The ultrasound is a useful, timely, and accessible tool to guide emergency patient care.
A systematic search was conducted in the following databases: Pubmed, Medline, SciELO, and Lilacs using the keywords ultrasonography, trauma, hemoperitoneum, and abdominal injury.
The main purpose of this review was to provide clear objectives and concepts on how to perform the FAST and FAST extended examinations properly, emphasizing the techniques that should be used and the appropriate ultrasonography windows. Photographs taken by the authors are included.
From this review, it can be concluded that there is enough evidence to recommend performing this procedure, with proven sensitivity and specificity ranging from 73 to 99%.
El ultrasonido es una herramienta útil, oportuna y accesible para orientar el manejo del paciente emergente.
Se realizó una búsqueda sistemática en las siguientes bases de datos: Pubmed, Medline, SciELO, Lilacs. Utilizando como palabras clave: Ultrasonography, Trauma, hemoperitoneum, abdominal injury.
Con los resultados obtenidos mediante esta revisión se pretende entregar conceptos claros sobre los objetivos y forma de realizar de manera apropiada los exámenes: FAST (Focused Assessment with Sonography forTrauma) y FAST extendido, haciendo énfasis en la técnica que se debe utilizar y las ventanas ultrasonográficas indicadas. Se adjunta fotografías realizadas por los autores.
De esta revisión se puede concluir que actualmente hay evidencia suficiente para recomendar la realización de este procedimiento, mostrando una sensibilidad y especificidad que varía entre el 73 al 99%.
The use of ultrasound technology to detect abdominal injury due to trauma was described by Kirstensen1 in 1972. Asher et al.2 reported in 1976 a sensitivity of 80% in the detection of splenic injury in blunt trauma. The use of ultrasounds was then abandoned, but as of 1990, the method has been taken up again specifically for blunt abdominal trauma.3
Since then, multiple authors have written about the topic. Ultrasound is more popular daily due to its availability, easy accessibility, low cost, and due to its lack of ionizing radiation.
The initial motivation to carry out the FAST examination (Focused Assessment with Sonography for Trauma) is the high prevalence of abdominal trauma, which is the third cause of death from trauma in the world, surpassed only by traumatic brain injuries and chest trauma. Furthermore, it is the leading cause of avoidable trauma-related death if it is detected in time.4 The term extended FAST (eFAST) refers to the addition of a chest exam, thus offering a broader spectrum for diagnosing and detecting any possible injuries.
Currently, FAST and eFAST are fundamental in the care of trauma patients. The American College of Emergency Physicians (ACEP) included training for it in its 2008 guidelines, and the American Institute of Ultrasound Medicine (AIUM) also recognizes it as an important aspect of its 2011 guidelines. Currently in Colombia, guidelines for ultrasound use in emergency care have been published by the Asociación Colombiana de Medicina de Emergencias (ACEM), which have in turn been adapted by various emergency care associations in Latin America.
This review will describe the technique used to conduct the FAST and eFAST exams, and will discuss the usage and limitations of the FAST-ABCDE. It will also analyze the interpretation of results and will evaluate its utility in decision-making in different areas of medical practice.
TechniqueWhen initiating the FAST test, the first thing one looks for is the presence of hemoperitoneum; then, after performing the chest exam, the next question to be answered is whether any chest injuries have been found, such as pneumothorax, haemothorax or cardiac tamponade.
To best conduct chest and abdominal evaluations, a low-frequency transducer (3–5Mhz) is required to examine the abdomen and subxifoid window, and a high-frequency transducer is required for the examination of the chest. Not having the latter does not make conducting the examination impossible, though it does partially limit the visualization of the pleura and lung.
When starting the FAST examination, three windows are established: the hepatorenal window at the right superior quadrant, the splenorenal window in the left superior quadrant, and the pelvic window, which is viewed from above the symphisis of the pubis.5,6
When performing the eFAST examination, the subxifoid window is added in order to assess for presence of cardiac taponade, along with the windows in pulmonary apexes to rule out a haemothorax or pneumothorax.
The full examination should not take more than four minutes. In order to detect hemoperitoneum, the bleeding is assumed to have originated from the liver or spleen, as this technique lacks the sensibility to detect injuries in the hollow organs and retroperitoneal bleeding. It is worth noting that the presence of hemoperitoneum in a window is not specifically linked to bleeding in that site. There are some solid organ injuries that can be confidently detected with ultrasound, though this is not the main objective of the FAST exam.
