Knee osteoarthritis is a common cause for consultation around the world. Many patients with mild symptoms respond to conservative treatment, while others require interventional therapy including peripheral nerve blocks.
ObjectiveTo establish the clinical efficacy and safety of interventional management with ultrasound-guided saphenous nerve block in patients with chronic keen pain.
Materials and methodsDescriptive, retrospective trial in chronic keen pain patients who underwent ultrasound-guided interventional therapy at the pain clinic in the country, between September 2011 and June 2012, to determine the clinical efficacy and safety of the procedure. Data were obtained from all patients prior to the procedure, and then at two days, one month and three months later. The pain intensity was measured using the visual analog scale.
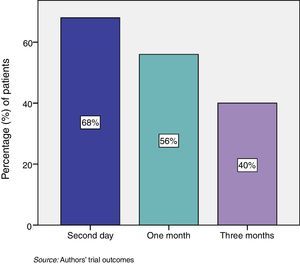
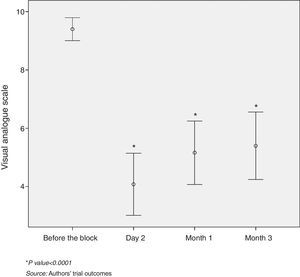
Results25 saphenous nerve blocks were performed. 68% of the patients experienced pain relief within two days. 56% and 40% exhibited relief one and three months after the procedure, respectively, with a statistically significant difference (p<0.0001) between the baseline visual analog scale and the follow-up evaluation. Patients with a history of fibromyalgia, neuropathic characteristics and previous knee surgery exhibited variable analgesic responses to the procedure.
ConclusionsInterventionist chronic knee pain management with ultrasound-guided saphenous nerve block was an effective and safe approach for these patients.
La osteoartritis de rodilla es una causa común de consulta en el mundo. Muchos pacientes con síntomas leves responden a los tratamientos conservadores, y otros requieren de tratamiento intervencionista, como bloqueos de nervios periféricos.
ObjetivoDeterminar la eficacia clínica y la seguridad del manejo intervencionista con bloqueo del nervio safeno guiado por ultrasonografía en pacientes con dolor crónico de rodilla.
Materiales y métodosEstudio de tipo descriptivo retrospectivo en pacientes con enfermedad dolorosa crónica de rodilla que recibieron tratamiento intervencionista guiado por ultrasonografía en una clínica de dolor del país entre los meses de septiembre de 2011 y junio de 2012, para determinar su eficacia clínica y su seguridad. Se obtuvieron datos de todos los pacientes antes del procedimiento, a los 2 días, un mes y 3 meses después. La intensidad de dolor se midió con la escala visual analógica.
ResultadosSe realizaron 25 bloqueos del nervio safeno. El 68% de los pacientes presentaron alivio del dolor a los 2 días. El 56 y el 40% presentaron alivio al mes y a los 3 meses de realizado el procedimiento, respectivamente, con una diferencia estadísticamente significativa (p<0,0001) entre las medianas de la escala visual analógica inicial y la escala visual analógica de los seguimientos. No se presentaron complicaciones. Los pacientes con antecedente de fibromialgia, dolor de características neuropáticas y cirugía previa de rodilla presentaron respuestas analgésicas variables con el bloqueo.
ConclusionesEl manejo intervencionista del dolor crónico de rodilla con el bloqueo del nervio safeno guiado por ultrasonografía de los pacientes observados fue una opción de tratamiento eficaz y segura.
