Inserting a catheter into the epidural space is an anesthetic technique, not exempt from complications. Catheter knotting and retention are rare complications.
Clinical findings, diagnostic evaluation and interventionsTwo cases of epidural catheter-associated complications are discussed. The first was due to the development of a spontaneous knot and the second due to retention and then rupture; both cases required surgical removal.
ConclusionTo prevent these potential complications, refrain from passing excessive catheter length and do not leave more than 5cm of catheter into the epidural space. If a catheter cannot be easily removed, try using several maneuvers and if these fail or there is any pain or paresthesia, diagnostic imaging is required to locate the catheter and request neurosurgery support.
La inserción de un catéter en el espacio epidural es una técnica anestésica que no está exenta de complicaciones. El anudamiento y la retención de un catéter son complicaciones poco frecuentes.
Hallazgos clínicos, evaluación diagnóstica e intervencionesPresentamos dos casos de complicaciones asociadas al catéter epidural. El primero debido a la formación de un nudo espontaneo y el segundo por retención y posterior ruptura. Los dos casos requieron extracción quirúrgica.
ConclusiónPara evitar estas posibles complicaciones no pasar en exceso el catéter y no dejar más de 5cm del catéter en el espacio epidural. Si un catéter no puede ser fácilmente retirado se pueden intentar extracción de este usando varias maniobras, si estas son infructuosas o si hay dolor o parestesias, se debe ubicar el catéter con imágenes diagnósticas y solicitar apoyo de neurocirugía.
Epidural anesthesia is a widely used technique that consists in the neural block of thoracic, lumbar and/or sacral segments. According to the indication, local anesthetics are administered into the epidural space with a single injection or preferably via a catheter,1 with a test dose beforehand.2 A catheter insertion in the epidural space entails the potential risk injuring the dura mater, development of hematomas, abscesses, neurological injury, or catheter misplacement.3 Knotting of an epidural catheter is a rare complication.4 An epidural catheter retention without knotting is even rarer.5