In the ultrasound images, the free abdominal liquid is visualized as an anechoic (black) image, which appears in any of the windows described. The transducers have a position marker, which should always be oriented towards the head or the right side of the patient, depending on the desired type of image. The ultrasound technician should be trained in abdomen software (if this option is available).
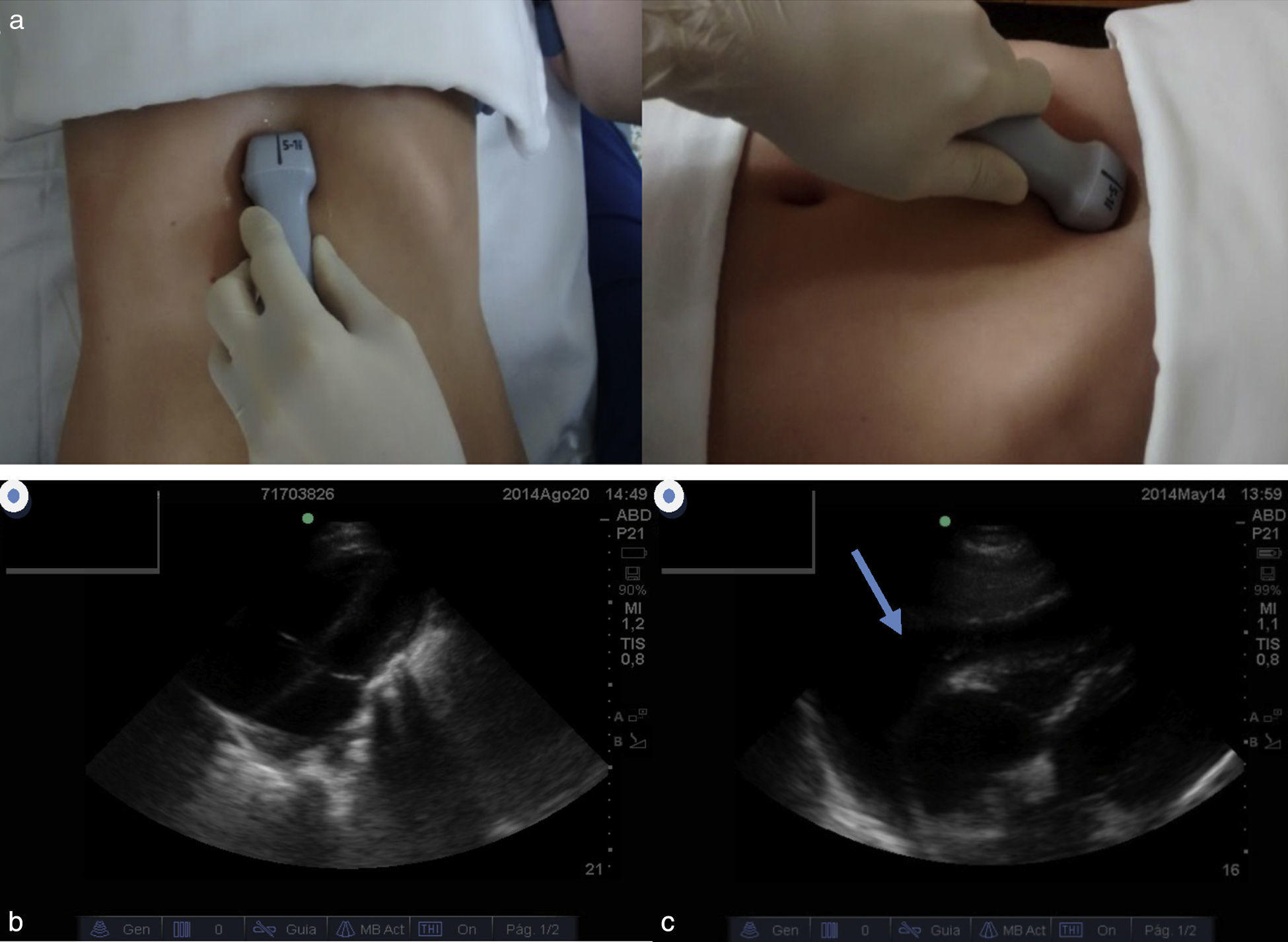
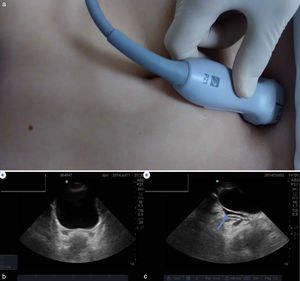
Ultrasonography windowsPericardiac windowThis evaluates the pericardium to detect cardiac taponade, and in the case of circulatory arrest by trauma, looks for the presence of cardiac contractility.
