Pudendal nerve blocks have a wide range of clinical applications for the management of acute post-operative pain in urologic, gynecological surgery, in coloproctology, as well as in pain medicine for differential diagnosis, and for the management of pudendal neuropathies. However, despite its benefits it is infrequently used.
ObjectiveTo perform a detailed description of the most recent ultrasound-guided techniques with the aim of encouraging safe and reproducible learning.
Materials and methodsWe have performed a broad, non-systematic review of the literature through Medline, Embase and Science Direct between 1985 and 2016, to evaluate the most relevant articles, using the following key words: pudendal nerve anatomy, pudendal nerve, pudendal nerve blocks, pudendal nerve ultrasound, pudendal neuralgia, nerve entrapment, chronic pain, Alcock canal, and pelvic pain. The search was limited to articles published in Spanish, English and French.
ResultsRecent descriptions were found of a large number of anatomic variants, which are described in detail and shown in graphic documents in order to facilitate the sonoanatomic correlation of nerve location as a guide for the performance of the pudendal nerve block through the different approaches.
ConclusionsThe deep and detailed knowledge of the anatomy of the pudendal nerve and its variations is essential for the realization of Regional Anesthesia techniques guided by images.
These promising techniques should continue to be evaluated with clinical studies.
Los bloqueos del nervio pudendo poseen un amplio rango de utilidades clínicas en el manejo agudo de dolor POP en cirugía urológica, ginecológica, en coloproctología así como en Medicina del dolor en diagnóstico diferencial y manejo de las neuropatías del nervio pudendo. Sin embargo su aplicación es relativamente infrecuente a pesar de los beneficios.
ObjetivoRealizar una descripción detallada de las técnicas más recientes guiadas por ultrasonografía con el objeto de motivar su aprendizaje de una manera segura y reproducible.
Materiales y métodosSe realizó una revisión amplia, no sistemática de la literatura a través de Medline, Embase y Science Direct desde 1985 hasta 2016, evaluando los artículos más relevantes, utilizando las palabras clave: anatomía del nervio pudendo, nervio pudendo, bloqueos del nervio pudendo, ultrasonido del nervio pudendo, neuralgia del pudendo, atrapamiento nervioso, dolor crónico, canal de Alcock y dolor pélvico. La búsqueda se limitó a artículos publicados en español, inglés y francés.
ResultadosSe encontraron recientes descripciones de una gran cantidad de variantes anatómica, que se describen en detalle y muestran en documentos gráficos con el propósito de facilitar la correlación sonoanatómica de la localización del nervio como guía para la realización de bloqueos de nervio pudendo a través de los diferentes abordajes.
ConclusionesEl conocimiento profundo y detallado de la anatomía del nervio pudendo y sus variaciones es esencial para la realización de técnicas de anestesia regional guiada por imágenes. Estas técnicas promisorias deben continuar evaluándose con estudios clínicos.