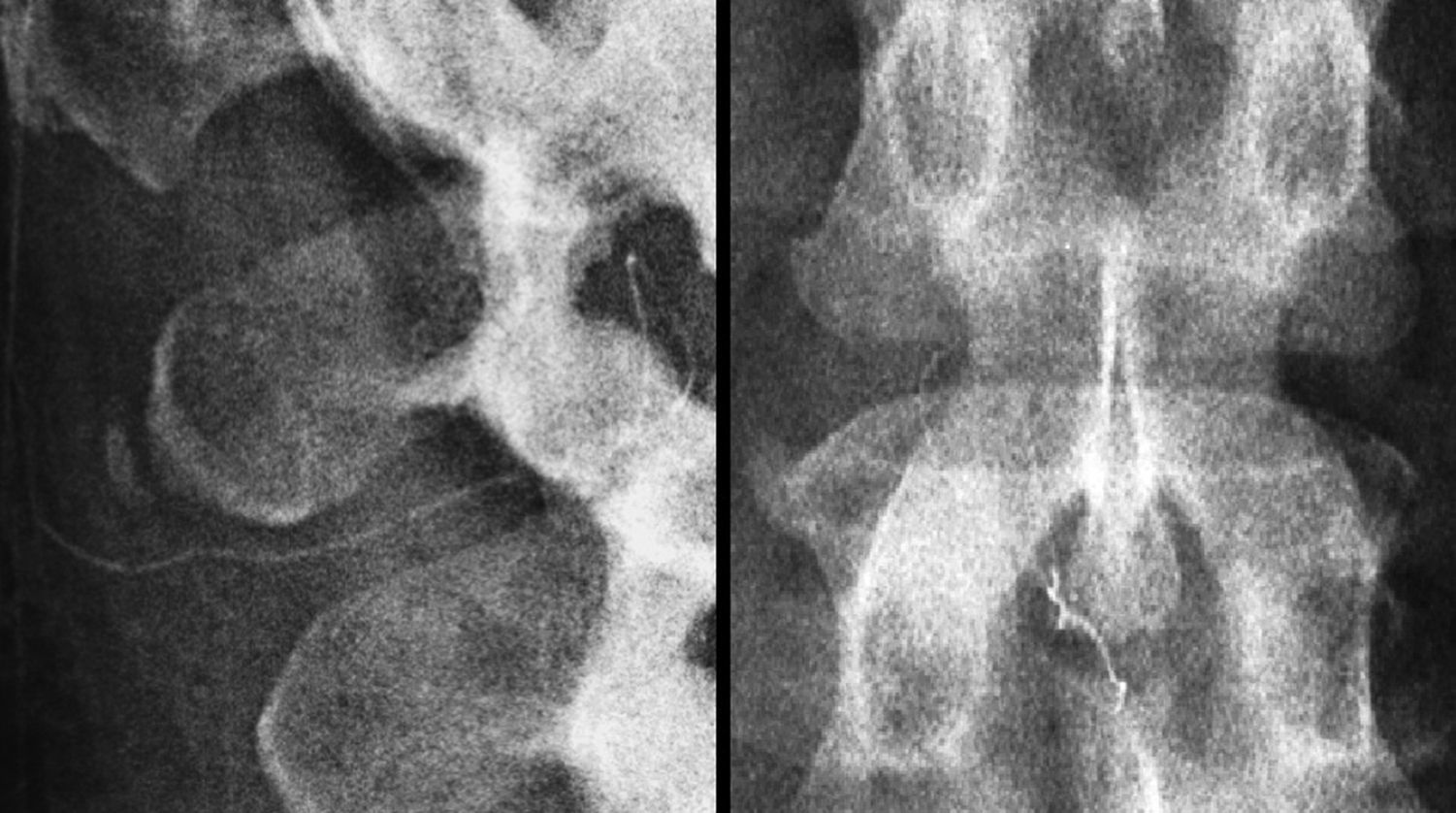
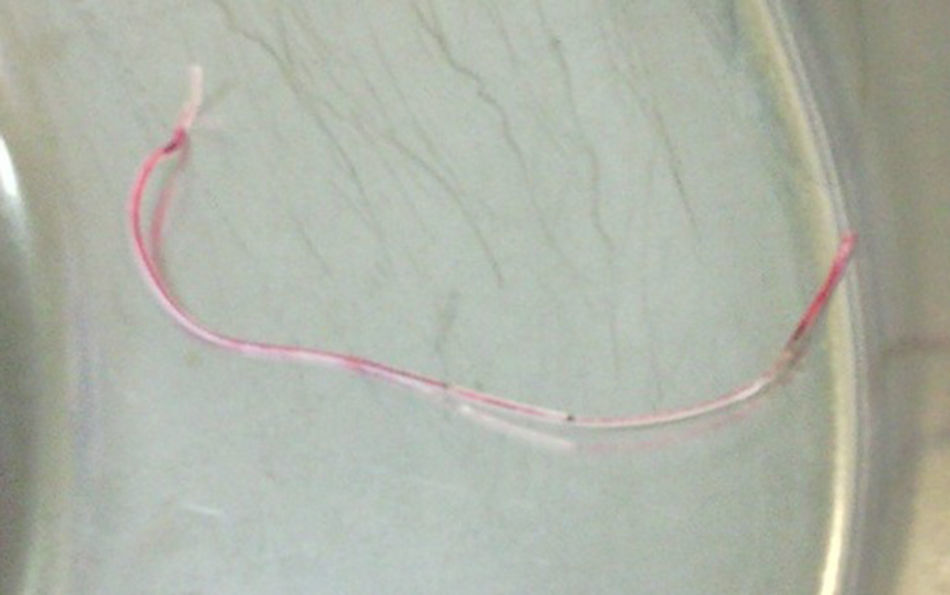
Clinical case 1A 25-year-old woman, housewife, mestizo, with unremarkable family history, denies allergies or toxic substance abuse. She had a diagnosis of Bartholin's gland abscess and was scheduled for drainage. Blood and coagulation time tests were normal. The anesthetic technique selected was epidural block. Using non-invasive monitoring in the OR, and a left lateral decubitus approach for the L2-L3 lumbar space with Tuohy No 18 needle and the loss of resistance with air technique the epidural space was localized 4cm away. A test dose of 3ml of 2% lidocaine was administered, with no changes in the physiological variables, so the rest of the dose was injected after 1min, administering 50μg of fentanyl, upon introducing the catheter to the 14cm mark. At the end of the procedure the patient was moved to a left lateral decubitus position for catheter removal, but there was a strong resistance and an anchoring sensation with a skin lump when pulling the catheter (Fig. 1). Three anesthesiologists made several attempts, with the patient in various positions, but it was impossible to remove the catheter. Due to the suspicion of catheter knotting, a neurosurgeon was consulted. During a second surgical phase and under local anesthesia, the neurosurgeon followed the catheter trajectory, dissected the tissues down to the ligamentum flavum, and pulling softly and consistently managed to remove the catheter; a knot was found at the catheter tip (Fig. 2). The patient was then taken to the recovery room and once the anesthetic effect cleared, she was transferred to her room where she stayed for 24h to continue with the administration of antibiotics and Ciprofloxacin 400mg IV every 12h. The patient experienced no parestesias, pain or any other symptoms. She was discharged 24h later, with oral antibiotic management and Ciprofloxacin and a gynecology control appointment in seven days time.