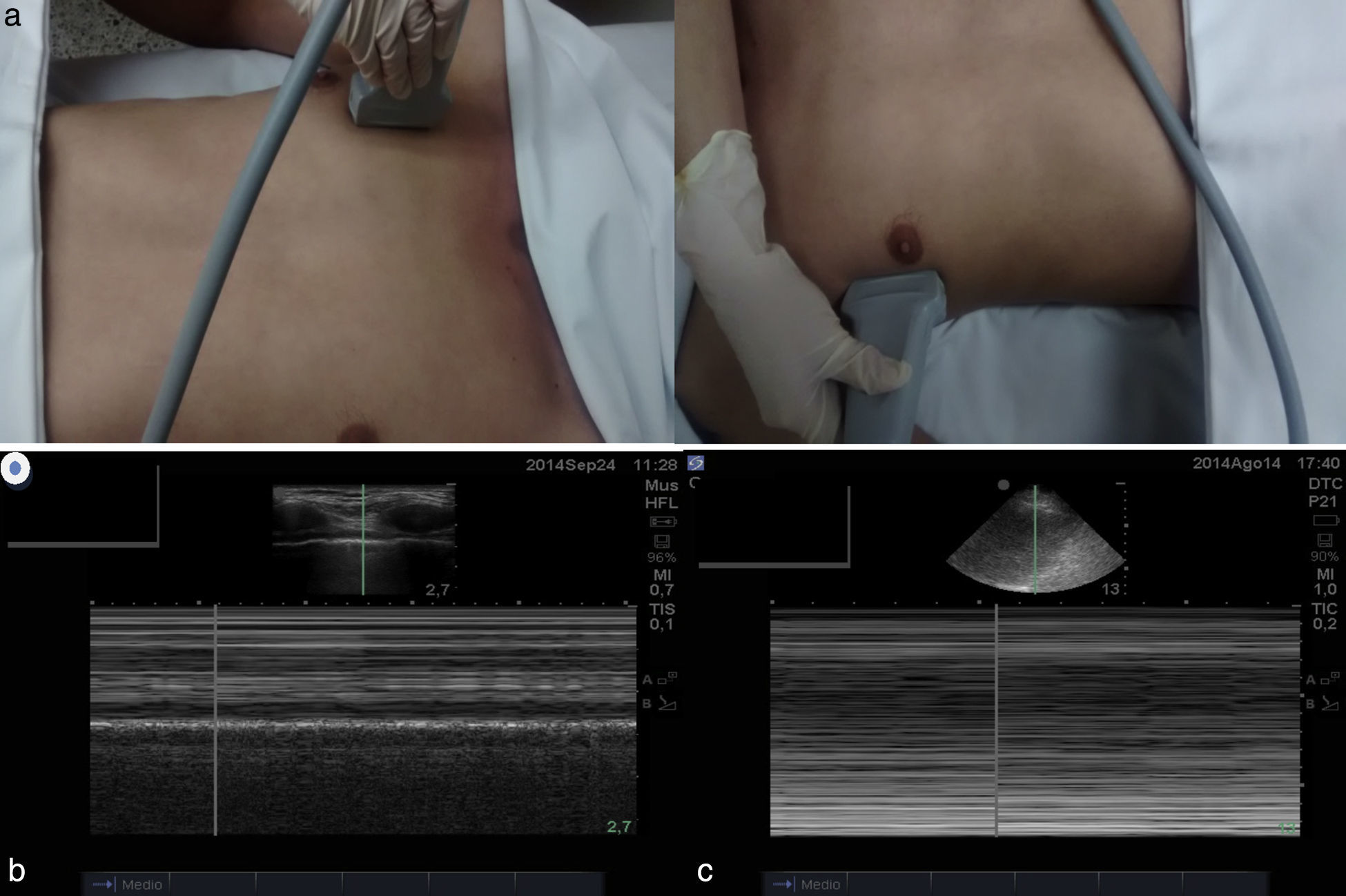
The transducer is positioned at the subxifoid level, using the liver as an acoustic window to obtain the best resolution. The indicator should be positioned on the right side of the patient. In some occasions it is not possible to obtain this image (pain, distension, bad window), so the image should be taken from the middle of the left parasternal axis (Fig. 1a–c).