Knee osteoarthritis (OA) is an important public health condition worldwide. Symptoms are present in 20–30% of the population over 65 years of age with an increasing prevalence due to our aging population. The condition is characterized by chronic joint pain that impacts the quality of life.1–3 The diagnosis is based on X-ray findings, although 50% of the patients with radiological changes do not present clinical symptoms.3
Most patients with mild knee OA symptoms respond to conservative treatment such as physical therapy, anti-inflammatory agents, and hyaluronic acid injections, among others. However, these therapies are not enough for patients with severe symptoms. Total knee arthroplasty is the only valid and reliable treatment to relieve refractory joint pain of the osteoarthritic knee, but there are some patients with high surgical risks and others who are not willing to undergo surgery.1 Therefore, other minimally invasive therapeutic options have been included, such as ultrasound-guided saphenous nerve block, also used for other indications such as arthroscopy analgesia, ankle and varicose veins surgery, for the treatment of saphenous nerve chronic neuralgia, and verve entrapment at the adductors canal.4
Ultrasound guidance has improved the safety of these techniques since it lends itself to using a smaller volume of local anesthetic agent and thus avoids systemic toxicity, shortens the time required for the block, requires less needle insertions and provides faster onset of action. Moreover, this approach reduces the risk of accidentally puncturing other structures since it enables the visualization of the peripheral nerves, of the neighboring structures and of the needle. There are few disadvantages including limited availability and the need for an additional training.5–9
Due to the little information available about the efficacy of the saphenous nerve block in chronic knee pain, the purpose of this article was to determine the efficacy of the saphenous nerve block in chronic knee pain.
Materials and methodsWith prior authorization from the Ethics Committee, an observational, descriptive, longitudinal, and retrospective study was undertaken in patients with chronic knee pain disease who received ultrasound-guided intervention treatment with a sub-sartorial approach for a saphenous nerve block. Records were obtained prior to the procedure, and then two days, one month and three months following the block. The sample was taken from patients who came to the pain clinic for consultation between September 2011 and June 2012 and who met the inclusion and exclusion criteria. The data were collected from secondary sources (medical records). Since this was an observational study, no informed consents were required.
The inclusion criteria were as follows: (1) chronic knee pain diagnosis (more than 6 months), (2) administration of a saphenous nerve block, and (3) the use of ultrasound to guide the block.
The exclusion criteria were: (1) indication for interventional management with multiple simultaneous blocks, (2) knee prolotherapy-based pain management or saphenous nerve radiofrequency in the course of the last year, and (3) insertion of a continuous perineural infusion catheter.
The variables considered included: sex, age, diagnosis, use of concomitant oral pain killers, diagnosis of fibromyalgia, prior ipsilateral knee surgery, presence of neuropathic-like pain, pain classification according to the visual analog scale (VAS) and the presence of complications. Pain relief was defined as a decrease in at least 50% in VAS.
The database was stored in Microsoft Excel® and the software used for analyzing the data was SPSS 18. A descriptive analysis was made of all the variables studied, supported by the calculation of percentages and descriptive measures. The association between the qualitative variables was also established using the Chi-square test (exact fisher test), and a paired analysis to establish the difference between pain intensity before and after the procedure, using the test, in addition to a bi-variant analysis to assess the association between pain relief with a diagnosis of fibromyalgia, a history of prior surgery and neuropathic pain characteristics. The respective odds ratios (OR) were estimated using a statistical significance of less than 5% and 95% confidence intervals.
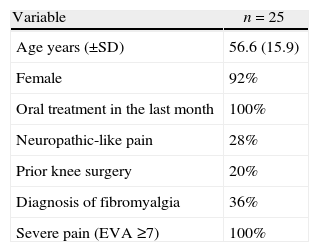
Results25 patients treated with ultrasound-guided saphenous nerve block performed at a pain clinic in the country between September 2011 and June 2012 were analyzed. The mean age was 56.6 years (SD±15.9), and 92% were females. 100% of the patients were receiving oral pharmacological treatment during the last month, with at least acetaminophen, a mild opioid and a tricyclic antidepressant and/or an anti-neuropathic (pregabaline, gabapentin or carbamazepine). Every patient reported severe pain prior to the block (Table 1).
Overall characteristics of patients evaluated.
| Variable | n=25 |
| Age years (±SD) | 56.6 (15.9) |
| Female | 92% |
| Oral treatment in the last month | 100% |
| Neuropathic-like pain | 28% |
| Prior knee surgery | 20% |
| Diagnosis of fibromyalgia | 36% |
| Severe pain (EVA ≥7) | 100% |
SE, standard deviation; VAS, visual analog scale.
