Advances in prenatal sonography have enlightened us about the problems of ovarian cysts in the foetus, their management during pregnancy and after birth. Most ovarian cysts diagnosed antenatally are simple anechoic cyst or complex with septations/sedimentation/retracting clot. Appearance of a uniformly solid appearing ovarian cyst prenatally is extremely rare. We present a case of a 29-year-old primigravida, who reported at 31 weeks of gestation with a scan suggestive of congenital adrenal neuroblastoma for further management. With subsequent review by foetal medicine consultant it was diagnosed to be complicated foetal ovarian cyst. The foetus delivered vaginally at term. The neonate underwent right salpingo-oophrectomy on 3rd day of life due to torsion. The histopathology revealed a benign ovarian tumour with torsion and necrosis. The case highlights the importance of making all attempts to arrive at an accurate diagnosis for foetal abdominal masses. Once diagnosis is made, we need to evaluate further for signs of complications. Expertise can be improved by clinical, sonographic and pathological correlation.
Los avances en la ecografía prenatal nos han esclarecido los problemas de quistes ováricos en el feto, su gestión durante el embarazo y tras el nacimiento. La mayoría de los quistes de ovario diagnosticados prenatalmente son quistes simples anecoicos o complejos con septaciones/sedimentación/coágulo retráctil. La aparición prenatal de un quiste ovárico con apariencia uniformemente sólida es extremadamente rara. Se presenta el caso de una primigesta de 29 años, quien se presentó a las 31 semanas de gestación con exploración indicativa de neuroblastoma suprarrenal congénito que precisaba tratamiento. La revisión posterior por parte de un clínico experto en medicina fetal dio lugar al diagnóstico de quiste ovárico fetal complicado. La madre dio a luz por vía vaginal a término. La neonato fue sometida a salpingo-ooferoctomía derecha en su tercer día de vida debido a una torsión. El estudio histopatológico reveló un tumor ovárico benigno con torsión y necrosis. El caso pone de relieve la importancia de poner todos los medios posibles para alcanzar un diagnóstico preciso en masas abdominales fetales. Una vez realizado el diagnóstico, es necesario evaluar más a fondo para determinar si hay signos de complicación. La destreza diagnostica puede mejorarse mediante la correlación clínica, ecográfica y patológica.
