Surgical care is an integral component of healthcare services in all countries, and its quality is evaluated through monitoring of national indicators of safe surgical and anaesthesia care. In Peru, monitoring is only partial because of the lack of data regarding some of the indicators. However, there is a need for comprehensive monitoring in order to gain knowledge of the progress towards the healthcare goals proposed by the World Health Organisation and The Lancet Commission Global Surgery.
La atención quirúrgica es un componente integral de los sistemas sanitarios en todos los países, y la valoración de su calidad se realiza a través de la monitorización de indicadores nacionales de atención segura quirúrgica y anestésica. En Perú, esta monitorización se realiza de forma parcial, pues no hay información respecto a algunos indicadores. Sin embargo, debería ser integral para conocer el progreso de los objetivos sanitarios propuestos por la Organización Mundial de la Salud y la Comisión Lancet en Cirugía Global.
Surveillance in public health has used standardised measurements designed to quantify the cost of disease in a population, monitor mortality rates, and provide guidance to health systems. Maternal mortality (MM), infant mortality (IM) and life expectancy (LE) rates have been important indicators for measuring the effectiveness of healthcare services over a considerable time period. However, as a result of the increase in LE in the world, as well as the drop in MM and IM rates, other measurements such as surgical care have gained important when it comes to evaluating the health system.1
Surgical services are integral components of the public health system because they are part of the continuous primary care process. Although they have been recognised as a costly component, surgeries are performed in both affluent and precarious economic contexts alike.2,3 In 2012, 312.9 million surgical procedures were carried out in the world4; however, information regarding frequency and safety of this care was severely limited by the lack of national data, considering that 70% of countries had no information on their national surgery volumes, and practically none attempted to value the allocation of surgical resources or the results.1
Peru was not an exception, because up until recently it did not monitor the main indicators on preparation, provision and effect of safe and affordable surgical and anaesthesia care for the population.1,5 Some of the characteristics of the Peruvian health system are described below, followed by current considerations regarding monitoring of indicators and, finally, proposed measurements for comprehensive monitoring.
The Peruvian health systemA mixed system, it comprises two large sub-sectors, public and private, with different assets and sources of funding coming from tax collection (Ministry of Health – MINSA – with its offering of Comprehensive Health Insurance – SIS), social security contributions through taxation on active worker salaries (Social Health Insurance – EsSalud), and premium payments for private insurance. This results in a fragmented system with several weaknesses such as network overlap, inability to provide comprehensive care, and absence of complementary services and continuity of care.6,7
Timely access to essential surgeryTimely surgical care is the ability to receive rapid and appropriate care from a healthcare institution (primary care level hospital) within a two-hour period.5,8 A segment of the Peruvian population lives at high altitude in the Andean region where access is difficult, but travel time to the closes healthcare institution (IPRESS) went down from 39 to 42min (walking), and from 27 to 23 in motor vehicles, between 2011 and 2014.9 However, these time periods were estimated for the total number of healthcare institutions, including many facilities without surgical care capability.
National surgical volumeAccording to the National Health Superintendency (SUSALUD), 613,396 surgical procedures (major and minor)10 were performed in 31,151,643 inhabitants, for a rate of 1969 surgeries for every 100,000 inhabitants in 2015. The Lancet Commission on Global Surgery (LCGS) proposed that, by 2030, countries should be performing at least 5000 major procedures for every 100,000 inhabitants per year, given that it is the volume that correlates with several desirable health results such as a LE of 74–75 years, a MM rate of less than 100 women for every 100,000 live births, and the 143 million additional surgeries required worldwide in order to save lives and prevent disability. Moreover, this figure could be used for benchmarking surgical services and as a target for monitoring the execution of surgical care plans at a national level.5,11,12
Number of operating roomsThe total number of Peruvian healthcare institutions (IPRESS) that provide surgical care are already registered in an electronic database called the National Registry of Healthcare Institutions (RENIPRESS) belonging a SUSALUD, although there is no information on the number of operating rooms that are operational in each surgical service. This means that there are no data regarding the volume of surgical patients per operating room per year.13 Only ESSALUD reported running 250 operating rooms at a national level, covering 10,754,665 affiliates in 2015.14,15
Density of surgical specialistsIn 2014, there were 1382 specialists accredited as anaesthetists and 8804 accredited as surgeons (all surgical specialties).16 However, in the Medical College of Peru (MCP) database, licensure figures for 2016 were 1706 anaesthetists, 6765 surgeons and 3055 obstetricians and gynaecologists,17 accounting for a rate of 36.6 specialists for every 100,000 inhabitants in a total population of 31,488,625 inhabitants.18 But this rate might be higher considering that many physicians graduating from residency programmes practice in different specialties without having yet obtained their professional degree, which is a pre-requisite for inclusion in the national MCP database of specialists.
