Iatrogenic retroperitoneal haematoma is an infrequent but serious complication of certain surgical procedures.
Case presentationWe present the case of a female who developed retroperitoneal haemorrhage after an intradural lumbar puncture, resulting in multiple-organ failure. The diagnosis and treatment of this complication was more difficult than usual because of the presence of bilateral subclavian artery stenosis.
ConclusionEarly diagnosis and prompt treatment with either conservative or interventional management is essential in order to decrease associated morbidity. Bilateral non-invasive arterial pressure measurements should be routinely performed in all cases, especially in patients with peripheral artery disease.
El hematoma retroperitoneal iatrogénico es una complicación infrecuente pero, en ocasiones, de consecuencias fatales.
Presentación del casoEn este artículo describimos el caso de una mujer que sufrió una hemorragia retroperitoneal secundaria a una punción lumbar intradural con evolución hacia el fallo multiorgánico, agravado en su manejo por la presencia de estenosis bilateral de arterias subclavias que dificultó el diagnóstico y el tratamiento.
ConclusiónUn diagnóstico precoz y certero del hematoma retroperitoneal, unido a las medidas de soporte necesarias y a un abordaje quirúrgico eficiente cuando se requiera, se antojan fundamentales para evitar un desenlace mortal. Por otro lado, la medición de la presión arterial de forma bilateral debe ser una medida rutinaria en todos los pacientes, pero más aún en aquellos casos con enfermedad arterial periférica.
Retroperitoneal haematoma resulting from lumbar puncture was described for the first time in 1950.1 The actual incidence is difficult to determine considering that only isolated case reports are found in the literature. Potential causes have included anaesthetic techniques such as intradural anaesthesia,2 epidural technique, lumbar plexus blocks,3 or ilioinguinal nerve blocks.4 We present a case of severe retroperitoneal haematoma with hypovolemic shock secondary to diagnostic intradural puncture, which posed a serious management challenge given the presence of bilateral subclavian artery stenosis.
Patient informationA 78-year-old female patient with a relevant history of blood hypertension, hypercholesterolemia, hyperuricemia, peripheral vasculopathy with lower limb claudication due to iliofemoral stenosis, and supra-aortic trunk vasculopathy. She had had three episodes of ischaemic attacks in the previous year and was receiving antiplatelet therapy with clopidogrel and concomitant treatment with simvastatin, venlafaxine, pantoprazole, mirtazapine and allopurinol.
She presented to the emergency department with clinical manifestations of dysarthria and intense headache. She was admitted to the neurology service due to the suspicion of a new ischaemic attack episode.
Clinical findingsDue to the onset of fever >38°C, blood samples for culture were made and a diagnostic lumbar puncture was performed using a Quincke 22GA bevelled needle, requiring several attempts.
Immediately afterwards, the patient reported inguinal and left lower limb pain, and went into progressive decline of her general condition with hypotension, poor peripheral perfusion and reduced level of consciousness, leading to her transfer to the ICU.
