Orthognathic treatment has assumed an important role in orthodontics and maxillofacial surgery in the last years; however, little has been investigated about this type of treatment.
ObjectivesThe main purpose of this study was to identify major factors and/or predictors associated with postoperative pain (PP) and hospital length of stay (LOS) after orthognathic surgery.
Materials and methods52 patients who underwent orthognathic surgery from 2008 to 2010 at the University Hospital of São Paulo University were investigated. Study variables such as patient characteristics, preoperative, intraoperative and postoperative data were collected. The outcome variables were PP and LOS. Descriptive and analytical statistics was computed for all variables.
Results27.6% of patients had pain in the postoperative period. Lidocaine used in general anesthesia was an associated factor of PP. The overall mean LOS was 2 days; gender, location of procedure, type and duration of anesthesia were identified as probable predisposing factors. There was a significant correlation between anesthesia time and discharge. Anesthesia variables were more predictably related with postoperative pain and hospitalization time. Location of orthognathic procedure, however, was an important surgical variable that influenced in LOS.
ConclusionsIntravenous lidocaine boluses used during general anesthesia were associated with PP. Male patients, single-jaw surgery, inhalational anesthesia and duration of anesthesia were predisposing factors that improve LOS.
la cirurgía ortognática ha asumido un papel importante en la ortodoncia y en la cirugía maxilofacial en los últimos años. Sin embargo, se ha investigado poco sobre este tipo de tratamiento.
Objetivosel objetivo principal de este estudio fue identificar los principales factores o predictores asociados con el dolor posoperatorio (DP) y el tiempo de internación (TI) después de la cirugía ortognática.
Materiales y métodosfueron estudiados 52 pacientes que se sometieron a cirugía ortognática (2008 - 2010) en el Hospital Universitario de la Universidad de São Paulo. Se recolectaron variables de estudio tales como características de los pacientes y datos perioperatorios. Estadística descriptiva y analítica se calculó para todas las variables.
Resultadosel 27,6% de los pacientes presentaron dolor en el posoperatorio. La lidocaína utilizada en la anestesia general fue un factor asociado del DP. El TI medio global fue de 2 días. El género, la localización del procedimiento, el tipo y la duración de la anestesia se identificaron como factores predisponentes probables. Hubo una correlación significativa entre el tiempo de anestesia y de descarga. Las variables de anestesia podían predecirse más cuando estaban relacionadas con el DP y el TI. La localización de la cirurgía ortognática, sin embargo, fue una variable quirúrgico importante que influyó en lo TI.
Conclusionesla lidocaína intravenosa en bolo utilizada durante la anestesia general se asoció con el DP. Los pacientes varones, la cirugía sobre una sola mandíbula, la anestesia inhalatoria y la duración de la anestesia fueron factores predisponentes que prolongaron el TI.
Orthognathic treatment has assumed an important role in orthodontics and maxillofacial surgery over the past 3–4 decades, with esthetic, functional and social impact on the quality of life of patients.1 However, little has been investigated whether clinical practice features have affected variables such as postoperative pain, duration of inpatient stay or chance of requiring high level nursing (sub acute care). These issues are clearly important when orthognathic treatment is done in a publicly funded health care system as they influence the use of resources. Improved knowledge in this field would increase the ability of public health systems to plan their provision of these services and allocate resources appropriately.2
Reduction of postoperative pain (PP) and of length of stay (LOS) after surgery can result in improved allocation and use of health care resources and a substantial reduction in the cost of health care delivery. Although a number of reports have attempted to identify patient characteristics and perioperative adverse events that correlate with pain and prolonged hospital stay, there is a paucity of published papers focused on PP or LOS after orthognathic surgery.
A better understanding of the variables affecting PP and LOS may allow surgeons to assess the management of patients undergoing orthognathic surgery, and hence improve patient care and discharge planning.3
The overall purpose of this study was to estimate the postoperative pain (PP) and the hospital length of stay (LOS) after orthognathic surgery in a large series of patients. The specific aims of this study were to identify major factors associated with PP and LOS, and to determine predictors of PP and prolonged LOS after orthognathic surgery.