Source: Authors’ trial outcomes.
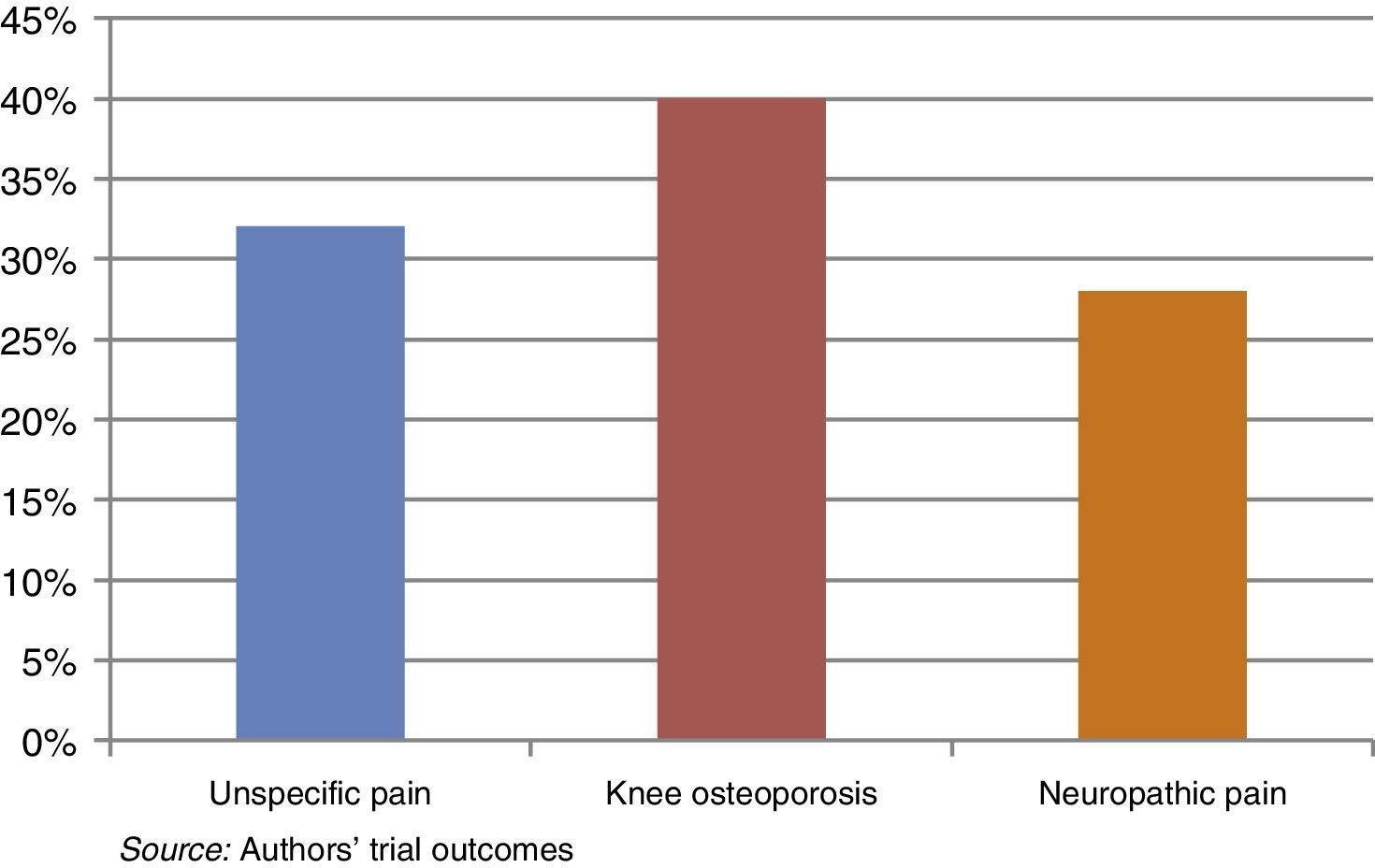
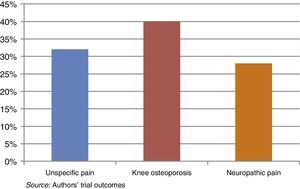
The most relevant diagnosis was unspecific knee osteoarthritis, particularly by the fibromyalgia patients (Fig. 1).