Pudendal nerve blocks have a wide range of clinical applications1,2 that involve anaesthetic/analgesic goals: haemorrhoid,3–6 ano-rectal, vaginal, and perineal7 surgery; labour,8 episiotomies,9,10 prostate biopsy,11 prostate brachytherapy,12 interstitial cystitis,13 and penile surgery.14 Moreover it is an integral part of the diagnosis and therapy of pudendal neuropathy of which little is known, although there is growing research into its pathophysiology and therapeutic approaches.2,14–20
Despite the above, pudendal nerve blocks are not a popular technique in daily practice in general, urologic or obstetric surgery, perhaps because of lack of knowledge of the block or because of the frequency of blind blocks with variable or incomplete results.8 At present, with the popularity of ultrasound-guided blocks21–32 it is important to review the anatomy, sonoanatomy and some relevant technical aspects that may make its implementation a safe and reproducible practice.
ObjectivePudendal nerve blocks are an option to consider in certain urologic, gynaecologic and coloproctology procedures and, more recently, also in the pain clinic, thanks to the growing development of ultrasound as a neurolocalisation technique. The objective of this study was to review the indications and techniques for pudendal blocks, taking into account recent detailed descriptions of the complexity and anatomic variants of the pudendal nerve as determining factors for success with the block, and for the education process required to disseminate the benefits.
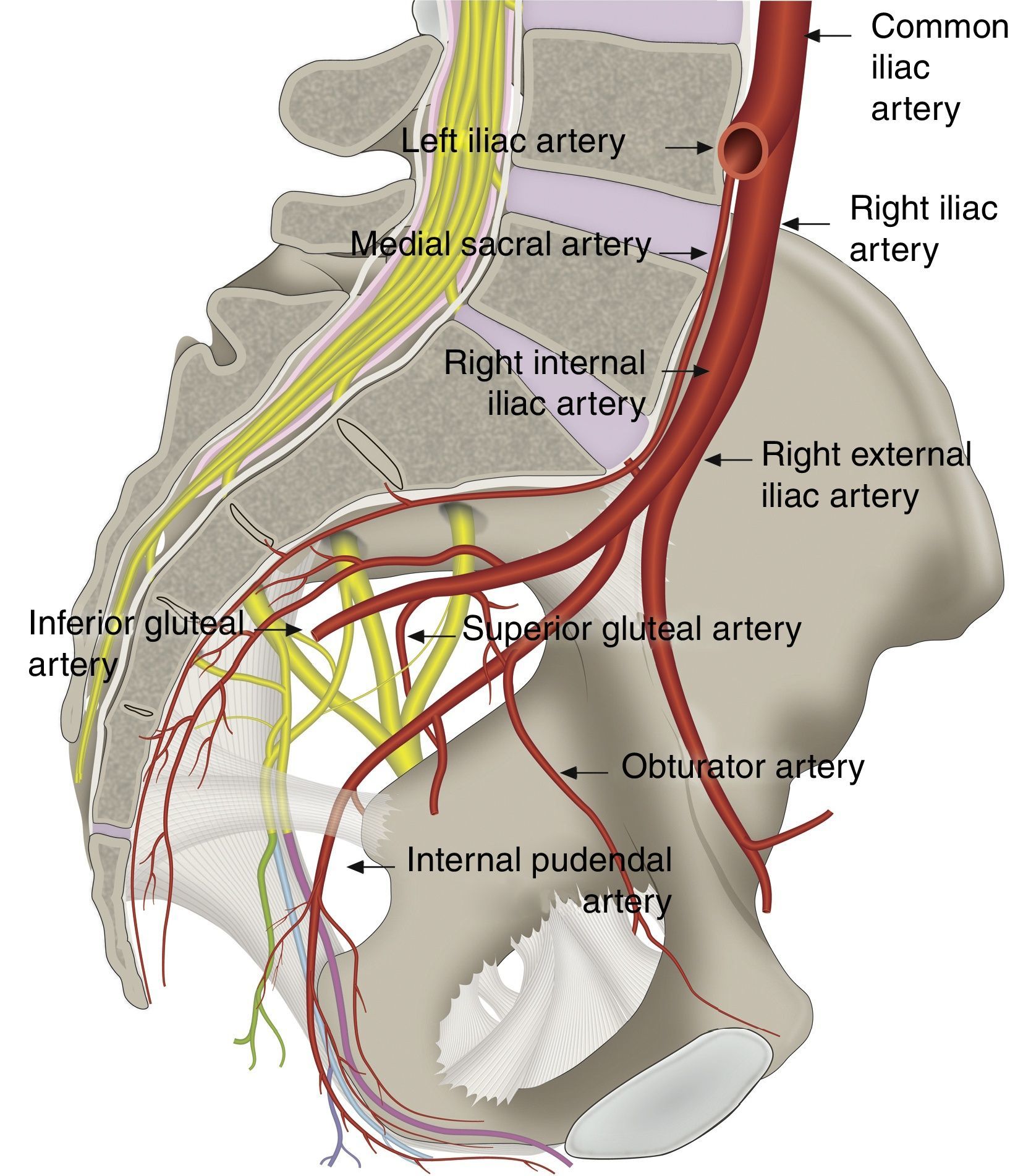
Pudendal nerve anatomyThe pudendal nerve is the main nerve of the perineum,33 the pelvic floor muscles18,34 and the external sexual organs. It was described by Benjamin Alcock in 1836 as he studied the course of the internal pudendal artery35–37; since that time, interesting descriptions of its complexity and anatomic variability have been made.35,38–44 The nerve receives input from the primary ventral roots of S2–S4 in the sacral plexus, forming 1, 2 or three trunks before its final branching41,45; variable contributions from S1 and/or S546–49 have also been described. When supply to the plexus is mainly from S2 and S3, it is called a prefixed plexus, and when the main contributions are from S3 and S4, it is called a postfixed plexus.43
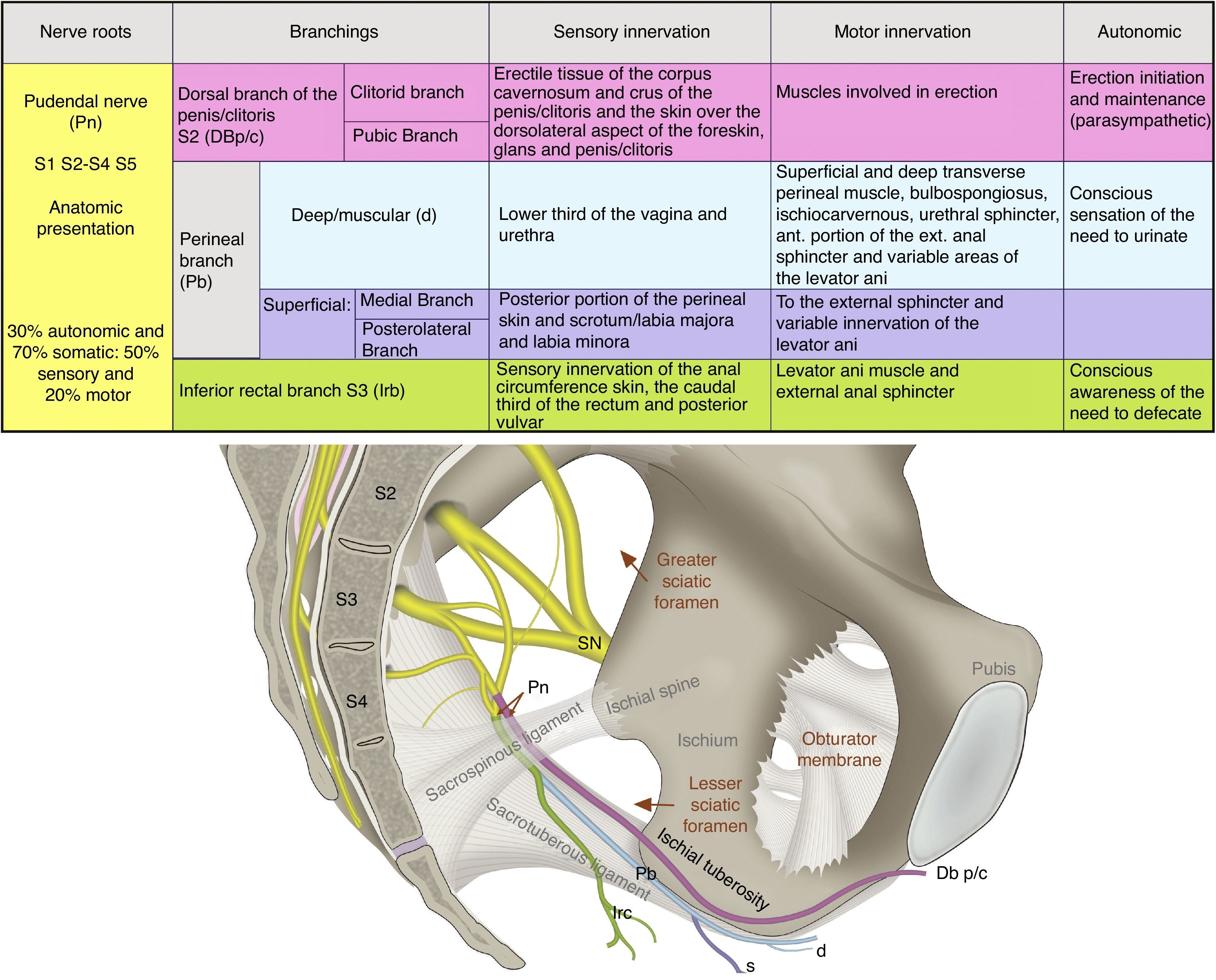
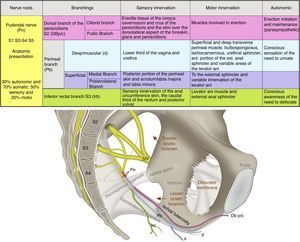
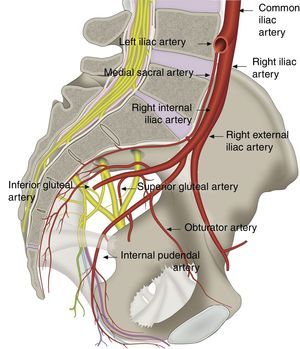
The pudendal nerve consists of 70% somatic fibres and 30% autonomic fibers. The visceral branch has 4–6 branches that connect with the roots of S2–S4 in order to form the pelvic sympathetic and parasympathetic plexus as shown in Fig. 1.48,50
Anatomy and function of the pudendal nerve (Pn), formed by the roots of S2–S4. Its branches include the dorsal branch of the penis/clitoris DBp/c; the perineal branch (Pb) with its deep (d) and superficial (s) branches, as well as the inferior rectal branch (Irb) in its relation with the sacrospinous and sacrotuberous ligaments; the greater and lesser sciatic foramen; the ischial spine and the sciatic nerve (SN).