MethodsInvestigators evaluated clinical records from subjects who underwent orthognathic surgery from 2008 to 2010, in a retrospective cohort study. A total of 67 patients were admitted for surgical treatment in the Department of Oral and Maxillofacial Surgery. Fifty-two patients (32 females, 20 males) who underwent orthognathic surgery were selected. Patient age ranged from 16 to 63 years (average age 29).
Subjects included in the sample had congenital or acquired skeletal deformities corrected using conventional orthognathic operations. Subjects undergoing distraction osteogenesis were excluded. This study was reviewed and approved by the Ethics Committee of the University Hospital.
Study variablesStudy variables were grouped into the following sets: patient characteristics, preoperative, intraoperative and postoperative. Patient variables were age, sex, and body mass index (BMI). Preoperative variables include ASA classification, medical history, acquired habits and physiological data.
The intraoperative variables were divided into subgroups surgical and anesthesia. Surgical subgroup variables include location, procedure type, use of segmental maxillary osteotomies, whether bone grafting or ancillary procedures were performed, and duration of operation. Location was categorized as mandibular, maxillary, or bimaxillary cases. Procedure types included Le Fort I, bilateral sagittal split osteotomy (BSSO) or vertical ramus osteotomy (VRO) and surgically assisted palatal expansion. In the setting of Le Fort osteotomies, the number of segments was recorded as 1, 2, or 3 pieces. Anesthesia subgroup variables were anesthesia method, anesthetic agents and supplementary medication. The anesthesia method was categorized as normotensive or hypotensive anesthesia (reduction of systolic pressure to 80–90mmHg, or mean arterial pressure of 50–60mmHg or reduction of 30% of mean arterial pressure of baseline).4 Anesthetic agents such as local anesthetics, inhaled general anesthetic agents, intravenous non-opioid anesthetic agents, intravenous opioid analgesic agents, and reversal agents were noted, as well as supplementary medication (perioperative steroid use, anti-inflammatory or analgesic prescription).
Postoperative adverse events were collected and included pain, postoperative nausea and vomiting (PONV), bleeding, superficial and deep wound infection, wound dehiscence and other. Patients were routinely medicated with intravenous nonsteroidal anti-inflammatory drugs (Ketoprofen 100mg or Ketorolac 30mg every 12h), corticosteroid (hydrocortisone 100mg or dexamethasone 4mg every 12h) and dipyrone (2g every 6h). In postoperative period, patients were evaluated with visual analog scale (VAS) pain scores during 24h. If patients recorded VAS>5, tramadol (100mg every 6h) was used as rescue medication.
PredictorsThe outcome variables were PP and LOS. PP was categorized as yes/no response and duration of PP in days. LOS was computed as the time interval (in days) between discharge from the operating room recorded on the nurse's operating room note and the time at which discharge orders were signed. Variables associated with PP and duration of LOS were considered as primary predictor variables.
The hospital discharge criteria used were normal ambulation and mental status, absence of nausea and vomiting, minimal pain controlled with oral analgesics, no surgical bleeding, capacity of fluid intake, presence of diuresis and presence of an adult escort.5
Data analysesDescriptive statistics was computed for each variable. Pearson Chi-Square test and Fisher's exact test were used to identify variables associated with PP and duration of LOS. Associations among variables, PP and LOS were tested with the Pearson correlation test. The level of statistical significance was set at p ≤0.05. Statistical analysis was performed using Minitab Statistical Software for Windows version 15.0 (Minitab Inc, USA).