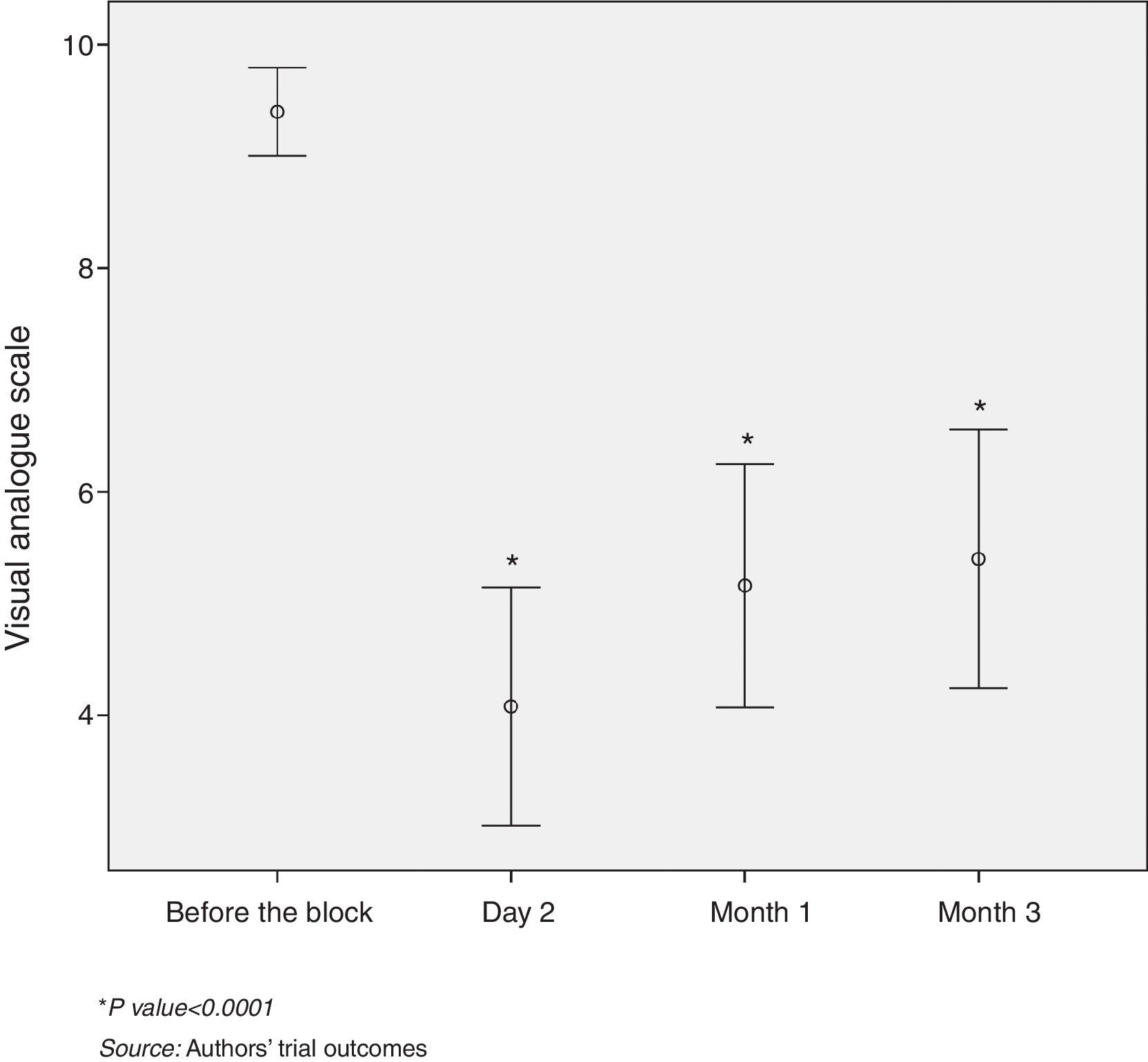
The percentage of patients with pain relief at two days, at one month and at three months following the procedure was 68%, 56% and 40% respectively (Fig. 2).