A 38-year-old woman, housewife, mestizo, 34 weeks into pregnancy. Her GyOb history indicated 5th gestation, 2 deliveries, 1 C-section, 1 miscarriage, with no remarkable family history, no previous chronic degenerative diseases, allergies, or toxic substance abuse. The patient required a cesarean section because she was undergoing active labor and the baby was in a breech presentation. The blood and coagulation time tests were normal. Epidural block was the anesthetic technique chosen. Non-invasive monitoring was used in the OR with the patient in the left lateral decubitus position to approach the L2-L3 lumbar space using Tuohy No 18 needle, and with the loss of resistance with air technique, the epidural space was localized 5cm away. A test dose of 3ml of 2% lidocaine was administered, with no changes in the physiological variables; the 300mg of lidocaine dose was completed after one minute through the needle and then the epidural catheter was inserted, down to the 20cm mark. Then the needle was removed and the catheter was pulled out; however, when the 13cm mark was reached, resistance was felt that prevented the catheter withdrawal. In view of the difficulty, the removal procedure was interrupted and the catheter was fixed to the skin. With the dose of lidocaine administered, a T5 sensory level was obtained and the surgery was performed uneventfully. When the procedure was completed, the patient was turned to the left lateral decubitus position, a second anesthesiologist applied a constant and forceful traction to the catheter but the catheter broke. The patient expressed no signs of parestesis or pain. Plain lumbar spine X-rays were taken that indicated a catheter loop (Fig. 3). The patient was evaluated by neurosurgery and surgical management was recommended. The next day, under general anesthesia and with the patient in the prone position, the neurosurgeon performed a lumbar incision and identified the location of the distal tip of the catheter into the subcutaneous cell tissue. Using a steady pull force, the surgeon was able to remove the catheter (Fig. 4). Once the patient was extubated and tested to make sure that there were no sensory or motor limitations, she remained in the recovery room for 2h and was then transferred to the room. After 24h she was discharged and during that time she experienced no signs of pain or neurological upsets.
Medical literature discussionEpidural anesthesia is not exempt from complications when inserting or removing the catheter. Several causes of tear, breakage, or knotting have been described, including: the amount of force used to insert or remove the catheter, cutting or sectioning the catheter with the tip of the needle when trying to remove it through the Tuohy needle, and catheter inserted too deep into the epidural space, among others.1–6
The actual incidence of epidural catheter knotting is difficult to assess and knot-less catheter retention is even more rare. Based on case reports in the literature, the epidural catheter knotting has been estimated at 0.0015%.4 Most knotted catheters are inserted at the lumbar level, mostly in obstetric patients and the knot develops along the last 3cm of the catheter,5 and has been associated with over 5cm of the catheter's length inserted into the epidural space.6–8
There are very few reports on catheter retention with no knotting. Roma et al. report that out of 19,280 epidural analgesia procedures from January 2000 through July 2007, only two epidural catheters were difficult to remove. The first case was due to a knot and the second one because the catheter was more flexible and tended to stretch and became anchored to the tissue.5
Whenever there is difficulty to remove the catheter, the recommendation is to pull out softly and steadily, with the patient in the same position used to insert the catheter; if this approach fails, try pulling with the patient in different positions and at various angles of lumbar flexion or extension.9 If these measures fail, imaging studies should be performed, such as X-rays with or without contrast medium, CT-scan, or MRI.10,11 After locating the catheter and in the absence of contraindications such as nerve involvement, further attempts to remove the catheter can be made, until it is retrieved or breaks down. Generally speaking, catheter fragments do not cause any injuries or symptoms because these are sterile or inert materials. However, if the fragment is close to the skin, it has the potential of getting infected and if the patient reports any symptoms, surgery is indicated.12
Patient managementDespite Morris's8 recommendations being followed for the removal of a retained epidural catheter, the removal attempts failed and neurosurgery support was required.
Lessons learnedThe particular characteristic of the cases herein discussed is that both epidural catheter complications were associated with inserting the catheter too deep. So a way to avoid these potential complications is to check the distance from the epidural space, not to insert the catheter too deep, and do not leave more than 5cm of catheter into the epidural space.
Patient's viewIn both cases the patients were informed about the risks and complications of the anesthetic technique and the neurosurgeon also educated them on the complications when removing the catheter surgically, as well as of the need to do a laminectomy when appropriate. None of the patients reported any pain or neurological symptoms during the catheter insertion, surgical removal, or thereafter. The length of stay was not extended in either case as a result of timely diagnosis and management.
Informed consentThe informed consent was signed upon informing the patient about the risks and complications of the anesthetic technique, the surgery, and authorization was obtained to report the case. No details are given on the identity of the patients.
FundingNone.
Conflicts of interestNone.
Please cite this article as: Molina-García RA, Muñoz-Martínez AC, Hoyos-Pescador R, De la Torre-Espinosa R. Catéter epidural retenido. Complicación poco frecuente. Reporte de dos casos. Rev Colomb Anestesiol. 2017;45:4–7.