Introduction: The use of fiberoptic bronchoscopy as a tool for tracheal intubation is relatively new in our setting. Its availability has been increasing, and hence the need for anesthetists to receive adequate training in the use of this device. Knowledge and mastery of this technique, following all the necessary steps, is the starting point for the successful performance of a procedure.
Objective: These guidelines describe the technique for intubation using the fiberoptic bronchoscope at the Evaristo García University Hospital of the Colombian Department of Valle.
Methodology:This paper is based on a review of the literature, the authors' experience, and a discussion forum.
Results:Presentation of the guidelines for intubation using fiber optic bronchoscope at the Evaristo García University Hospital. Description of the technique for constructing a mask for patient ventilation during tracheal intubation under fiberoptic bronchoscopy.
© 2012 Sociedad Colombiana de Anestesiología y Reanimación. Published by Elsevier. All rights reserved.
Introducción:El recurso del fibribroncoscopio como instrumento para la intubación traqueal es relativamente reciente en nuestro medio. La disponibilidad del mismo es cada vez mayor y con ella, la necesidad que los anestesiólogos se entrenen suficientemente en el uso de este equipo. Conocer y dominar una técnica, respetando cada uno de sus pasos, es el primer paso a la realización exitosa de un procedimiento.
Objetivo:En la presente guía se describe la técnica utilizada en para la intubación con fibrobroncoscopio en el Hospital Universitario del Valle Evaristo García.
Metodología:El artículo se basa en la revisión de la literatura, la experiencia de los autores y un foro de discusión.
Resultados:Se presenta la guía para la intubación con fibrobroncoscopio en el Hospital Universitario del Valle Evaristo García. Se describe la técnica para la construcción de una máscara para la ventilación del paciente durante el procedimiento de intubación traqueal con la utilización del fibrobroncoscopio.
© 2012 Sociedad Colombiana de Anestesiología y Reanimación. Publicado por Elsevier. Todos los derechos resevados.
The use of fiberoptic bronchoscopy to facilitate endotracheal intubation was introduced recently1 and has been gradually increasing, not only for the management of patients with airway disease, but also in other clinical situations such as, checking the placement of the tracheal or endobronchial position of the tube, and examining the upper airway, larynx, trachea, and bronchial tree.
The learning curve for intubation under fiberoptic bronchoscopy2, 3 must always be developed in patients with a normal airway, and is considered completed after at least 10 successful single attempts in less than 2 minutes.4
In patients with an airway that is considered difficult5, 6 or with abnormal anatomy, the first attempt at intubation when the fiberoptic bronchoscopy technique is used7, 8 must always be made by the anesthetist with the longest experience in performing the procedure, considering that the life of the patient is the primary consideration, above and beyond academic interest; moreover, the first attempt may be the best opportunity to access the airway before the situation becomes difficult as a result of secretions, edema or bleeding.9, 10
The recommendation in cases with predictors of a difficult airway is to perform the procedure with the patient awake,11–15 because the situation may change suddenly. For example if there is a need to approach the airway on an emergency basis, in which case the usefulness of the fiberoptic bronchoscope may be limited; and hence the need to be prepared with alternative devices.16
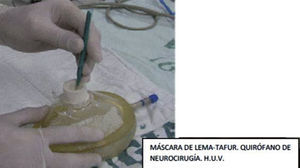
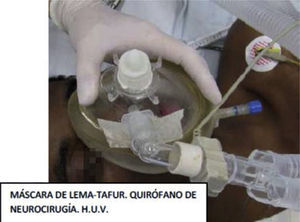
The teaching mask (Lema-Tafur mask), designed more than 10 years ago, permits a prolonged attempt at intubation with the fiberoptic bronchoscope while the patient is in apnea or spontaneous ventilation under profound sedation (for training purposes).17 The peculiarity of this mask is that it may be constructed by any anesthetist, using elements normally available in the operating room. A similar mask that serves the same purpose is available in the United States market under the name of multi-port mask, or Patil mask.18, 19
Recommendations for use of the fiberoptic bronchoscopeThe following recommendations were developed on the basis of a review of the literature available in PubMed regarding the technique and the learning process, and also on the experience in our Department that resulted in a group activity to review and share these guidelines.