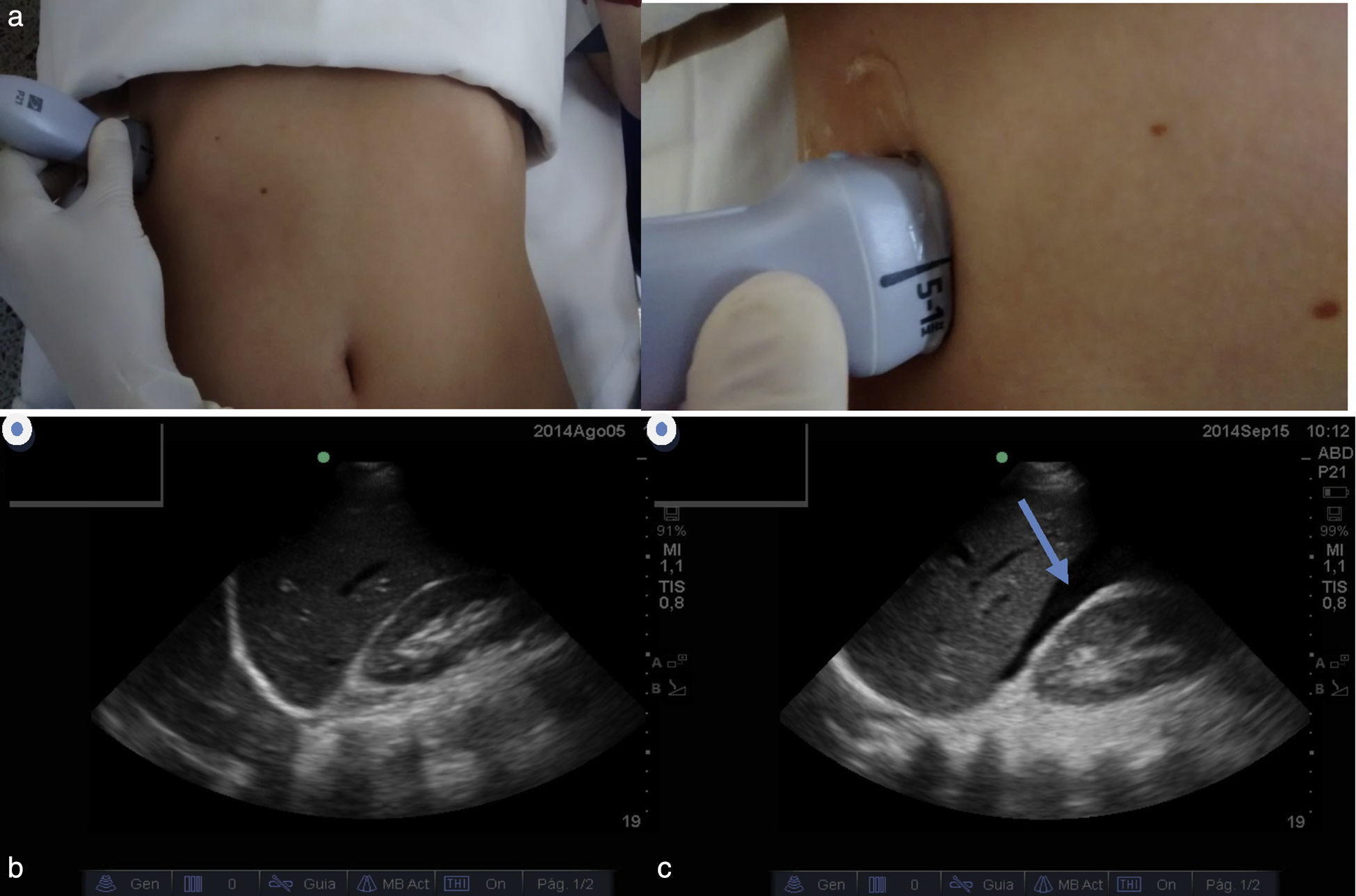
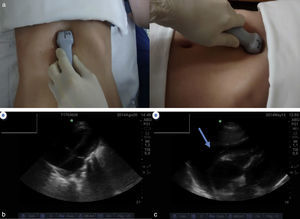
Superior right quadrantThis evaluates the hepatorenal space, the Morrison pouch and the right pulmonary base. This is the most sensitive in diagnosing hemoperitoneum, and the easiest to obtain in the technical sense.