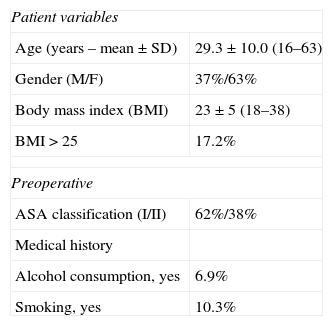
ResultsFifty-two patients (32 females, 20 males) who underwent orthognathic surgery were studied. The demographic data of the sample are summarized in Table 1. Most patients (51.7%) were healthy or without any preoperative medical compromises; 10.3% had a cardiovascular disease, 13.8% had a respiratory disorder and 17.2% had some other disorders.
Demographic data.
| Patient variables | |
| Age (years – mean±SD) | 29.3±10.0 (16–63) |
| Gender (M/F) | 37%/63% |
| Body mass index (BMI) | 23±5 (18–38) |
| BMI>25 | 17.2% |
| Preoperative | |
| ASA classification (I/II) | 62%/38% |
| Medical history | |
| Alcohol consumption, yes | 6.9% |
| Smoking, yes | 10.3% |
SD – standard deviation, M/F – male/female, BMI – body mass index, ASA – American Society of Anesthesiologists.
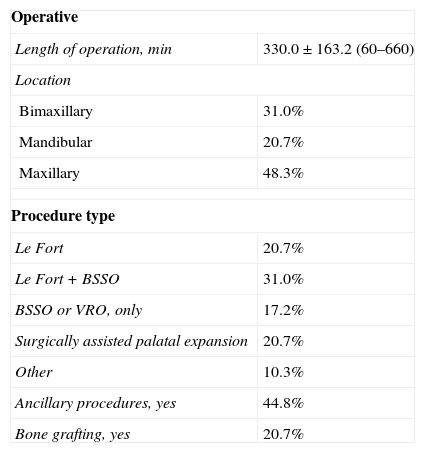
The surgical procedure types and duration of surgery are summarized in Table 2. Mean length of operation was 330.0±163.2min. The distribution of the different operations is shown in Table 1. Bimaxillary osteotomies were performed in 31% of patients. Le Fort and/or BSSO were the most frequent type of procedure, followed by surgically assisted palatal expansion. Ancillary procedures included third molar extraction, septoplasty, genioplasty and coronoidectomy. Bone grafting materials used were polyethylene implants, hydroxyapatite and autogenous bone. Postoperative nausea and vomiting was the most frequent adverse event; bleeding was also observed.
Surgical procedure types and duration of surgery.
| Operative | |
| Length of operation, min | 330.0±163.2 (60–660) |
| Location | |
| Bimaxillary | 31.0% |
| Mandibular | 20.7% |
| Maxillary | 48.3% |
| Procedure type | |
| Le Fort | 20.7% |
| Le Fort+BSSO | 31.0% |
| BSSO or VRO, only | 17.2% |
| Surgically assisted palatal expansion | 20.7% |
| Other | 10.3% |
| Ancillary procedures, yes | 44.8% |
| Bone grafting, yes | 20.7% |
BSSO – Sagittal Split Osteotomy, VRO – Vertical Ramus Osteotomy.
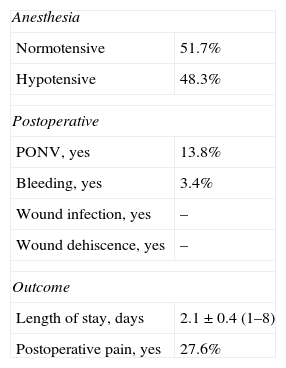
The type of anesthesia, postoperative complications and length of stay are summarized in Table 3.
Type of anesthesia and postoperative complications.
| Anesthesia | |
| Normotensive | 51.7% |
| Hypotensive | 48.3% |
| Postoperative | |
| PONV, yes | 13.8% |
| Bleeding, yes | 3.4% |
| Wound infection, yes | – |
| Wound dehiscence, yes | – |
| Outcome | |
| Length of stay, days | 2.1±0.4 (1–8) |
| Postoperative pain, yes | 27.6% |
PONV – Postoperative Nausea and Vomiting.
About 27.6% of patients undergoing orthognathic surgery had pain in the postoperative period and 62.5% of complainants were male but there was no statistically significant difference (p=0.12).