The fiberoptic bronchoscope must not be lubricated with gels or lidocaine spray: only normal saline solution or distilled water must be used to help slide the tube. On the other hand, lack of lubrication may hinder withdrawal of the fiberoptic bronchoscope.20
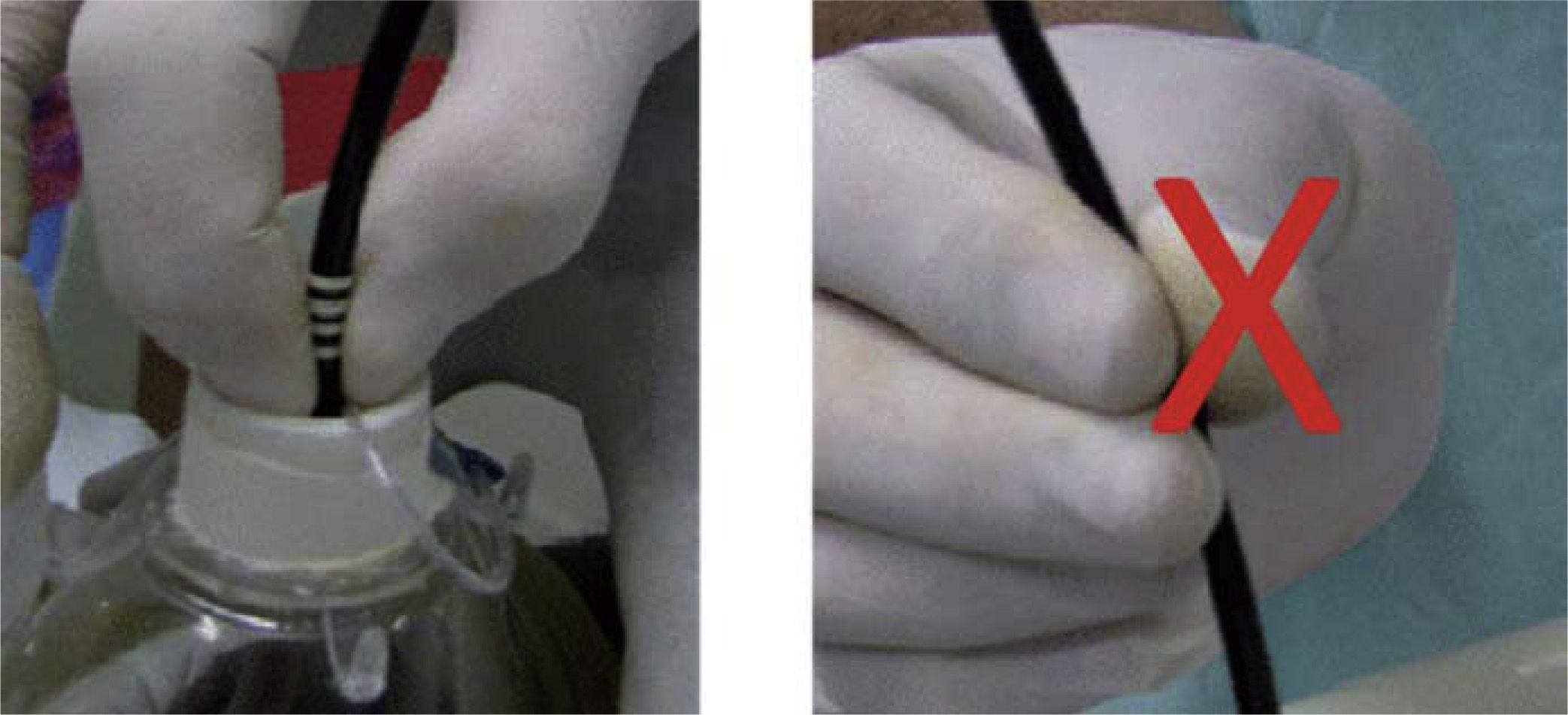
The optic fiber must be grasped only with two fingers, usually the thumb and the index fingers. When the fingers are supported on three points on the fiber, there is a greater risk of pressure breakage (fig. 1).