This is done by placing the transducer slightly in front of the right midaxillary line between the 7th and 8th costal margins. The position marker must be oriented towards the head of the patient. It is important to visualize the diaphragm to determine the presence of a potential haemothorax. For the adequate evaluation of this window, it is necessary to move the transducer up or down along the patient's torso (Fig. 2a–c).
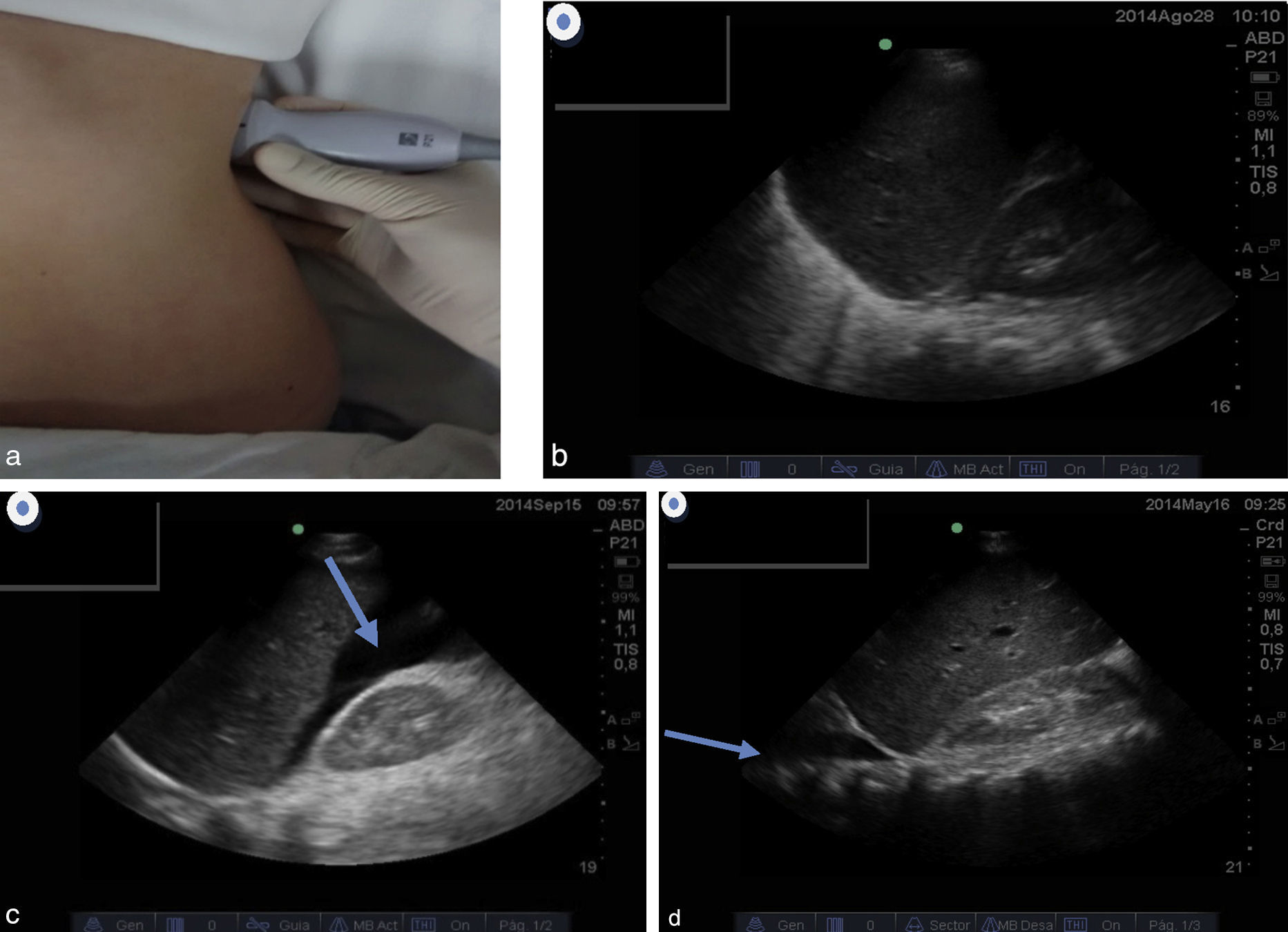
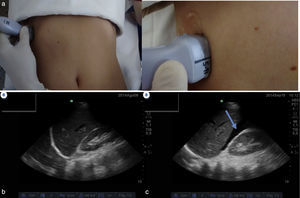
Left superior quadrantThis quadrant evaluates the splenorenal space and uses the spleen as an acoustic window. It also visualizes the left pulmonary base and ipsilateral paracolic gutters.