Intravenous lidocaine boluses of 1.5mg/kg used during general anesthesia (in 32 patients during induction and immediately before extubation) were associated with PP: 87.5% of the patients who received lidocaine had complained of pain (p=0.03).
Length of stay – predictive factorsThe average length of stay was 2.1±0.4 days (range, 1–8 days; median, 1 day). Sixty-two percent (62%) of the patients were discharged the next day of surgery. Approximately twenty-eight percent (28%) were admitted for more than two days; one patient was admitted for longer than five-day period.
Data analysis detected gender, location of procedure, type and duration of anesthesia as probable predisposing factors. Seventy-five percent of patients admitted for longer than two days were male (p=0.008). Bimaxillary procedures demanded shorter hospitalization; single-jaw surgery required longer hospitalization (p=0.008).
Patients undergoing inhalational anesthesia (sevoflurane/isoflurane) stayed longer in hospital (p=0.01) compared with those who underwent total intravenous anesthesia.
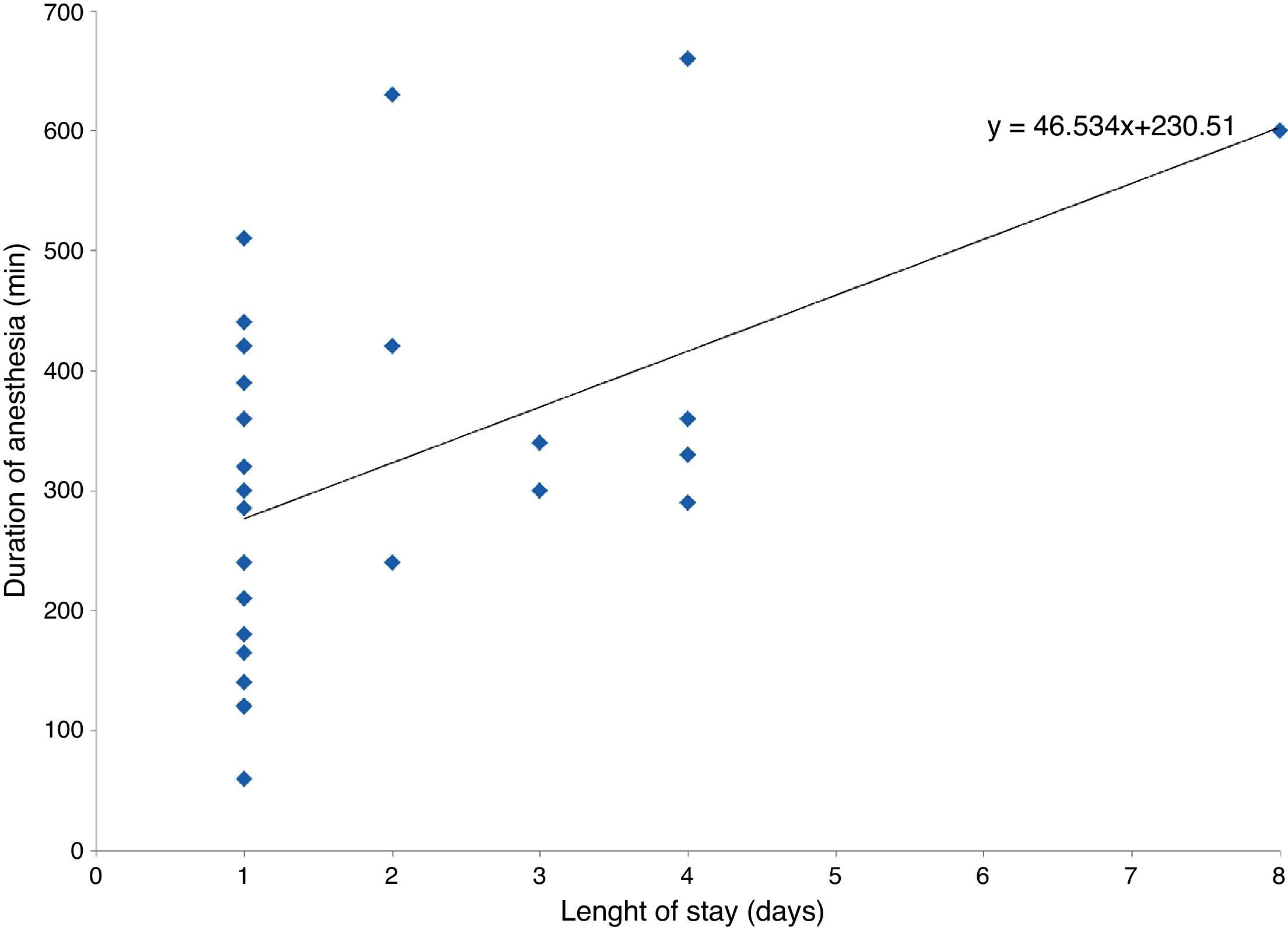
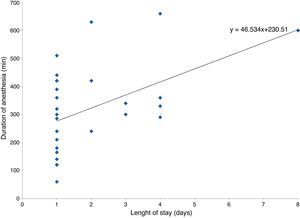
Prolonged anesthesia time significantly correlated with admission time. There was a positive and significant correlation (Pearson r=0.558; p=0.002) between length of stay and duration of general anesthesia (Fig. 1).
DiscussionAs orthognathic surgical procedures have evolved, several aspects of the management of these patients have changed. Many surgical and anesthesia advances allow faster treatment and care, and more selected orthognathic procedures have been performed with improved patient's outcome. Perhaps the most significant advance has been the use of rigid fixation. Rigid fixation facilitates oral hygiene, comfort, and nutrition, but more importantly, airway management that eases concerns over the difficulty patients may have postoperatively with nausea. The development of microsurgical instrumentation, including saws, drills, and retractors, has improved the