The fiberoptic bronchoscope must be washed according to the internal policy of the institution policy for handling flexible endoscopic devices.
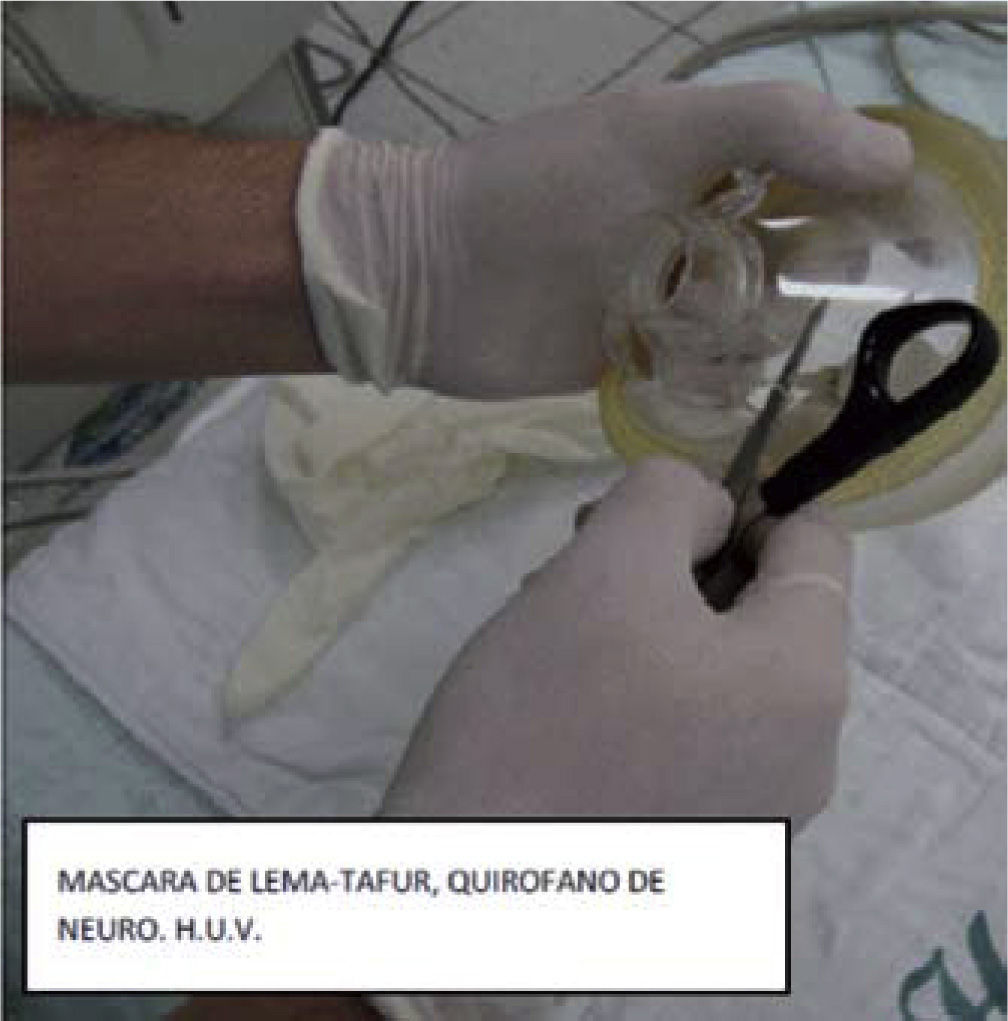
Lema-Tafur maskWith a sharp instrument, gently make a hole large enough to pass a 7 or 7.5 orotracheal tube connector on the side of the mask. The hole will be used to connect the ventilation system (fig. 2).
