hypertension that presents with severe right knee pain and gate limitation. The MRI shows intact cruciate ligaments and discoid lateral meniscus. The patient was evaluated at the service of Pediatric Orthopedics and diagnosed with congenital right knee dislocation and was programmed for surgical repair.
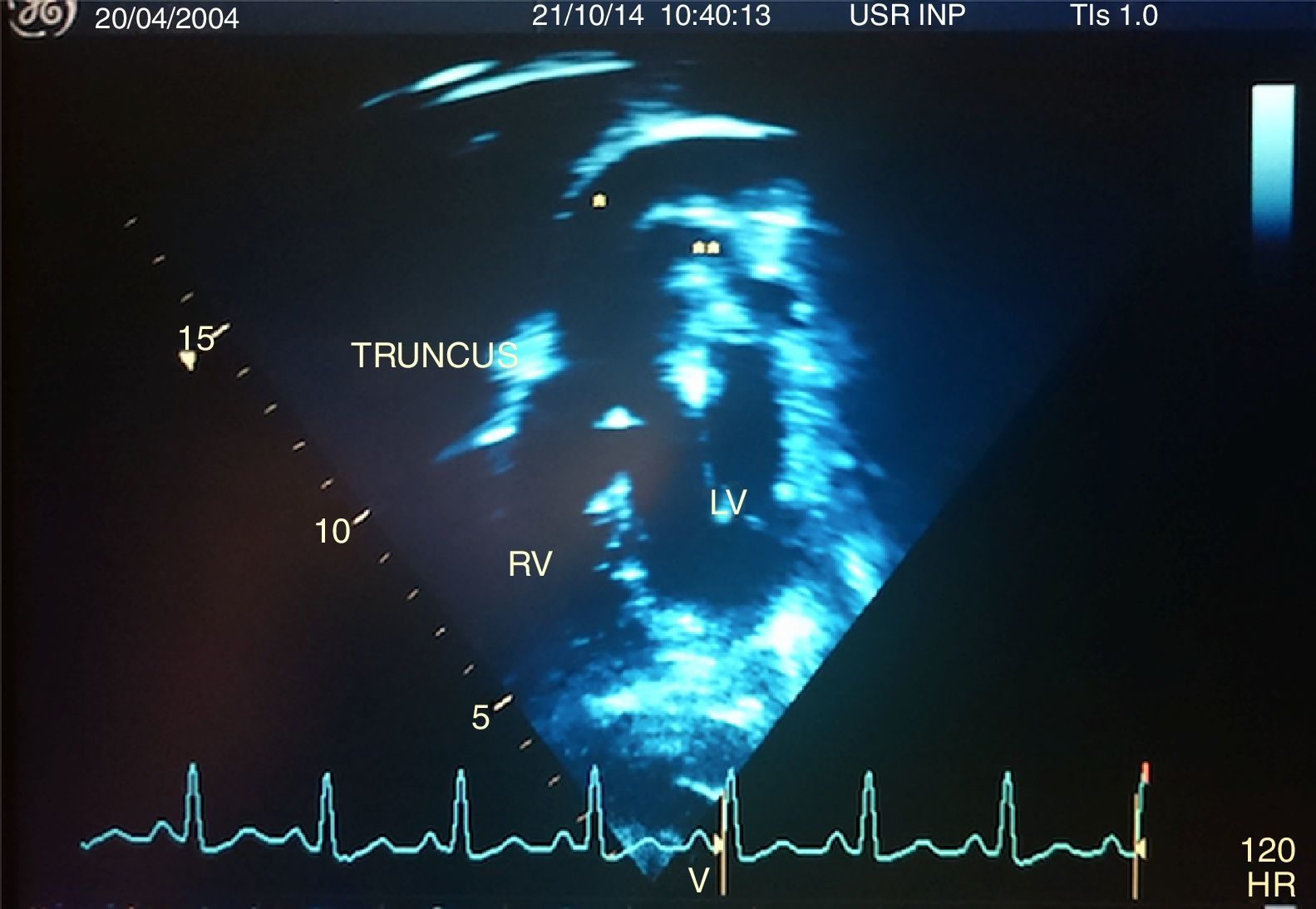
The pre-anesthesia evaluation reported uneventful family history with a diagnosis of velocardiofacial syndrome and mild psychomotor retardation. The findings of the physical evaluation indicated a cooperative patient, functional class NYHA II, generalized cyanosis, precordial fremitus, multifocal systolic murmur, pulse oximetry 87%, and body weight of 22kg. The transthoracic echocardiographic examination confirmed the cardiology diagnosis (Image 1). The patient has a history of anesthetic sedation for cardiac catheterization showing that the pulmonary pressure equaled the systemic blood pressure.