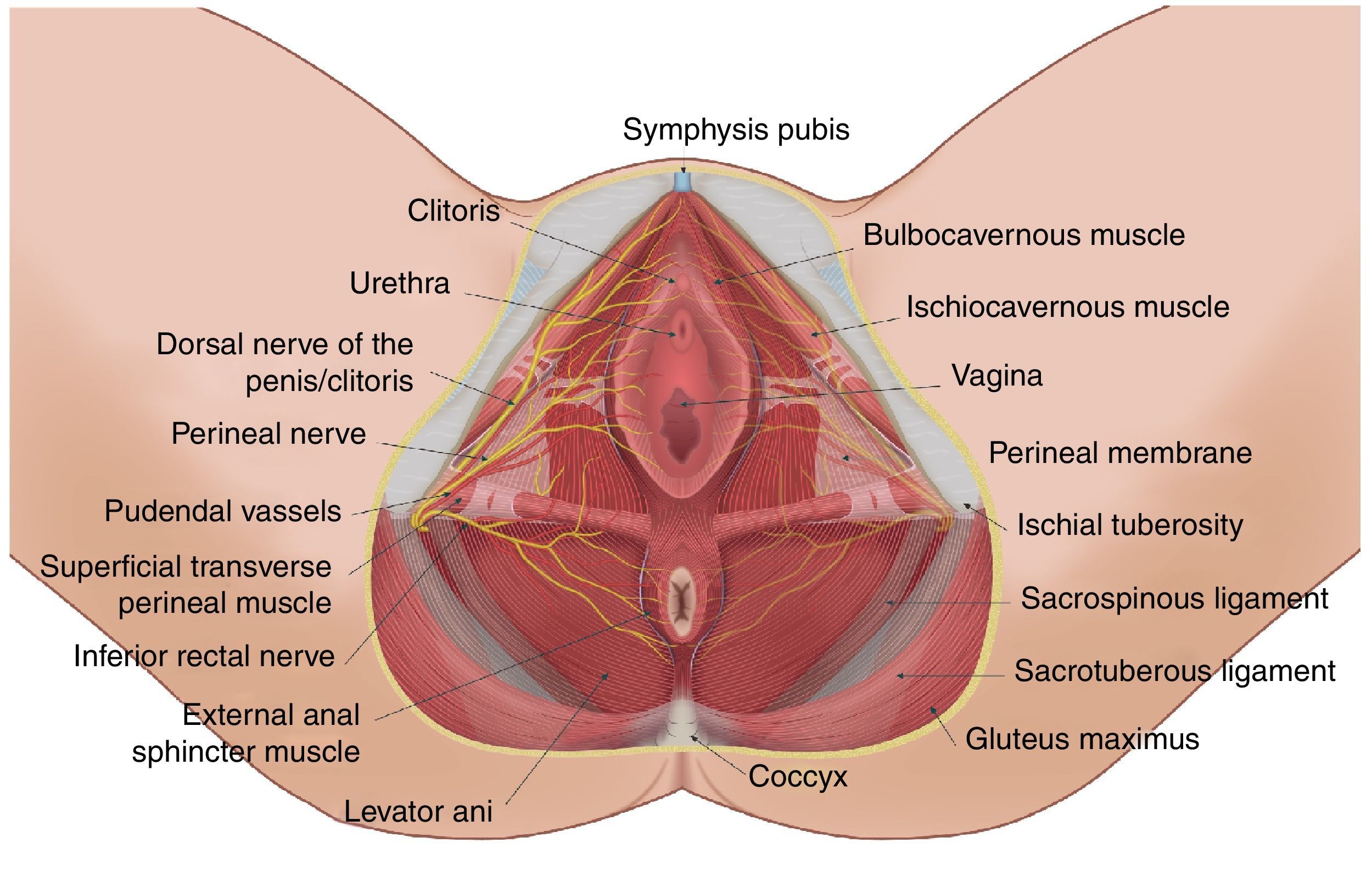
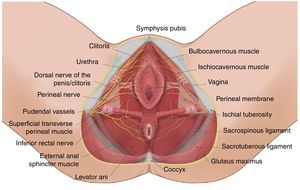
Three nerve branches have been described: the inferior rectal branch, the perineal branch and the dorsal branch of the penis/clitoris. The perineal branch divides into the superficial and deep branches, and the former divides into the medial and posterotaleral of the scrotum/labia.51 Interconnections between the perineal and rectal branches and the posterior femorocutaneous nerve are frequent.52
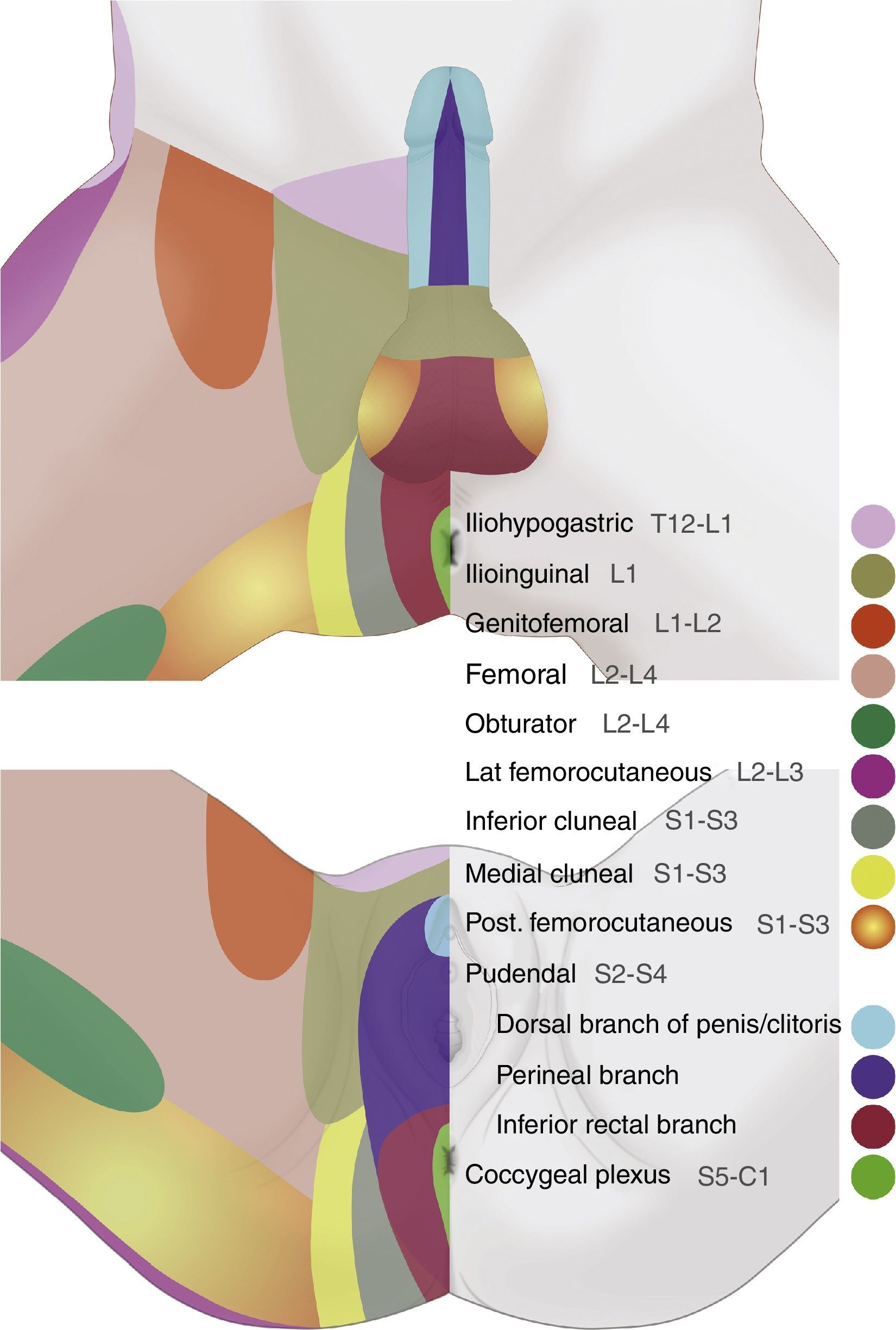
It is important to highlight their functional role in micturition, defecation, erection, ejaculation and childbirth.14,38,41,53Fig. 2 illustrates the dermal distribution territories of the nerves of the genital area.