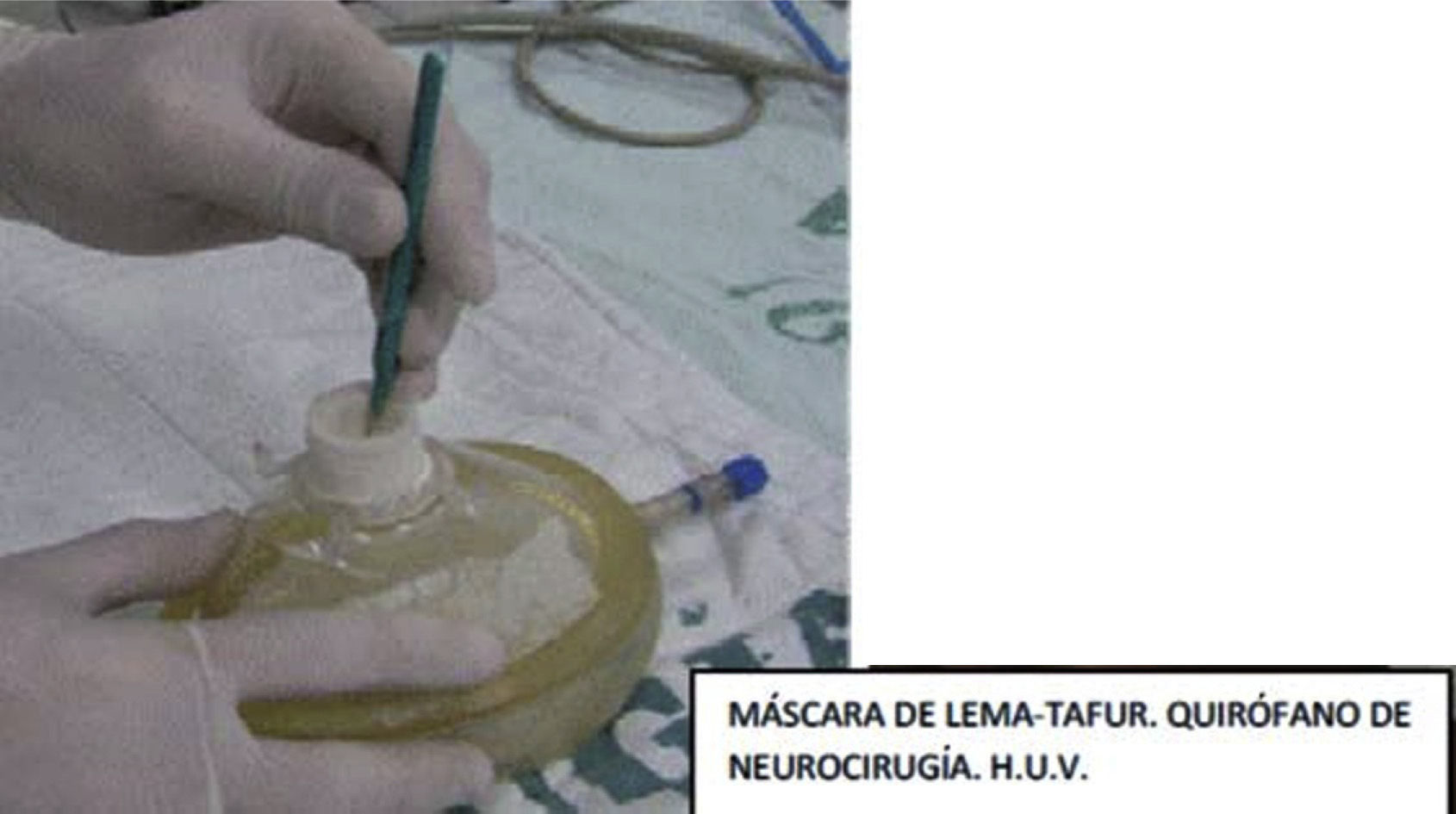
Place a gloved finger on the upper part of the mask and fix it with adhesive tape (fig. 3). Then make a very small hole to pass the device with the help of a scalpel blade (fig. 4).