60% of the patients with pain relief two days after the block had a VAS pain intensity of ≤4. Over 50% of the patients, evaluated one month and three months after the procedure, presented mild to moderate pain intensity (VAS≤6). The difference between the mean initial VAS and the mean VAS score on the second day was 5 points, which was statistically significant (p<0.0001). Likewise, statistically significant differences were identified between the mean initial VAS and the VAS score at one and three months (p<0.0001) (Fig. 3).
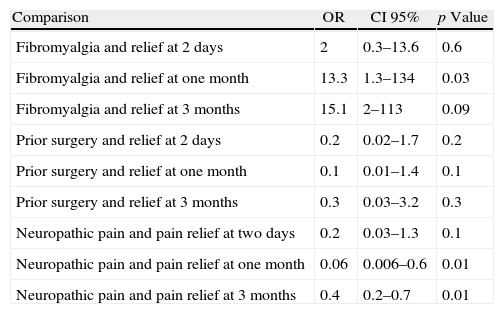
The sub-group analysis yielded similar results in terms of pain relief in patients with fibromyalgia at two days (p=0.6); however, at one month and at three months, the patients with fibromyalgia showed an improved analgesic response, with a statistically significant difference. In contrast, the results in neuropathic pain patients failed to exhibit any improvement at two days, while after one and three months the relief was less noticeable – in fact, none of them reported any improvement after three months. No statistically significant differences were reported during the three follow-up time points in patients who had undergone prior knee surgery (Table 2).
Association of fibromyalgia, neuropathic pain, and prior surgery with pain relief.
| Comparison | OR | CI 95% | p Value |
| Fibromyalgia and relief at 2 days | 2 | 0.3–13.6 | 0.6 |
| Fibromyalgia and relief at one month | 13.3 | 1.3–134 | 0.03 |
| Fibromyalgia and relief at 3 months | 15.1 | 2–113 | 0.09 |
| Prior surgery and relief at 2 days | 0.2 | 0.02–1.7 | 0.2 |
| Prior surgery and relief at one month | 0.1 | 0.01–1.4 | 0.1 |
| Prior surgery and relief at 3 months | 0.3 | 0.03–3.2 | 0.3 |
| Neuropathic pain and pain relief at two days | 0.2 | 0.03–1.3 | 0.1 |
| Neuropathic pain and pain relief at one month | 0.06 | 0.006–0.6 | 0.01 |
| Neuropathic pain and pain relief at 3 months | 0.4 | 0.2–0.7 | 0.01 |
OR, odds ratio; CI, confidence interval.
Source: Authors’ trial outcomes.
No complications were reported.