There is a correlation between this density figure and the MM rate given that, for every 10 increment units there is a 13.1% (95% CI 11.3–14.8) reduction in the MM rate.19 For this reason, the LCGS has emphasised the importance of achieving a minimum density of 20 specialists for every 100,000 inhabitants by 2030.20
Protection against impoverishment and catastrophic healthcare expendituresThe percentage of the Peruvian population with access to coverage, as well as the total health expenditure per capita (THEPC) increased steadily during the time period between 2004 and 2014 (from 37.3 to 69%, and from int. $282.22 to int. $656.18, respectively).10,21,22 However, a segment of the population (27% or nearly 8 million, including more than 1.7 million in a situation of poverty) has no coverage whatsoever and, consequently, no way to access healthcare services. This creates a risk of impoverishment and catastrophic spending associated with surgical care. The Peruvian population exposed to the risk of such expenditures is 36.1% and 29%, respectively, according to a research based on stochastic and surgical cost models.23,24
This indicator is subject to continuous monitoring by the National Statistics and Information Techology Institute (INEI) as part of the sustainable development goals, as a way to evaluate the goal on universal health coverage, including protection against financial risks.25
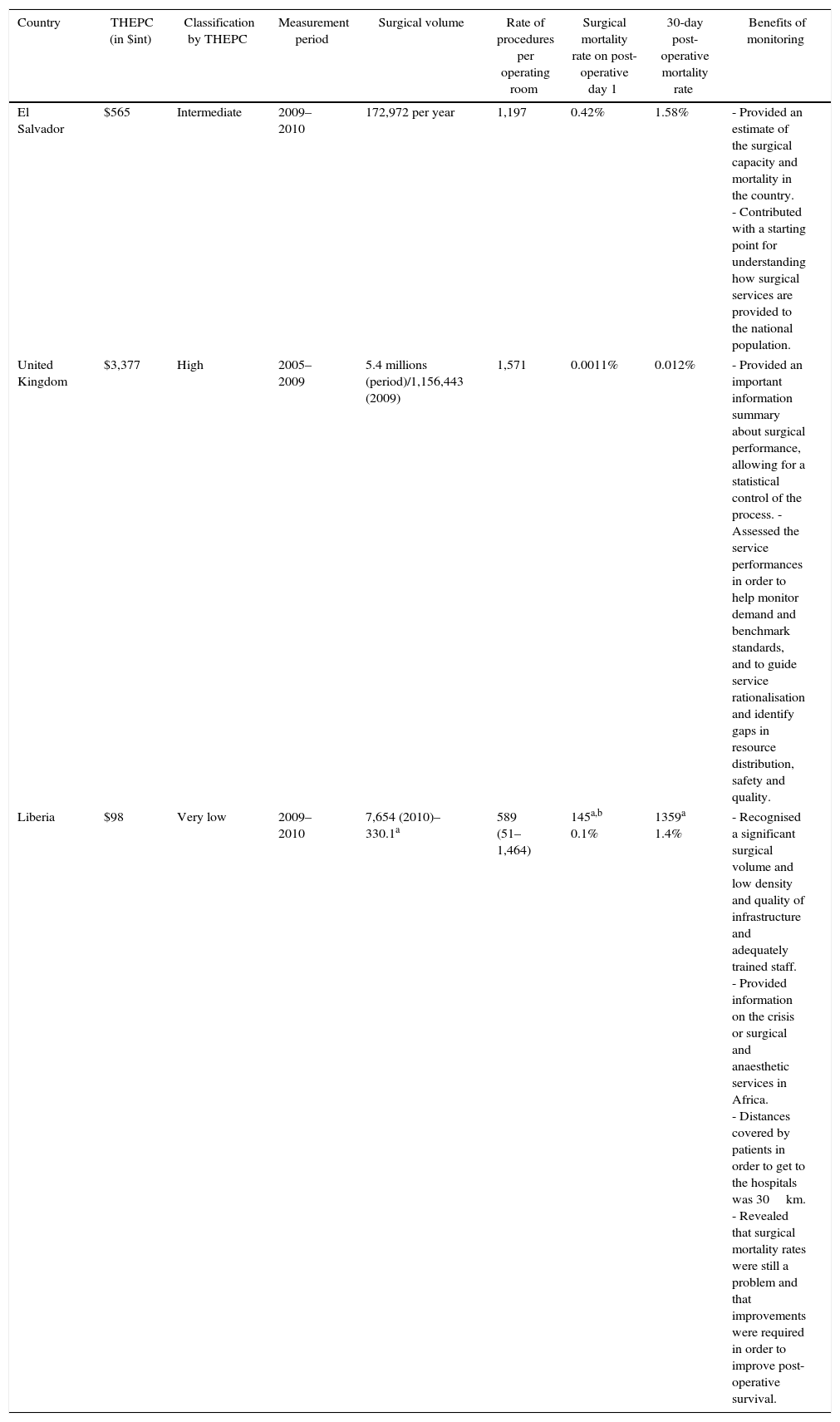
Problems associated with absent indicatorsAbsent indicators include timely access to essential surgery, number of operating rooms, and mortality rates during hospitalisation (with reasonable correlation with 30-day mortality),5,26 and they preclude comprehensive monitoring and knowledge of the magnitude of the work performed in surgery and anaesthesia. Likewise, absent indicators do not allow to quantify the impact of the national regulations on safe and standardised anaesthesia care (including the World Health Organisation surgical safety checklist).27,28 Consequently, it is not possible to address deficiencies in peri-operative outcomes29 or guide national surgical care policies and programmes.30 In contrast, Table 1 summarises the benefits derived from this form of monitoring in three countries with different THEPC and surgical volumes (El Salvador, United Kingdom and Liberia).31–35
Monitoring of national safe surgery indicators in three countries with different THEPC.