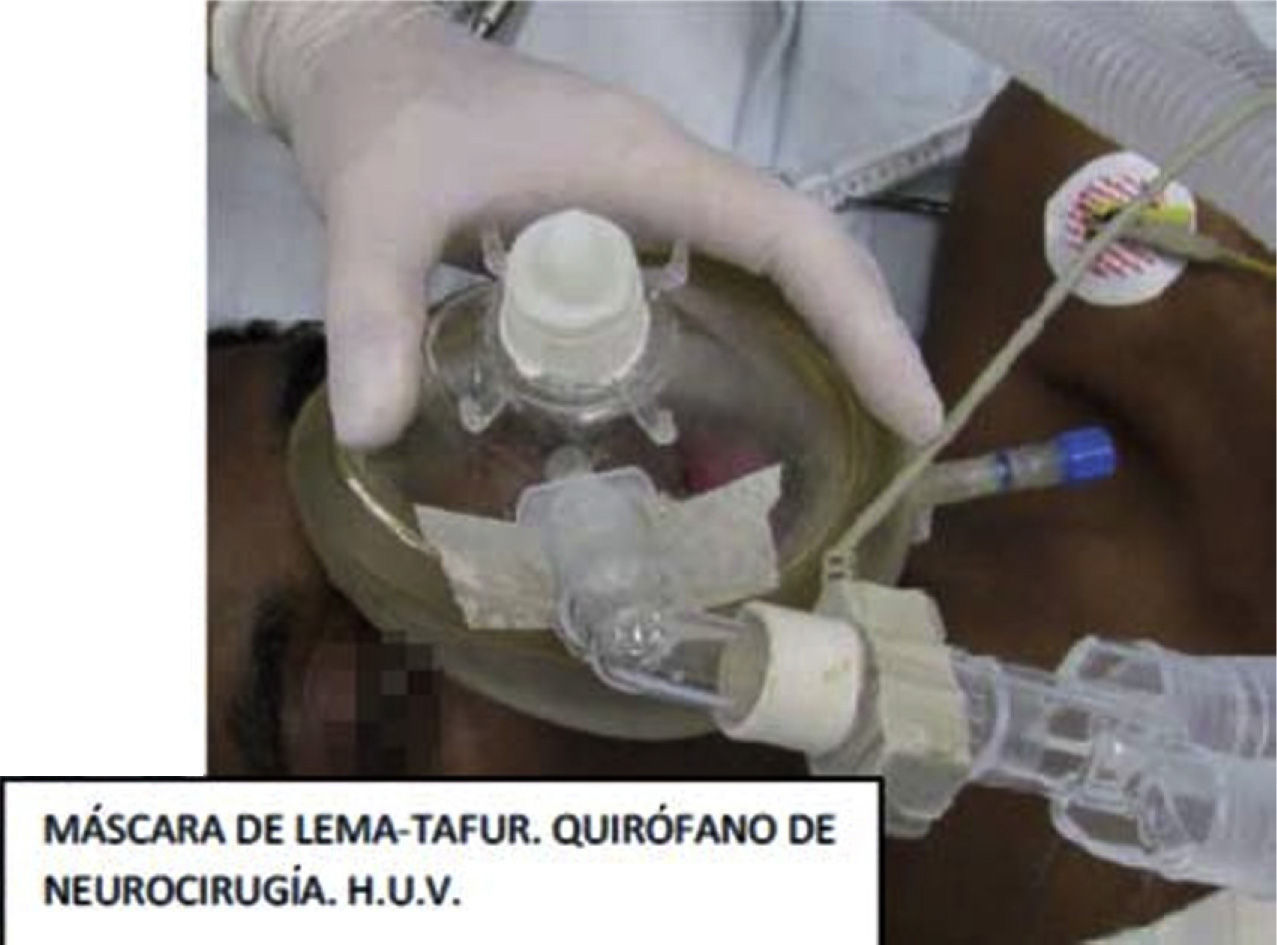
Connect the ventilation system with the help of the orotracheal tube connector and ventilate the patient, or allow the patient to breathe spontaneously (fig. 5). This is the final step before the Lema-Tafur device is ready to use.