surgeon's ability to make the precise bony cuts necessary to successfully perform osteotomies. This, in addition to familiarity with the surgical procedures, has allowed surgeons to decrease operating time. Also, the role of systemic steroids in decreasing surgical edema is well documented. This benefit is extremely important in orthognathic surgery because of the proximity of the airway to the surgical site.6,7 Finally, anesthetic management with innovative techniques and better agents contribute to the overall success. Inhalation agents, opioids, and muscle relaxants have been developed with a short half-life to quickly exit the body after surgery, decreasing recovery time. In the majority of orthognathic surgical procedures a number of agents are used to achieve controlled, modified hypotension. Inducing hypotension has the effect of decreasing blood loss and lessening the fluid replacement needs.8–12 Both increase the likelihood of early discharge.3,6,7
The gender distribution of this patient population was typical for orthognathic surgery patients and those suffering from TMJ problems in general. Women more often had pain problems and cosmetic concerns, and they generally seemed to seek help for these problems more actively than did men. The reasons for seeking treatment were functional and pain related in most patients.13
Only patients ASA I and II were included, probably because this type of surgery was more frequently performed in younger patients.
Postoperative pain and complicationsMost patients with postoperative pain were ready to go home after two days. Adequate pain control was not achieved in two patients until the third hospital day. As seen by other authors, patient's age, sex and ethnic origin did not affect the severity of postoperative pain.6,14,15 Niederhagen et al.14 found, however, that postoperative pain intensity was significantly correlated to operating time, the frequency of analgesic demand and the type of surgery (orthognathic surgery>other maxillofacial surgeries).