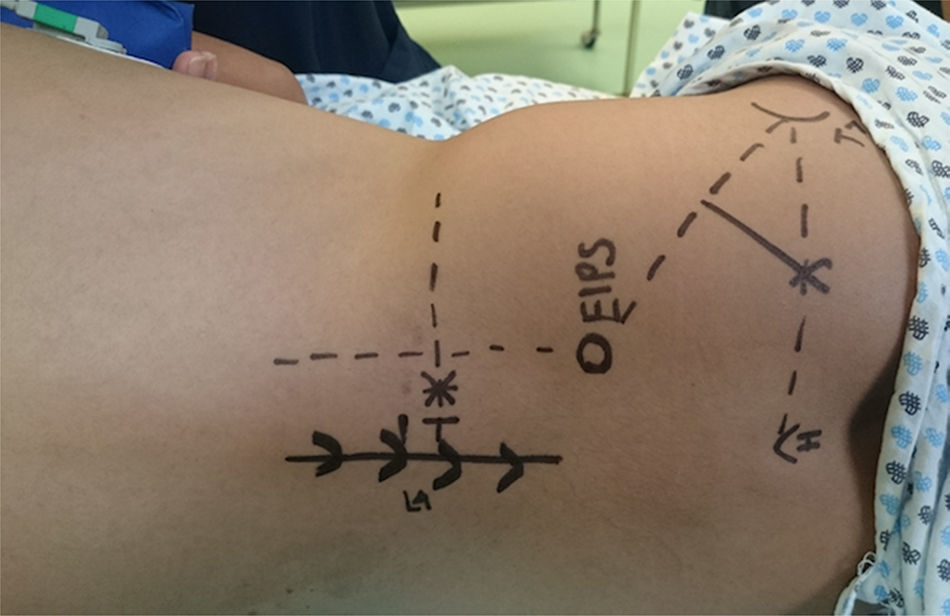
The orthopedic surgery was done under regional anesthesia. The patient was admitted to the OR with a patent 20G peripheral catheter. The initial monitoring indicated a BP of 99/62mmHg, HR 113lpm, room air SpO2 88%, Temperature 36.8°C. Intravenous sedation with fentanyl 50mcg, lidocaine 20mg, propofol 45mg and invasive monitoring with right radial arterial line was later on performed. During the procedure the patient maintained spontaneous ventilation and received supplemental oxygen through a nasal cannula. A propofol infusion between 90 and 120mcg/kg/min was used for maintenance of anesthesia. Regional anesthesia was delivered through a posterior sciatic block and lumbar plexus block using neurostimulator guidance with Ropivacaine and Lidocaine with no complications (Image 2).
The hemodynamic parameters were stable during the procedure with arterial blood pressure measurements between 68 and 80mmHg, HR 96–105lpm, SpO2 82–90%. Bleeding was minimal. At the end of the procedure the patient was admitted to the pediatric ICU with Aldrete score of 9, 2 in Ramsay's scale, 3 in Bromage's scale, 0 pain in the visual analog scale.
DiscussionThe truncus arteriosus is characterized by the presence of a single arterial vessel emerging from the base of the heart and irrigates the coronary bed, the pulmonary circulation, the systemic circulation, and usually presents interventricular communication. From the embryological perspective this defect is the result of a failed division of the common truncus between the pulmonary artery and the aorta. A deletion of the 22q11 chromosome has been identified in up to 35% of the patients.7
Collett and Edwards described 4 types of truncus arteriosus, based on the origin of the pulmonary artery. Type I (48–68%) is defined as the presence of a small pulmonary trunk arising from the arterial trunk with branching of the right and left pulmonary branches. In type II (29–48%), the trunk of the pulmonary artery is missing but the pulmonary branches emerge close to one another from the arterial trunk. Type III (6–10%) is also characterized by the absence of the trunk of the pulmonary artery but the right and left branches emerge distant from one another. Type IV is no longer considered an anomaly of the truncus arteriosus and is now recognized as a form of pulmonary atresia with ventricular septal defect.8
As a result of the changes in cardiopulmonary circulation, patients with truncus arteriosus present with a left to right shunt that increases the pulmonary blood flow.9 The pulmonary blood vessels chronically exposed to an increased blood flow, develop an obstructive vascular pathology leading to increased pulmonary vascular resistance and hence increased pulmonary pressure. When this pressure equals or exceeds the systemic blood pressure, there will be reversal of the shunt and causes severe hypoxia.10 Patients with uncorrected congenital heart disease and left to right shunt will develop Eisenmenger's disease or Eisenmenger's complex characterized by pulmonary hypertension, right ventricular atrophy, impaired pulmonary vessels, reversal of right to left shunt, and hypoxemia refractory to oxygen therapy.2 When the pulmonary vascular resistance exceeds 8 Wood units, or if Eisenmenger's syndrome has been diagnosed, corrective surgery is contraindicated.11 Eventually patients usually die from heart failure.12
Carmosino et al. showed that children with pulmonary hypertension have a significantly higher risk of developing perioperative complications, including cardiac arrest, pulmonary hypertension crisis, and death when undergoing procedures under sedation or under general anesthesia. Most complications were more frequent in those patients with pulmonary pressure equal or higher than the systemic blood pressure, and there was no association either with age or etiology.3 Unless a previous genetic study is available, any blood products that need to be administered to patients with truncus arteriosus shall undergo prior radiation, because of the strong association with Di George syndrome and T-lymphocytes deficiency.7