Procedure- -
Describe the procedure to the patient and explain what he/she may feel and the reason why he/she will be awake during the intubation process (under normal circumstances, this will help reassure the patient).
- -
Premedicate with metoclopramide and ranitidine at least 1 hour before the procedure.21
- -
Micronebulize with 5–10 ml of 2% lidocaine 20 minutes before the procedure.22–25
- -
Prepare the cart for airway management, the anesthesia machine, and resuscitation and anesthesia drugs.26
- -
In pediatric patients and in those adult patients who require it, their pathology permitting it, atropine may be used as antisialagogue.27, 28
- -
As far as the technique is concerned, the recommendation is to intubate through the nasal approach,29 since it is better tolerated by the patient and, additionally, the nasopharyngeal anatomy itself guides the tip of the device towards the larynx, facilitating the identification of the glottis and the vocal chords. For nasotracheal intubation, the most permeable nostril must be used in adults and the less permeable in pediatric patients. It is important to bear in mind that prolonged nasal intubation has a higher incidence of sinusitis compared to the orotracheal approach.30, 31
- -
Spray lidocaine inside the selected nostril, plus oxymetazoline with the help of a nasal "wick", at least 10 minutes before the procedure.32, 33
- -
The use of a bite protector is mandatory for orotracheal intubation. It is also recommended to warm the tube by placing it in warm saline solution in a basin in order to improve its flexibility; introduction of the fiberoptic bronchoscope into the airway may be easy, but advancing the tube may be difficult because of the oropharyngeal and hypopharyngeal angles.
- a.
Spray lidocaine on the base of the tongue and the pharynx and instruct the patient to gargle and then inhale (remember that one lidocaine spray delivers 10 mg, and that the maximum dose of local anesthetic must not be exceeded). This technique is then supplemented by instilling 2% lidocaine through the fiberoptic bronchoscope under direct visualization, exactly over the vocal chords.
- b.
Blocks: If the previous step does not attenuate the swallowing and cough reflexes, 3 cc of 2% lidocaine may be applied through the cricothyroid membrane,34 using a 22-gauge Jelco® catheter. The anesthetic elicits a cough reflex, hence the need to pay close attention to the manipulation of the needle at the neck, because it may mean additional risks for the patient.35, 36
- c.
A glossopharyngeal nerve block37 in the tonsillar pillars is not recommended because of the risk of puncturing the carotid arteries, or the protracted loss of protective reflexes of the upper airway.
- -
The operator must be familiar with techniques for blocking the upper airway, because that block will be required in cases where the previous steps are insufficient.
- -
The total dose of lidocaine must not exceed 7–10 mg/Kg of body weight.38, 39
- -
Except in cases of cervical trauma, the patient must be positioned with cervical and atlanto-axial extension. In the anesthetized patient, either with ventilation or spontaneous breathing, forward mandibular dislocation and outward traction of the tongue may facilitate the success of the procedure.40
- -
Ideally, the operator of the fiberoptic bronchoscope must be situated at the patient's head.