This is done by placing the transducer at the level of the posterior axillary line between the 7th and 8th costal margins and the position marker should be oriented towards the head of the patient. As with the right window, the diaphragm must be located and it is necessary to move the transducer up or down along the torso of the patient to obtain a better image. This window is the most technically difficult to visualize (Fig. 3a–d).
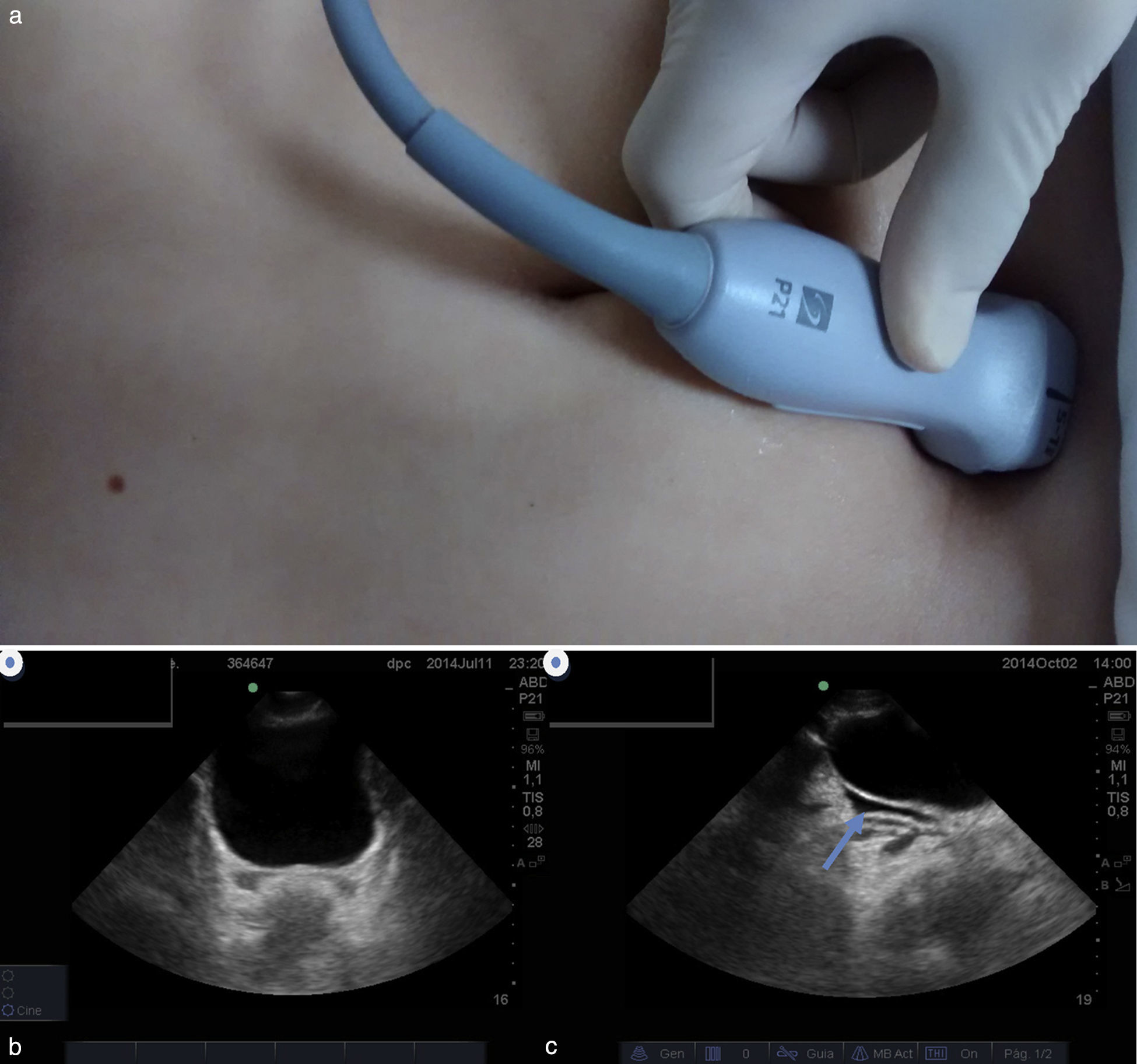
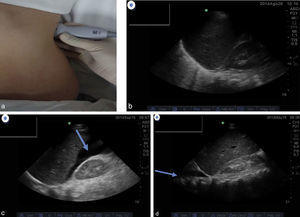
Pelvic or supra-pubic windowThis is to evaluate the presence of free liquid at the pelvic level, but does not rule out pelvic fractures because this liquid can originate from solid organ injuries. In women, there could also be liquid in the window for physiological reasons. The full bladder is used as the ultrasound window, since the absence of urine does not lead to reliable results.
This is done by positioning the transducer at the supra-pubic level and should be visualized on the longitudinal and transversal axes (position indicator towards the head and then towards the right side of the patient) (Fig. 4a–c).
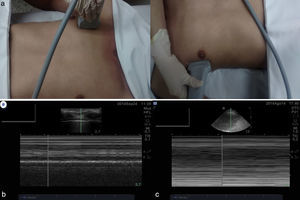
Pulmonary windowsThese are part of the eFAST examination and their objective is to detect the presence of pneumothorax. Here, high-frequency transducers (higher or equal to 10Mhz) are preferred, but not having them still makes it possible to visualize these windows, though the quality of the image is affected. The sensitivity of the ultrasound for detecting pneumothorax and haemothorax is higher than that of X-rays. This theory has been demonstrated in a variety of studies. In addition, the diagnosis is quick and easy to obtain.7,8