Perineal dermatomes showing the dermal distribution territories of the iliohypogastric, ilioinguinal, genitofemoral, femoral, pudendal, inferior cluneal, obturator, posterior femorocutaneous, lateral femorocutaneous nerves, and the coccygeal plexus, which may present frequent anatomic variations and interconnections.
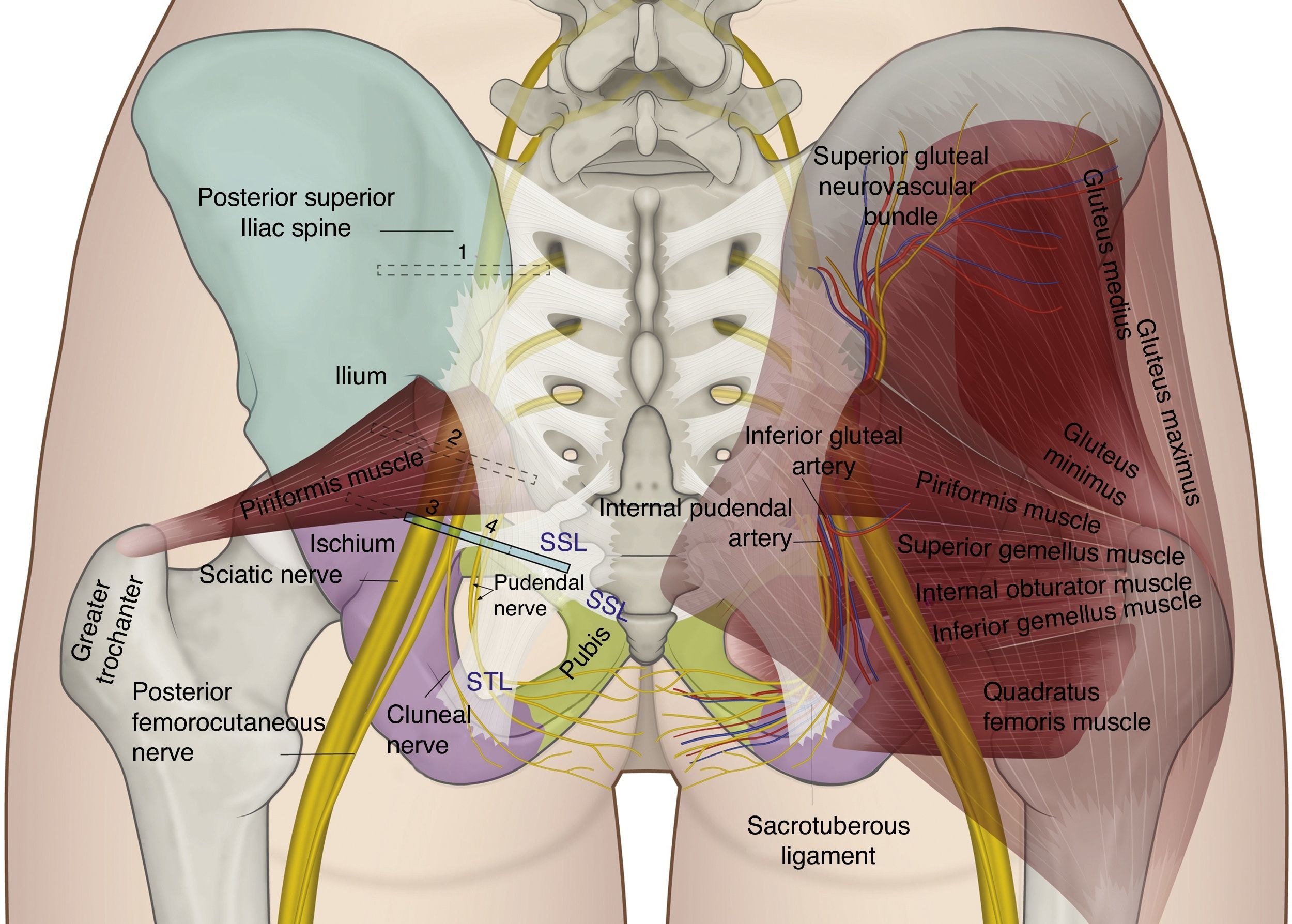
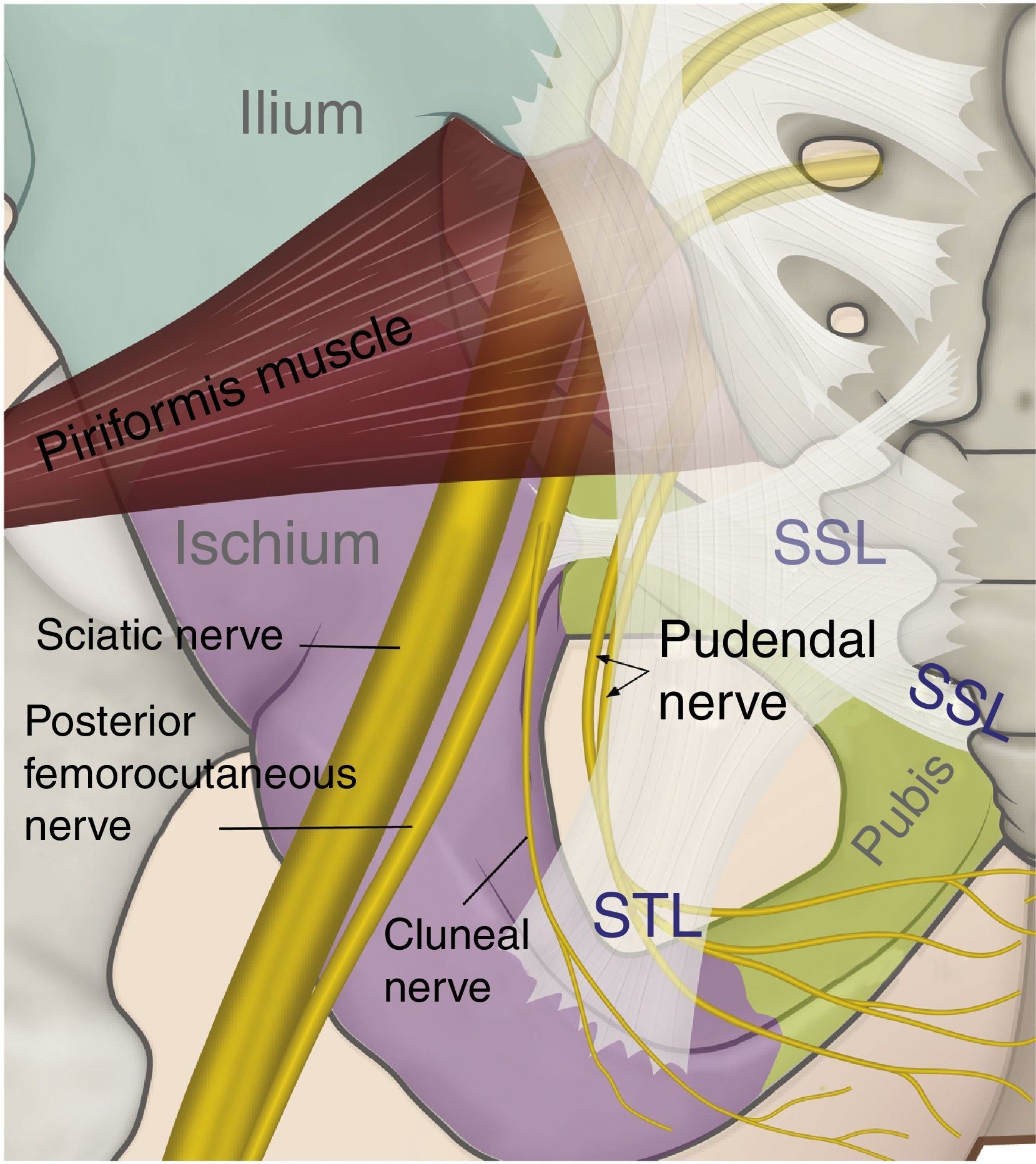
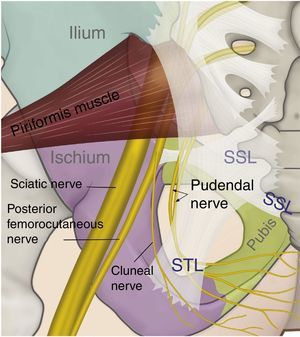
The perineal nerve emerges from the pelvis through the greater sciatic foramen in a caudal course towards the piriformis muscle and the sciatic nerve. Later, it re-enters the pelvis through the lesser sciatic foramen, dorsal to the sacrospinous ligament and ventral to the sacrotuberous ligament.8,35,41,44,54–57 It is in the interligamentous portion of its course where compressive nerve pathologies may be frequently found (see Figs. 3 and 4).
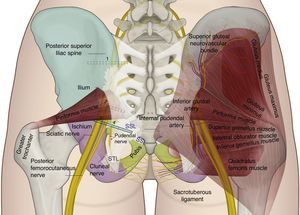
Gluteal anatomy and recommended position for the ultrasound transducer for assessment: (1) at the level of the postero-superior iliac spine; (2) at the level of the greater sciatic foramen; (3) at the level of the ischial spine; and (4) medial to the ischial spine.
In the anatomic descriptions by doctors Gabrielli and Olave,43 the pudendal nerve is shown to be present either as a single trunk (53.3%), as two trunks (36.7%) or as three trunks (6.7%). Pasuk Mahakkanuk et al.42 found the pudendal nerve as a single trunk (56.2%), two trunks (31.5%) and three trunks (12.3%). In their anatomic assessments, Furtmuller et al.44 found that the perineal and the rectal branches arise from a common trunk most of the time; they also found a common trunk between the dorsal branch of the penis and the perineal branch, but less frequently between the dorsal branch of the penis and the inferior rectal branch, thus forming two and even three trunks from their origin.