The anesthetic considerations include a broad range of variables to be considered. The presence and the severity of cardiac failure may require preoperative management with inotropic agents. The principal goal during the induction of anesthesia will be maintaining a balance between the pulmonary vascular resistance (PVR) and the systemic vascular resistance (SVR). Hyperventilation or using high oxygen concentrations leads to a reduced PVR, contributing to a considerable increase of the pulmonary blood flow, lower diastolic blood pressure, and even results in systemic hypoperfusion.7
There is no consensus about the safest anesthesia in patients with severe pulmonary hypertension or in patients with Eisenmenger's syndrome. In a literature review, Martin et al. claim that using regional anesthesia has no advantage over the use of general anesthesia. However, the best predictor of mortality is the type of surgical intervention, since patients undergoing major surgery experienced up to 24% mortality as compared to 5% in patients undergoing minor surgery.13
The anesthetic management of this patient was planned based on the cardiovascular pathophysiology of the truncus arteriosus with severe pulmonary hypertension. The pulmonary and systemic blood flows arise from a common vessel and consequently the blood flow circulation and distribution may be affected when manipulating the vascular resistance. The patient's pulmonary pressure was similar to the systemic blood pressure, so our priority was to avoid any changes in the pulmonary and systemic vascular resistance since such changes could favor the imbalance between both types of circulation. We decided to keep the patient under spontaneous ventilation since endotracheal intubation and the use of mechanical ventilation could increase the PVR. CO2 was monitored via an arterial line and was kept between 38 and 43mmHg, since both hypocapnia and hypercapnia change the pulmonary vessels resistance. FiO2 was maintained between 21 and 25% in order to avoid a drop in PVR. We used propofol to maintain sedation because its pharmacological characteristics make it predictable; at the usual doses propofol has no negative inotropic effect and has a short half-life.
One of the major challenges during the procedure was to select an anesthetic technique that provided stronger hemodynamic stability. We decided to use a lumbar plexus block, in addition to the posterior sciatic nerve block and this provided adequate anesthesia with no impact on systemic vascular resistance.
In conclusion, the management of anesthesia in patients with congenital heart disease must be individualized and should take into account the complexity of the non-cardiac surgical procedure, the level of cardiovascular involvement resulting from the congenital heart disease, and the hemodynamic impact on the various organs. When there is uncorrected truncus arteriosus, the primary goal of anesthesia shall be to maintain a balance between the pulmonary vascular resistance and the systemic vascular resistance, and consider regional anesthesia with peripheral nerve block as an alternative for managing these patients. Moreover, these procedures should be done by a multidisciplinary team with experience in these conditions and at a hospital with the adequate technology available for diagnosis and perioperative management.
Ethical disclosureProtection of persons and animalsThe authors declare that this research did not involve any experiments in human beings or animals.
Confidentiality of dataThe authors affirm that they have followed the protocols of their institution on the publication of patient information.
Right to privacy and informed consentThe authors obtained the informed consent of all patients and/or subjects herein mentioned. These documents are under custody of the corresponding author.
FundingAuthors’ personal funds.
Conflicts of interestNo conflicts of interest to disclose. This article was written by the authors and is proprietary.
Please cite this article as: Díaz-Fosado LA, Sarmiento L, Velazquez-Martínez T. Manejo anestésico de un escolar con tronco arterioso tipo I no corregido e hipertensión pulmonar severa sometido a reparación de luxación congénita de rodilla. Reporte de caso. Rev Colomb Anestesiol. 2016;44:259–262.