For the detection of pneumothorax, the transducer should be positioned in the superior pectoral region on both sides to detect the presence of pleural sliding. If there is a pneumothrax, there will be no sliding. Both M and B modes should be used, which are included on the controls of the device.
Using mode M, the presence of motion artefacts is evaluated. An image known as the “waves on the beach” sign indicates pleural sliding and can be used to rule out pneumothorax. Conversely, the image known as the “stratosphere” or “barcode” sign indicates an absence of sliding, which can be used to make the diagnosis of pneumothorax. It is important to note that on some occasions when the breathing of the patient is superficial, there isn’t always a reliable way to confirm the existence of pleural sliding. It is ideal to administer ventilation with positive pressure to better determine a diagnosis. Besides evaluating visually the pleural sliding, mode B (conventional) can then be used to evaluate the presence of B lines or comet-tail artefacts as the absence of these is strongly related to pneumothorax.
The diagnosis of pleural effusion, which in the field of trauma is interpreted as haemothorax, has already been described, and is carried out by evaluating the presence of free liquids in the pulmonary bases during the FAST examination (Fig. 5a–c).
This topic will be covered in greater detail in the chapter on pulmonary ultrasound.
The learning curve of the ACEP recommends doing 25–50 ultrasounds to obtain the appropriate sensitivity. It is clear that the reliability of the examination increases with experience as it is an operator-dependent procedure.
EvidenceSensitivity in detecting hemoperitoneum varies greatly in the reported literature, ranging from 73% to 99%.9,10
A recent study with over 4000 patients, conducted by Lee and colleagues,11 reported a sensitivity of 85% in detecting hemoperitoneum, regardless of blood pressure figures, which had a sensitivity of 96%.