In the posterior portion of the ischiorectal fossa, immediately after the sacrospinous ligament, the nerve branches for the first time, giving rise to the inferior rectal nerve, which penetrates the internal fascia of the obturator muscle in order to innervate its anal territory.47,58 Mahakkanukrauh et al. found that, in 21% of cases, the inferior rectal nerve arises independently from the root of S4 without being part of the pudendal trunk.41 The perineal branch penetrates medially into the internal fascia of the obturator muscle, sliding towards the base of the urogenital diaphragm where it divides into its superficial and deep terminal branches. The dorsal branch of the penis/clitoris arises from Alcock's canal38 and continues proximal to the inferior pubic ramus anteriorly; the course through Alcock's canal has been described as one of the most susceptible areas for nerve entrapment. In their work, O’Bichere et al. showed that the dorsal branch of the penis/clitoris may arise directly from S2 in 25% of cases.48
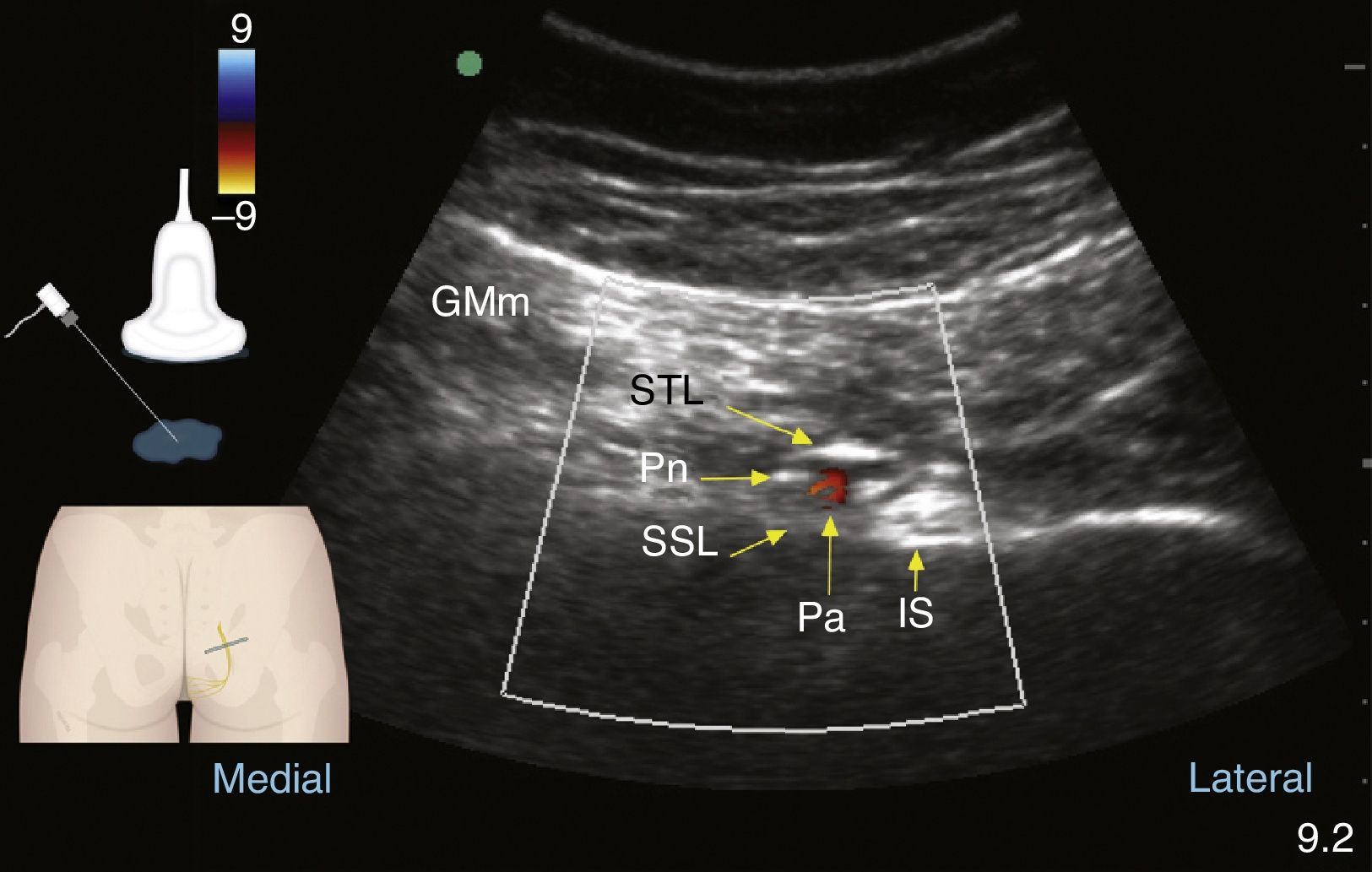
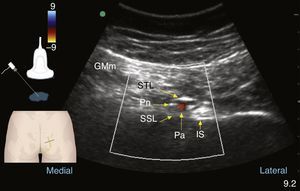
The internal pudendal artery and vein are also found along the course of the pudendal nerve and its branches.41 This is very helpful in identifying the nerve under echo Doppler (see Fig. 5).1,49,59 At the gluteal level, the internal pudendal artery was found lateral to the nerves in 60% of cases, medial in 35% and on either side of the nerves (double), and slightly lateral and ventral to them, in 5% of cases.2,53,57,60,61
TechniquePudendal nerve blocks may be performed through two approaches: anterior/perineal1,2,7,54 or posterior/transgluteal.2,49,56,59,62–65 The perineal approach is used for distal entrapments or for anaesthetic/analgesic purposes in gynaecological, urological or colorectal surgery. The posterior approach has been used in recent years in proximal nerve entrapment syndrome, with a high rate of success in terms of the diagnostic/therapeutic objective, although with a moderate 21.7% risk of sacral plexus blockade.2
Techniques for pudendal nerve blocks described include: 1. anatomical landmarks15; 2. neurostimulation6,66; 3. fluoroscopy49; 4. tomography67–69; and, more recently, blockage guided by ultrasound.1,7,49,59,70–72 We believe that ultrasound is better than other techniques in terms of practical use and results71 and, therefore, we will focus on the sonoanatomic descriptions that enable a refined and reproducible practice in order to increase the frequency of success in terms on the specific goals proposed for each individual patient.60,61
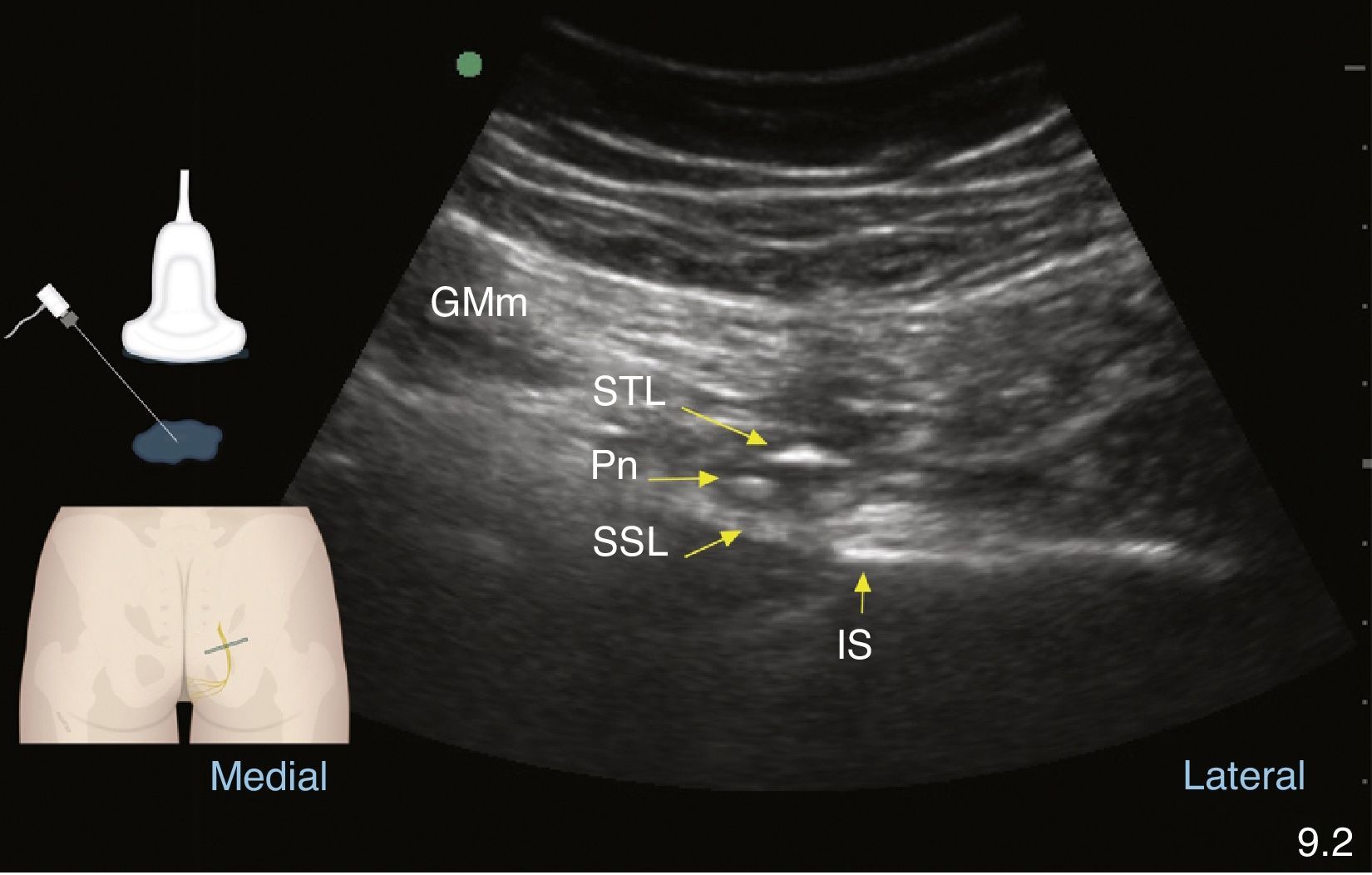
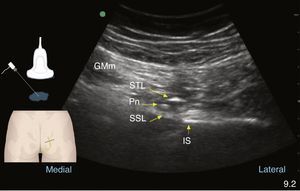
Posterior approachIn 2001, Kovacs et al. described the ultrasound-guided block technique at the level of the ischial spine in cadavers73 and Rofaeel did so in humans in 2008.59 Following the protocol consisting of the informed consent, monitoring, positioning, asepsis, antisepsis, and sedation for all blocks, with the patient on lateral decubitus and the area to be blocked facing upwards and the knees slightly flexed, or in prone position with soft support under the pelvis,65 an identification scan is performed using a linear or convex transducer depending on the patients's constitution. In the average adult patient, the pudendal nerve is located 5–6cm from the skin,59 leading to a more frequent use of the convex transducer, which is placed initially across the proximal gluteal area and then moved obliquely as shown in Fig. 3.