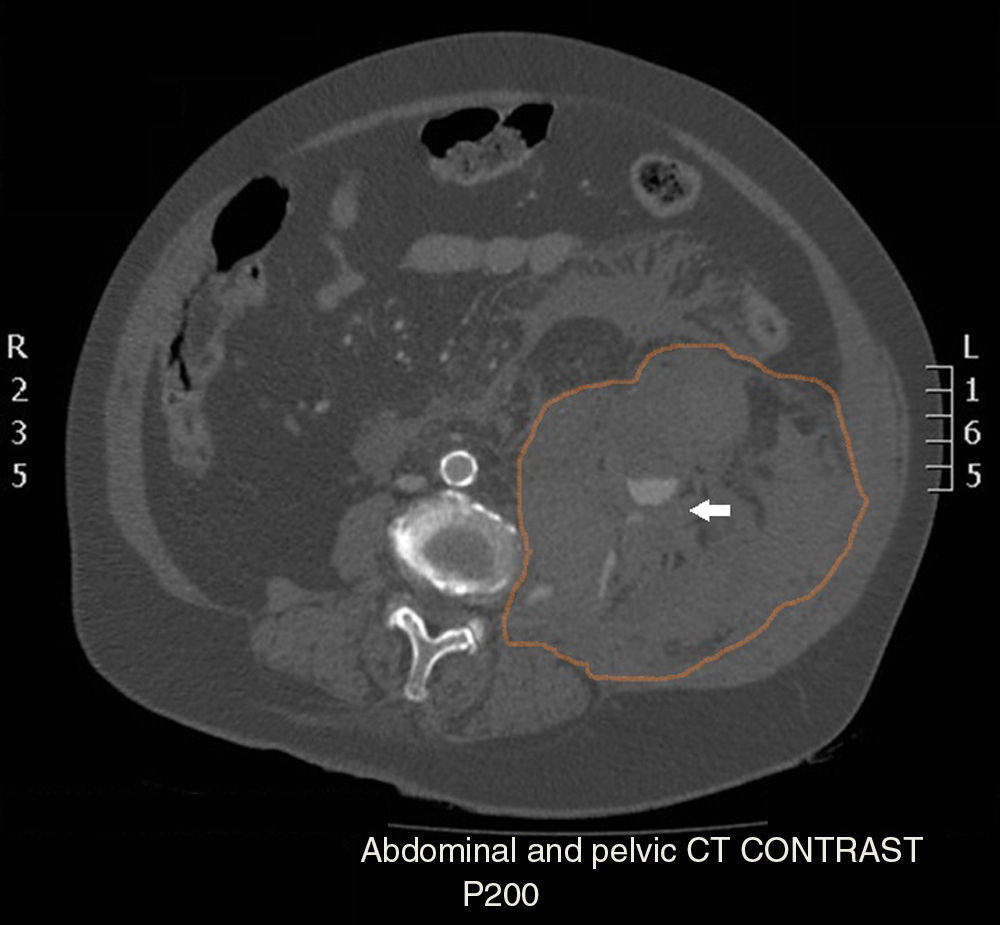
Therapeutic interventionAs soon as the patient arrived at the ICU resuscitation manoeuvres were initiated, consisting of orotracheal intubation, mechanical ventilation, vasoactive drugs, antibiotics, and intensive fluid replacement therapy guided mainly by invasive radial arterial pressure (AP) values. When blood gases confirmed significant acute anaemia an urgent CT scan of the abdomen and pelvis was requested, revealing a significant left retroperitoneal haematoma secondary to the rupture of a lumbar artery at the level of L3 (Fig. 1).
Left retroperitoneal haematoma extending from the anterior and posterior para-renal space to the perisplenic space and the pelvis, with displaced adjacent structures. Presence of free fluid throughout the abdominal cavity. Most of the contour of the retroperitoneal haematoma is outlined in orange. Presence of active bleeding from the lumbar artery marked by the white arrow.
Given the situation, it was decided to proceed with urgent surgery in order to perform arteriography and arterial embolization. Three hours after the puncture, the patient was transferred to the operating room with a diagnosis of haemorrhagic hypovolemic shock, on high-dose vasoactive drugs. After establishing access through the left femoral artery for the arteriography, a very intense femoral beat was observed which was totally inconsistent with the low invasive and non-invasive AP values monitored in both upper limbs. An AP transducer was then placed over the left femoral artery, revealing a significant systolic blood pressure differential of up to 90mmHg between the two peripheral circulations. From that moment on, femoral AP was considered as the real AP. This difference dropped to 40mmHg following the reduction of vasopressor doses and blood product transfusions. Later, once the old clinical record was made available, a suspected bilateral subclavian artery stenosis was found to be the confirmed cause of this differential.
Outcome and follow-upAfter lumbar artery embolization, and once the bleeding was stopped, the patient was transferred back to the ICU in a critical situation with haemodynamic instability and onset after a few hours of myoclonus and oligoanuric renal failure. A brain CT scan was performed 24h later, revealing extensive cerebral ischaemia probably as a result of the severe hypovolemic shock experienced by the patient. In view of the poor prognosis it was decided to limit therapeutic attempts, and the patient died 72h after admission.