DiscussionChronic knee pain affects one of every four people over 55 years of age and 70% of them show radiological evidence of OA. There have been reports of a 15% incidence of disability with symptoms ranging from mild to moderate.2,3
The saphenous nerve is the only cutaneous branch of the posterior division of the femoral nerve, originating in the femoral triangle, descending laterally to the femoral artery and into the Hunter adductors canal that crosses over the femoral artery. The saphenous nerve innervates an extensive skin area over the medial aspect of the knee, the leg, the ankle and the foot.4,10–12 The saphenous nerve block, in combination with a sciatic nerve block, provides surgical anesthesia for procedures below the knee, while selective saphenous nerve blocks are preferred for ankle and foot surgeries because it provides anesthesia with no quadriceps motor block.12 The saphenous nerve block also provides analgesia in patients with chronic knee pain.13
This block was reported for the first time by van der Wal et al. using a trans-sartorial approach14; however, this block can be achieved through various approaches, including above the knee, at the level of the knee, below the knee or just on top of the medial malleolus. Above the knee blocks include the perifemoral, sub-sartorial and sartorial approaches, while the knee level blocks include the medial femoral condyle block, with or without nerve stimulation. The block may also be accomplished with a below the knee subcutaneous infiltration, distal to the medial condyle of the tibia. The perifemoral approach is considered more effective, but generates a partial weakness of the hip flexor muscles and the leg extensors.15 This ultrasound-guided block, just as the infra-patellar block, and the saphenous branch, improve postoperative knee pain.4,16,17
The block performed in the patients herein studied was sub-sartorial at the exit of the adductors canal, with a technique inside the plane using a portable ultrasound machine, with lineal transducer (7–12MHz), single puncture. The patients received 8mL of bupivacaine 0.5% with no epinephrine plus dexamethasone 4mg. The block was performed in a room for minor procedures, using aseptic techniques and a 23-gauge hypodermic needle. Patients were placed in a decubitus supine position, with the knee slightly flexed and external rotation of the hip. This approach reduced any adverse side events and improved the analgesia response for a considerable period of time. One single specialist performed the blocks with the participation in some cases of second year residents of anesthesia of a University in the country.
Other techniques may be used for saphenous nerve block in knee pain such as the continuous block of the adductors canal following knee replacement, that is associated with low pain scores at rest and reduces the need for supplementary morphine.17 Nerve stimulation,18 and radiofrequency for refractory anteromedial knee pain, as well as the technique with resistance loss and ultrasound-guided1,19 are additional options available. Generally speaking, all these techniques are yet to be confirmed with randomized, controlled clinical trials.
The percentage success rate reported with the various block techniques are 80% with the perifemoral and sub-sartorial approach; 40% with the medial femoral condyle block and 33% to 65% below the knee.15 When the loss of resistance technique is used, the block rate is approximately 80%, while the use of a nerve stimulator is successful in over 95% of the cases.4 These values correspond to patients with acute knee pain. This trial only included chronic knee pain patients and found lower values probably because of the time of evolution of the disease. On the other hand, Tsai et al. reported a series of 39 cases assessing the efficacy of the ultrasound guided saphenous nerve block with a 77% success rate at 4 months, a figure closer to the rates reported in this trial.13
A follow-up of a cohort of 10 subjects to assess the complete medial aspect block of the leg performed by Benzon et al. reported that the sub-sartorial, perifemoral, and below-the-knee approaches are more effective than the medial femoral condyle block to generate a sensory block of the medial aspect of the leg. The authors reported a complete sensory block of the medial aspect of the leg in 100% of the cases with a sub-sartorial approach and 70% with the perifemoral and below the knee approaches.15 In another trial, De Mey et al. found a 33% incidence with the below the knee approach20 and Van der Wal et al. found a 65% incidence.21
In contrast to the findings of nerve blocks in other anatomical regions, the findings in fibromyalgia patients and in neuropathic-like pain in this trial are striking.22 These data must be carefully analyzed due to the size of the groups and the conclusions cannot be extrapolated to the remaining population of patients with these pathologies. However, these data may be used as a hypothesis for future clinical trials. An OR >1 does not correspond to risk factors but rather to “protection” factors or in favor of the block, since the endpoint was not disease but relief.
Since this was a retrospective trial, there were some limitations to identify some data in the medical records; consequently, we were forced not to include all patients that underwent this block.
ConclusionUltrasound-guided saphenous nerve block for the treatment of chronic knee pain is an effective and safe procedure.
FundingThis review was funded with the authors’ own resources.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Arcila Lotero MA, Díaz RR, Mejía Aguilar MA, Jaramillo Jaramillo S. Eficacia y seguridad del bloqueo del nervio safeno guiado por ultrasonido en pacientes con dolor crónico de rodilla. Rev Colomb Anestesiol. 2014;42:166–171.