Once the settings are adjusted and the image optimised, the following structures need to be recognised, from proximal to distal: in transducer's position 1, posterosuperior iliac spine; in position 2, greater sciatic foramen, sacral and iliac ridge, piriformis muscle, sacral plexus, superior gluteal artery and, deep down, bowel movement may be recognised. In the transducer's position 3, the ischial spine must be recognised as a straight hyperechoic line with the acoustic shadow deep to it74; the sacrospinous ligament as a continuation of the hyperechoic line of the ischial spine, of lower echogenicity than the bone; the sacrotuberous ligament, superficial and parallel to the sacrospinous ligament, deep to the gluteus maximus. Laterally, it is important to recognise the superior gemellus muscle, the sciatic nerve and the inferior gluteal artery. With the transducer in this position, on the medial edge of the image, attention must be focused on the identification of the internal pudendal artery and the pudendal nerve, the latter being difficult to visualise because of its small size of 3.6mm.73,75 In their work, Bellingham et al. were able to identify the nerve only 57% of the time with an experienced operator49; at this level, it is found in the interfascial plane medial to the pudendal vessels in the majority of cases.65 Once these structures have been recognised, the transducer should be moved in the same angle until the pudendal neurovascular bundle appears in the centre of the ultrasound image and the transducer is in position 4. This is where the puncture will be made either in-plane from medial to lateral, or out-of-plane, as shown in Figs. 6 and 7, using a short-bevel 80–100mmx22G needle according to the patient's constitution. Sensory or motor neurostimulation may be used in the proximity of the nerve in order to determine the presence of paresthesia/motor contraction in the territory of the pudendal nerve. It is important to check for the intensity point at which the stimulus disappears in order to confirm that the needle is not intraneural and, ideally, that intensity must be between 0.2 and 0.3mAmp.2 Once it is in the right position, the drug is administered slowly and in a fragmented manner, in accordance with the stated objective, with frequent aspiration. For chronic pain, a mix of long-acting local anaesthetic and coticosteroid is used in a volume ranging from 4 to 6cc.13,49 Fitchner et al. suggest a slightly more caudal technique at the entry point to Alcock's canal in order to reduce the risk of a sciatic nerve block.2
Colour Doppler ultrasound at the gluteal level: pudendal nerve (Pn), gluteus maximus muscle (GMm), deep to the sacrotuberous ligament (STL) and superficial to the sacrospinous ligament (SSL); the internal pudendal artery (Pa) and the ischial spine are found lateral to these structures.