A later meta-analysis included 62 studies and over 18,000 patients, showing a sensitivity of 78.9% and a specificity of 99.2%, concluding that the FAST examination does not detect small quantities of liquid, though it does have great specificity and is useful in decision-making.12
Quinn and Sinert13 conducted a systematic review of literature, which included patients with penetrating injuries in the torso. In this case, the FAST examination was very useful in making the decision to carry out an exploratory laparotomy; a negative examination does not completely rule out the presence of hemoperitoneum.
The FAST examination is particularly useful in patients with penetrating injuries at the precordial level. In blunt abdominal trauma associated with hypotension, sensitivity reaches almost 100% and a positive examination is almost always an indication that emergency surgical management is needed.14–16
IndicationsIn the last few years, the FAST-ABCDE examination has been implemented for emergency patient care using ultrasound starting from the admittance of the patient to detect problems in the airway, to guide intubation and to monitor a patient's clinical state in real time. It also uses the windows described in the conventional exam, which is a new tool that is recommended by experts, though it will require validation studies to know its real use and scope.
Many indications have been assigned to the FAST, but only one has been validated by different studies over the last few decades, which is to confirm the presence of free liquid in the hemodynamically unstable patient with abdominal trauma,17 with a high specificity reaching 99% and a sensitivity of 75.8%.12
However, its use can be extended beyond that of unstable patients, as it has also become a useful diagnostic tool to monitor the state of patients with abdominal trauma who might have initially been stable but whose condition progressively destabilized, helping a physician to determine if this state is a direct consequence of the abdominal bleeding.18
Despite this, it is difficult to not rely on such a useful, available, economical, and portable tool in cases of patients with non-traumatic acute abdominal injury. In some cases, these patients may benefit from ultrasounds (e.g. aneurism of the abdominal aorta, ruptured ectopic pregnancy). Currently, the guidelines of the American Institute of Ultrasound in Medicine approve the use of FAST in medical situations.19
eFAST allows for a chest examination of patients with haemodynamic instability, aiding in the identification of the location of bleeding to plan the correct surgical approach and rule out the presence of pneumothorax.18
All of these indications should be taken into account according to each medical speciality that will benefit from this tool. In anaesthesia, for example, it will be useful to evaluate unstable patients in the peri-operative stage (haemothorax, pneumothorax, cardiac taponade, abdominal bleeding). The intensive care phyisican will always have access to this tool and it will be instrumental in monitoring the state of the trauma patient (blunt abdominal trauma that becomes unstable, or occult pneumothorax that turns into tension pneumothorax with mechanical ventilation) or that of a patient who has just come from surgery. The emergency medical specialist can use FAST as a diagnostic tool, which will be immensely useful in determining the aetiology and management of the unstable patient.
Most frequent mistakes in the use of FASTWhenever a physician decides to use FAST as a diagnostic tool, the objective of the procedure should be clearly defined as a lack of knowledge of the indications is often the main reason for the mistake in the first place. Whenever a FAST examination is carried out, it is important to remember that the sensitivity of this diagnostic tool for detecting retroperitoneal bleeding is not optimal.20,21 FAST is not a tool to study the origin of the bleeding as its diagnostic performance is not adequate for visceral injuries. That is, it is highly sensitive in detecting free liquid, but not in identifying the origin of this liquid. Another common mistake involves not performing the examination in a serial way, reporting negative initial results when in reality the liquid accumulated was not sufficient to give a positive result.22
The most common reasons for false positives are: viscera with liquid content (such as the intestine and gallbladder) as perirenal fat can be interpreted as liquid, and a bladder that is not sufficiently full can also give the impression of free liquid in the pelvic window; in these cases, it is recommendable to repeat the test to look for peristalsis, recognize the sign of the double perirenal line,23 and report the pelvic window as an unreliable unit so a better acoustic can be obtained for the full bladder. The diagnostic imaging should not be removed from the medical record. In this way, it is possible to avoid the interpretation of basic clinical conditions like ascitis as being FAST positive.
FundingThe authors did not receive sponsorship to undertake this article.
Conflicts for interestThe authors have no conflicts of interest to declare.
Please cite this article as: Giraldo-Restrepo JA, Serna-Jiménez TJ. Examen FAST y FAST extendido. Rev Colomb Anestesiol. 2015;43:299–306.