- -
When using the Lema-Tafur mask, the connector between the tube and the ventilation system must be removed, but placed within reach; otherwise, the tube will not go through the device when advanced. The tube without the adapter must be attached to the upper part of the fiberoptic bronchoscope (fig. 6). In 80%-85% of patients, the epiglottis and vocal chords may come into view with just a slight manipulation of the tip of the fiberoptic bronchoscope.41
It is not recommended to insert the tube in the nostril initially, because of a higher risk of bleeding; it is better to advance the fiberoptic bronchoscope first until the carina is visualized, and then introduce the tube42 (fig. 7).
Pharyngolaryngeal structures should be visible after advancing 10 cm. Try to visualize the middle turbinate, then the epiglottis, and finally find the way towards the larynx. Then pass the fiberoptic bronchoscope through the vocal chords until the tracheal rings come into view and you come close to the carina. If there is foamy saliva, you are probably in the esophagus. Pull back slowly, directing the tip anteriorly very gently; this will help you locate the airway. In patients breathing spontaneously, it is useful to follow the bubbles of secretions created by the flow of air.
After visualizing the carina, lower the externally-lubricated tube. From that point on, the scope serves only as a guide, and you must focus your attention of the descent of the tube (fig. 8).
It is often difficult to advance the tube over the fiberoptic bronchoscope because of factors such as the laryngeal anatomy, the tube design and flexibility, and the size of the scope.43 If there is resistance beyond the pharynx, it is usually at the epiglottis or the right arytenoid; in that case, draw back the tube 1-3 cm and rotate it counter clockwise 45° to 90° and then reintroduce it gently.44 If it does not advance, think about introducing a smaller tube and repeat the whole procedure. It is recommended not to apply pressure, because it has been found to be associated with laryngeal trauma.9
Check the desired position of the tube (monobronchial or tracheal). Do not give sedatives or hypnotics before making sure that the tube is indeed in the airway; this is achieved by observing the ventilation cuff, or using capnography and auscultation.
In the anesthetized and paralyzed patient, the tongue and soft tissues of the pharynx collapse and close the hypopharynx, restricting vision and the handling of the fiberoptic bronchoscope. Patients with a history of snoring, obstructive apnea, obesity, mandibular hypoplasia or nasal obstruction, or those with tonsillar hyperplasia are especially vulnerable to airway collapse during anesthesia.45 Additionally, apnea time and clinical control of the patient mean that it is impossible to carry out this procedure without the help of one or two trained assistants. Maneuvers such as lingual traction or anterior mandibular advancement help clear the airway; alone, they are beneficial, but they are more effective when performed together.46
The failure rate with fiberoptic bronchoscopy intubation is around 14.8% in the first attempt with the patient awake, and around 6.1% in anesthetized patients;47 however, these figures may be modified now that undergraduate and graduate courses offer training in airway management in general, and in management of the difficult airway and use of fiberoptic bronchoscopy in particular.48, 49
Complications, including esophageal perforation and barotrauma are quite rare, but may be fatal when they occur.50, 51 Severe epistaxis was the most common complication in a recent study (1.3% of cases).52 When there is resistance to tube advancement over the fiberoptic bronchoscope, there is a risk of severe laryngeal trauma, resulting in hoarseness, dysphonia and dysphagia in the immediate postoperative period.10
ConclusionsApproaching the airway with the fiberoptic bronchoscope is a safe technique, but it requires supervised training.
As with all techniques, following a guideline or a protocol when performing the procedure will ensure a high probability of success, because it will avoid improvisation, regardless of the expertise with direct operation of the fiberoptic bronchoscope.
Learning the intubation technique using the fiberoptic bronchoscope must start in patients with a normal airway or in mannequins. The Lema-Tafur device is easy to construct and is helpful in training as well as in cases where the fiberoptic bronchoscope is used for approaching the airway.
Competing InterestsNone declared.
Funding: The authors' own funds.