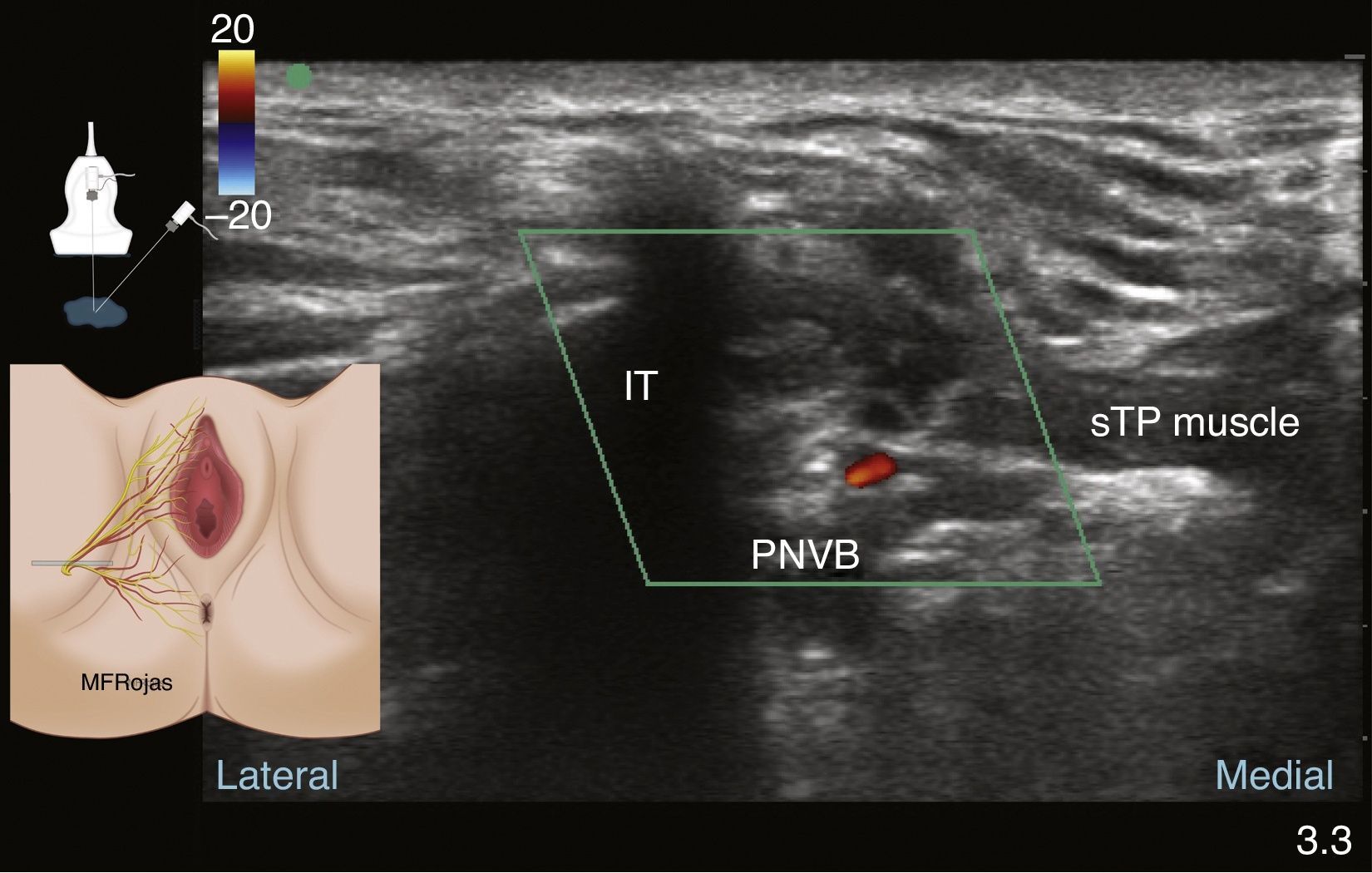
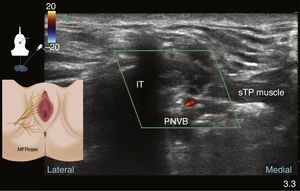
The ultrasound-guided perineal approach was reported by Parras and Blanco in 2013.1 Given that the nerve is very superficial in the perineal area, high or intermediate frequency transducers are recommended.1,7,70 After monitoring with the patient in lithotomy position, sedation, skin asepsis and transducer protection, the transducer is placed lateral to the vulvar/scrotal junction with the rectum, in an oblique sagittal or transverse position, to identify the perineal anatomy and the pudendal neurovascular bundle distally (see Fig. 8).
The transducer must be placed medial to the bony ridge of the ischiopubic ramus of the ischial tuberosity, and attention must be focused on looking for small hyperechoic structures of approximately 3mm76 that might correspond to the branches of the pudendal nerve. Recognition may be impaired because of their small diameter, and colour Doppler must be used for identifying the internal pudendal artery. Once the vascular structure is identified, B mode is selected again and the correlation between the coulour Doppler and the hypoechoic image of the artery is determined. The branches of the pudendal nerve are close to the branching of the artery.1 The neurovascular bundle must be situated in the centre of the screen (see Fig. 9).
The skin is infiltrated with a fine needle in order to reduce the discomfort caused by the penetration of the blunt 22Gx50mm neurostimulation needle. It is advanced in-plane or out-of-plane towards the target. Using a neurostimulation intensity of 0.6–0.4mAmp,9 look for the contraction of the anal sphincter or of the peripheral perineal structures in proximity to the neural structure, in order to confirm that the inferior rectal nerve is close3; safety guidelines must be applied in order to avoid intraneural puncture. Roffaeel et al. showed that the use of neurostimulation is not 100% reliable for the identification of the pudendal nerve59; this may be due perhaps to the low percentage of motor fibres it contains or the small size of its branches. Once the correct position of the needle has been confirmed, a response obtained or the internal pudendal artery seen, gentle aspiration is applied in order to ensure that the tip of needle is not inside the lumen of a blood vessel before starting the slow injection of the local anaesthetic mix, aspirating regularly and watching the ultrasound monitor for the correct distribution of the local anaesthetic; after the infiltration, the injected aqueous solution helps with the recognition of the nerve structures as it enhances echogenic contrast.1
The recommended volume of the selected local anaesthetic mix will depend on the objective of the block, although the recommended volume is usually 0.1 and 0.15ml/kg on each side.77 Long-acting drugs with a high safety profile, such as levobupivacaine, must be considered,1,16 always within the context of multimodal analgesia. The same applies when the concomitant use of corticosteroids is indicated.
Although in these approaches the drug mass used is low, it is advisable to be vigilant of the patient's state of consciousness and haemodynamic status at all the time, and watchful of the local anaesthetic distribution in the ultrasound image.
ComplicationsAlthough the reported rate of complications is low, they may still occur, and they include pudendal nerve injury, vascular injury, intravascular application of the drug mix, muscle weakness in the sciatic nerve territory, muscle pain, urinary or faecal incontinence, and numbness in the pudendal nerve area.16
ConclusionsA deep detailed knowledge of the pudendal nerve anatomy and its variants is essential for the use of imaging-guided regional anaesthesia techniques.
Ultrasound has shown to be of great help in nerve localisation in order to guide and control the application of anaesthetic or analgesic mixes in a more accurate, safe and efficient way. Special attention must be given to overall safety measures, the correct placement of the tip of the needle in relation to the nerve78 in order to reap the benefits of analgesia, and comfort with the procedures in which the block is indicated. Additional clinical studies are required for the evaluation of these promising techniques.
FinancingThe authors declare not having received any form of financial support for this work.
Conflicts of interestThe authors have no disclosures regarding conflict of interest.
We are grateful to doctors Alejandro Corujo, Antonio Bonilla, Ciro Alfonso Rodríguez and José Ariel Giraldo for their interest in reviewing this paper and making contributions.
Please cite this article as: Rojas-Gómez MF, Blanco-Dávila R, Tobar Roa V, Gómez González AM, Ortiz Zableh AM, Ortiz Azuero A. Anestesia regional guiada por ultrasonido en territorio del nervio pudendo. Rev Colomb Anestesiol. 2017;45:200–209.