Some anesthesiologists in our hospital use boluses of intravenous lidocaine to reduce cough reflex of patients during intubation and extubation. This is an individual practice, not standardized in our service. Intravenous lidocaine boluses used in general anesthesia were found to have no beneficial effect on postoperative pain.16,17 Although the analgesic effects of systemic lidocaine have been proven for chronic pain, conflicting results have been achieved in acute pain, such as postoperative pain.16–20 It seems that perioperative lidocaine the development of pronounced central hyperalgesia as abdominal surgeries.18–23 For instance, intravenous lidocaine infusion did not result in any significant reduction in visual analogic scale pain scores or postoperative analgesic requirements in patients undergoing tonsillectomy or in patients undergoing surgical procedures with bone and cartilage trauma as in orthopedic or cardiac surgeries.18,22
Some patients had nausea and vomiting after the first postoperative day but required no prolonged hospital admission. Postoperative nausea with or without vomiting can be minimized by reducing anesthesia time and use of inhalation anesthetics.6
There were no intraoperative transfusions, but there were cases of bleeding and epistaxis. Although bleeding complications are not unique to orthognathic surgery, the consequences can be severe. Surgical planning and a thorough medical history are paramount in avoiding such complications.6
Length of stayThe mean LOS for all procedures was 2 days. This value falls within the lower end of the range of 1.2–8.5 days reported in the literature for patients undergoing orthognathic surgery.2,3,6,13,24–27
From 1975—when Tornes and Lyberg24 found that average hospital stay was 8.5 days for surgical correction of mandibular prognathism—to present time, literature shows that there was a significant reduction over time, which was almost certainly the result of improved surgical and anesthetic techniques, as well as the increase in the use of rigid intermaxillary fixation (IMF) and perioperative steroids.2,3 In Brazil, public data from 2008 to 2011 showed that the mean inpatient stay was 3 days.28
Based on the results, male gender, procedure type, use of inhalational anesthesia and increased duration of anesthesia were associated with increased LOS.
Huamán et al. also found an association between gender and LOS; however, in their sample, female gender was associated with an increased LOS.3
Procedure type was commonly associated with LOS, as seen in Lombardo et al.,26 Lupori et al.,6 and Huamán et al.3; they all reported the longest LOS in bimaxillary procedures, followed by single jaw procedures. Our findings, however, were similar to Panula et al.,13 who, unexpectedly, found longer LOS in patients with single-jaw maxillary discrepancies compared with those with bimaxillary discrepancies. We conjecture that the longest hospitalization in single-jaw surgery is linked to the type of anesthesia selected for these procedures (inhalational anesthesia).
Patients undergoing inhalational anesthesia stayed longer in hospital (p=0.01) compared with those who underwent total intravenous anesthesia. Typically, the total intravenous anesthesia technique has faster recovery than the inhalational anesthesia technique.29 A systematic review on postoperative recovery and complications using different anesthetic techniques showed no significant difference in the early recovery between the intravenous anesthesia (propofol) and inhalational anesthesia (sevoflurane), but with significant heterogeneity. The time to home discharge, however, was earlier with propofol compared with sevoflurane; also, the postoperative complications, including PONV, were significantly greater with sevoflurane.30 Above results may explain the greater length of stay that was seen in the inhalational technique.
There was a significant correlation between anesthesia time and discharge home or admission for observation.31 The average duration of anesthesia was 330min; when the anesthesia time was greater than 5h, mean LOS was 3 days. Lupori et al.4 and Huamán et al.3 have also determined that increased duration of anesthesia resulted in increased frequency of hospital admissions.
Retrospective studies are important to improve management variables which can affect the success of orthognathic surgery. Enhancement of maxillofacial surgery procedures as the sagittal split osteotomy as hospital costs are decreased.7,27
The major limitation of this study rests in its retrospective nature and the small number of patients analyzed. In our study, there were no hospital readmissions despite the longer duration of anesthesia procedure. The inclusion of patients classified as ASA I and II can probably explain this result, as well as the low mean age of our patients. The results of other studies suggest that patients older than 40 years have longer hospital stays and an increased risk of complications and readmissions.32
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
FundingThe authors have not received any funding for producing this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Shinagawa A, Melhem FE, de Campos AC, Cicarelli DD, Frerichs E. Predictores de dolor y tiempo de internación prolongado tras cirugía ortognática: estudio de cohorte retrospectivo. Rev Colomb Anestesiol. 2015;43:129–135.