DiscussionIatrogenic retroperitoneal haematoma is an infrequent complication, but may result in severe complications, including patient demise. The risk is increased, as was the case in this patient, when there is antiplatelet treatment, intensive anticoagulation, or in patients ≥70 years of age.5 Beside iatrogenic origin, retroperitoneal haematoma may also have a spontaneous onset in certain patients as a result of abnormal coagulation, a diseased organ or retroperitoneal structure, kidney disease being the most frequent.
The clinical presentation varies significantly and, on occasions, the diagnosis is delayed because large quantities of blood may pool in the retroperitoneum before the onset of symptoms. In a retrospective study of patients with retroperitoneal haematoma following cardiac catheterization, the most common symptoms were low, posterior or lateral abdominal pain, diaphoresis, bradycardia, hypotension and anaemia. Such absence of clinical specificity and delayed diagnosis are key determinants of morbidity and mortality.6
There are no specific clinical guidelines for the treatment of retroperitoneal haematoma because the available evidence is based on small case series or isolated cases. There is a need to perform imaging studies like CT scan, or ultrasound if the former is not available, in order to confirm the diagnosis and the size of the haematoma. Depending on the patient's clinical situation, conservative treatment with support therapies must be instituted together with invasive monitoring, intensive fluid replacement therapy, blood transfusion in case of anaemia, and treatment of the coagulopathy if needed. These strategies are usually effective in the majority of cases. In haemodynamically unstable patients, the most appropriate option is surgical treatment with endovascular approach, using arteriography to identify the bleeding site and to perform embolization, reserving open surgery for cases in which the endovascular technique fails.7
Subclavian artery stenosis is characterized by partial or complete blood flow obstruction, the main cause being atherosclerosis. Its incidence is of around 3–4% and it may be as high as 11–18% in patients with peripheral artery disease.8 If is infrequent to find bilateral subclavian artery stenosis,8 but it may cause significant morbidity and produce ischaemic symptoms affecting the upper limbs, the brain, and even the heart. Patients affected with this disease are at a higher risk of coronary artery lesions and cerebrovascular events.
The presence of subclavian artery stenosis produces low AP measurements when AP is measured on the affected side, masking the symptoms and making therapeutic management more challenging.9,10 Routine arterial pressure measurements only on one upper limb may lead to inadequate clinical management in these patients. Hence the importance of emphasizing the need for bilateral AP measurements and, if necessary, in all the extremities, particularly in patients diagnosed with peripheral vascular disease.11
In our patient, there was a clear time correlation between the onset of symptoms of severe retroperitoneal haematoma and the lumbar puncture, ruling out spontaneous haematoma or other causes. CT confirmed the diagnosis and resuscitation measures were initiated in view of the instability, and the patient was transferred to the operating room for endovascular treatment and embolization of the bleeding site. The presence of bilateral subclavian artery stenosis in this patient was a confounding factor since it was not known from the start. The patient was believed to have arterial hypotension refractory to the use of high-dose vasopressors until femoral AP measurements were found to be inconsistent with the radial AP value. The cause of death – a massive cerebral ischaemia – was probably related to the clinical picture of acute haemorrhagic hypovolemic shock with severe anaemia and arterial hypotension suffered by the patient.
To conclude, it is worth highlighting that, in medicine, all invasive techniques may be associated with serious complications. A fast and accurate diagnosis of iatrogenic retroperitoneal haematoma, together with support measures and efficient surgical approach when needed, are essential. The presence of subclavian artery stenosis will result in lower AP values in the upper limb, corresponding to the real systemic values. If its existence in unknown, it may be a serious confounding factor that may lead to the wrong diagnosis and treatment. It is important to emphasize the importance of bilateral AP measurements, especially in patients with evidence of peripheral vascular disease.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingThe authors did not receive sponsorship to undertake this article.
Conflict of interestThe author has no conflicts of interest to declare.
Please cite this article as: Soto-Mesa D, Herrera-Soto A, Bermejo-Álvarez MÁ, Argüelles-Tamargo L. Hematoma retroperitoneal tras punción lumbar diagnóstica. Caso clínico. Rev Colomb Anestesiol. 2016;44:44–47.