| Country | THEPC (in $int) | Classification by THEPC | Measurement period | Surgical volume | Rate of procedures per operating room | Surgical mortality rate on post-operative day 1 | 30-day post-operative mortality rate | Benefits of monitoring |
|---|---|---|---|---|---|---|---|---|
| El Salvador | $565 | Intermediate | 2009–2010 | 172,972 per year | 1,197 | 0.42% | 1.58% | - Provided an estimate of the surgical capacity and mortality in the country. - Contributed with a starting point for understanding how surgical services are provided to the national population. |
| United Kingdom | $3,377 | High | 2005–2009 | 5.4 millions (period)/1,156,443 (2009) | 1,571 | 0.0011% | 0.012% | - Provided an important information summary about surgical performance, allowing for a statistical control of the process. - Assessed the service performances in order to help monitor demand and benchmark standards, and to guide service rationalisation and identify gaps in resource distribution, safety and quality. |
| Liberia | $98 | Very low | 2009–2010 | 7,654 (2010)–330.1a | 589 (51–1,464) | 145a,b 0.1% | 1359a 1.4% | - Recognised a significant surgical volume and low density and quality of infrastructure and adequately trained staff. - Provided information on the crisis or surgical and anaesthetic services in Africa. - Distances covered by patients in order to get to the hospitals was 30km. - Revealed that surgical mortality rates were still a problem and that improvements were required in order to improve post-operative survival. |
The WHO has emphasised that national monitoring of these indicators must be implemented urgently in all member countries because it will enhance the understanding of unmet needs, improve overall surgical and anaesthetic capacity in the context of universal health coverage, and will help implement reliable steps regarding access to essential surgery and anaesthesia.3
Proposals for achieving comprehensive indicator monitoringBecause of its fragmentation, the Peruvian health system will require a number of actions to unify information coming from the different sub-sectors in order to consolidate single national indicators. Proposed measures include the following.
First of all, strengthening tools for automated collection of standardised indicator data. Several are already available in various health sub-sectors, but SUNASA has a suitable software for entering standardised data through RENIPRESS,13 which displays open information regarding infrastructure, equipment, human resources and organisation (including availability of surgical services) of healthcare institutions (IPRESS) of all the sub-sectors. It also supports IPRESS registration, categorisation, information updates and withdrawals. Consequently, it could consolidate data regarding indicators pertaining to such things as active operating rooms and post-operative mortality in each Peruvian healthcare institution.36
Second, collection of health information by means of population-based mechanisms (census). The INEI has scheduled a geo-referenced population census in 2017 using a mapping process of the total number of Peruvian households. This census will allow to obtain updated information of population segments with health coverage.37,38 It could also estimate the time required to access a healthcare institution with surgical services by means of geospatial mapping, as has been done indirectly in other countries through multiple interviews with hospital representatives.8
Equally important is continuous coordination between MCP, scientific societies of surgical specialties, the National Council (CONAREME) and medical residency programmes in order to acquire accurate consensus data regarding the existing number of surgical specialists in Peru. These open data will serve to compare regional realities within the national context, identifying regions with a deficit of specialists in order to inform plans for corrective action.
Moreover, it would be desirable to develop a national plan for safe surgery in order to coordinate policies in accordance with the national and supranational regulations regarding staffing, infrastructure, provision of care, financing and use of the information.5
Finally, a national observatory consisting of representatives of the health sub-sectors would provide continuous monitoring of surgical and anaesthesia care indicators.
FundingThe author did not receive sponsorship to carry out this article.
Conflict of interestThe author declares having no conflicts of interest.
Please cite this article as: Shiraishi-Zapata CJ. Monitorización de indicadores nacionales de atención quirúrgica en el sistema sanitario peruano. Rev Colomb Anestesiol. 2017;45:210–215.