Cystic abdominal masses in the foetus are reliably identified by ultrasound, but it may not be possible to make a precise prenatal diagnosis. The challenge is much more if the mass is appearing solid on prenatal ultrasound. When such an abnormality is suspected, confirmation of normality of organ systems is essential which includes kidneys, bladder, stomach, bowel and gall bladder. Determination of gender also helps. The shape, size, character, position of the lesion may suggest the most likely diagnosis. Presence of heterogenous echoes suggests complications like torsion or haemorrhage into the cyst. We present a rare case of homogenously solid appearing foetal ovarian cyst prenatally diagnosed and correlated with postnatal USG and surgical findings. This case emphasises the importance of proper understanding of foetal anatomy and morphological characteristic of such foetal tumours on ultrasound and the advantage of follow up in improving clinical expertise.
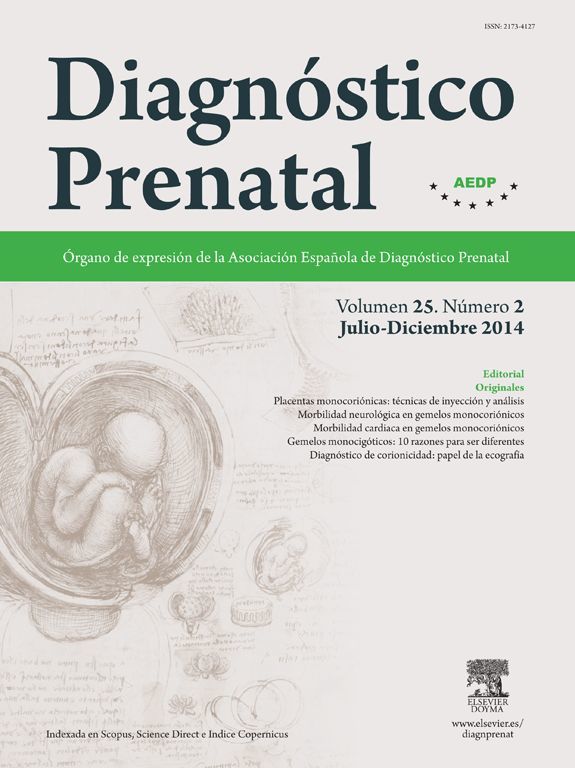
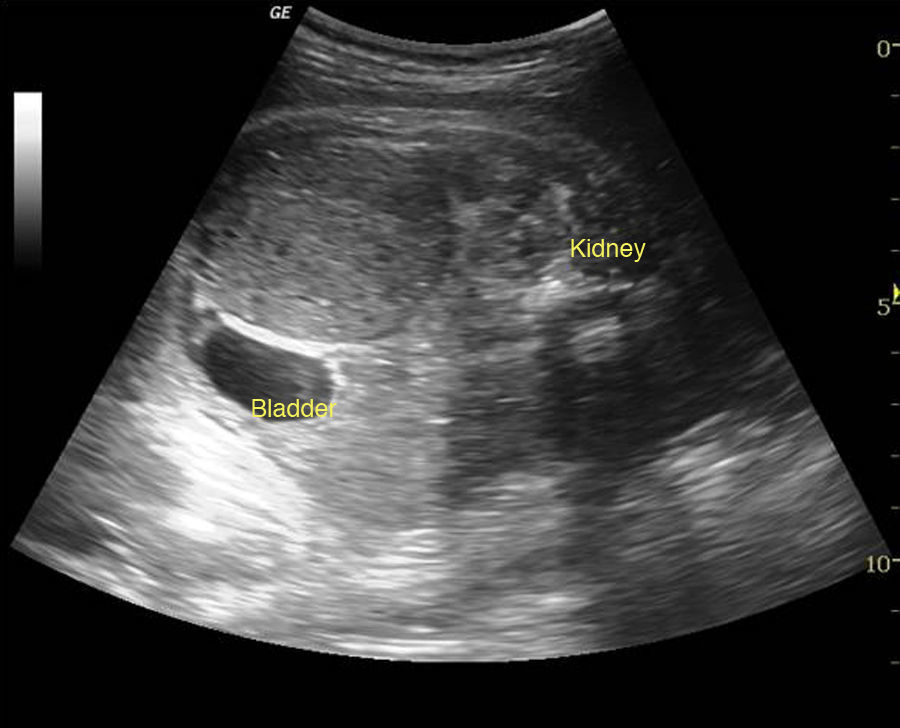
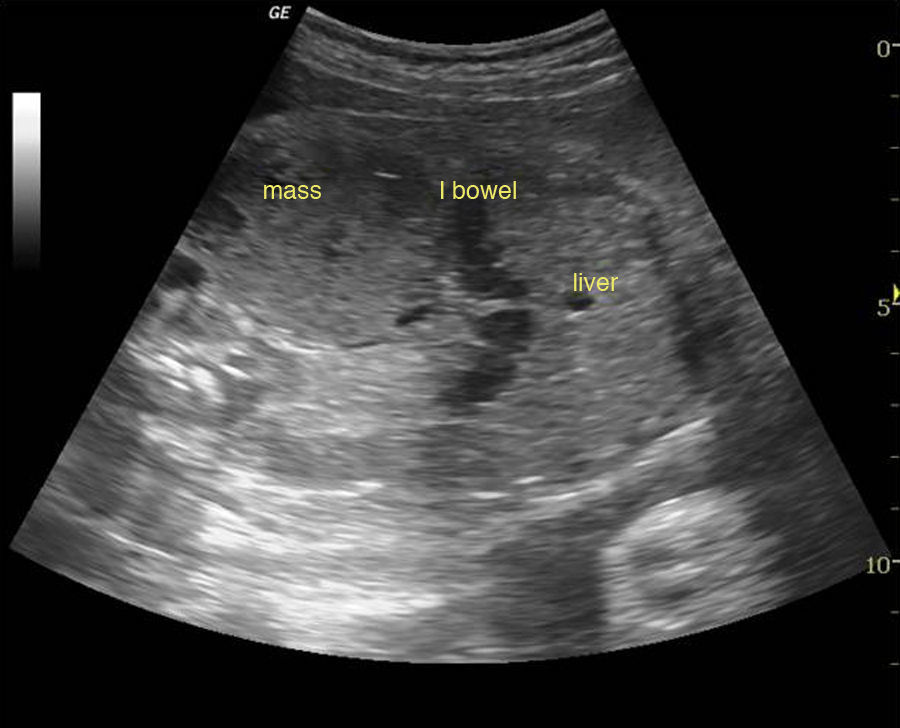
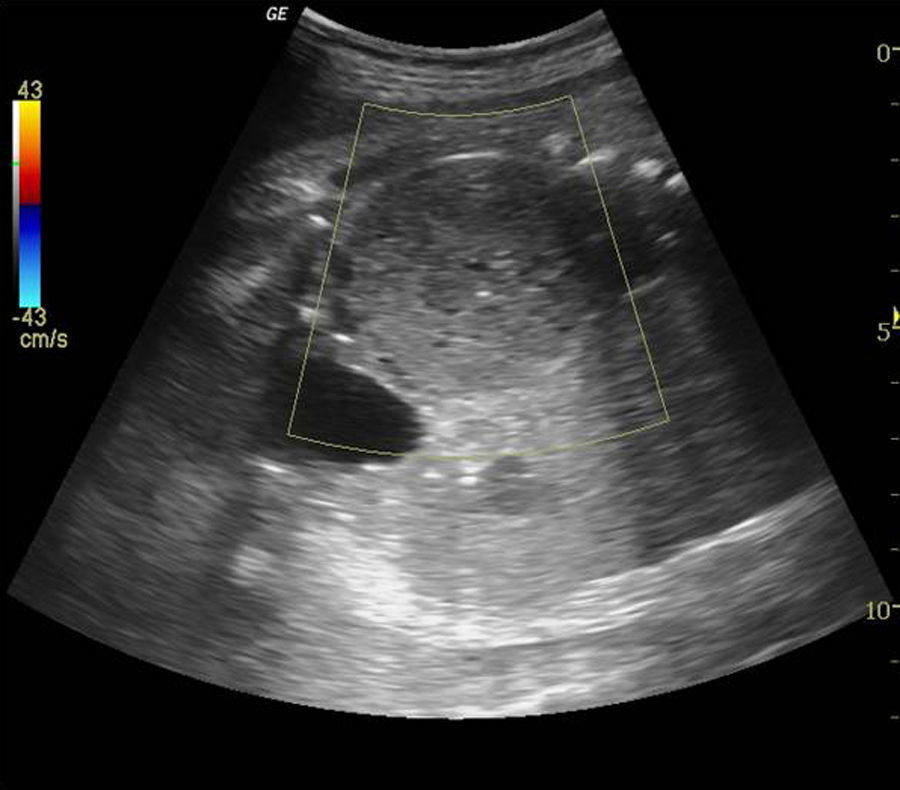
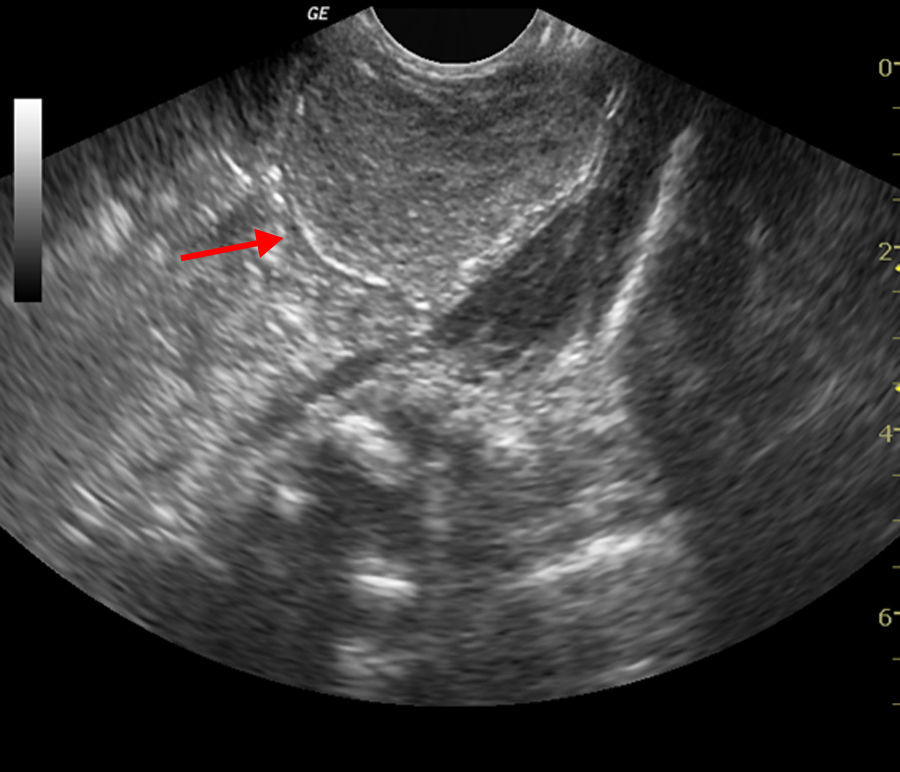
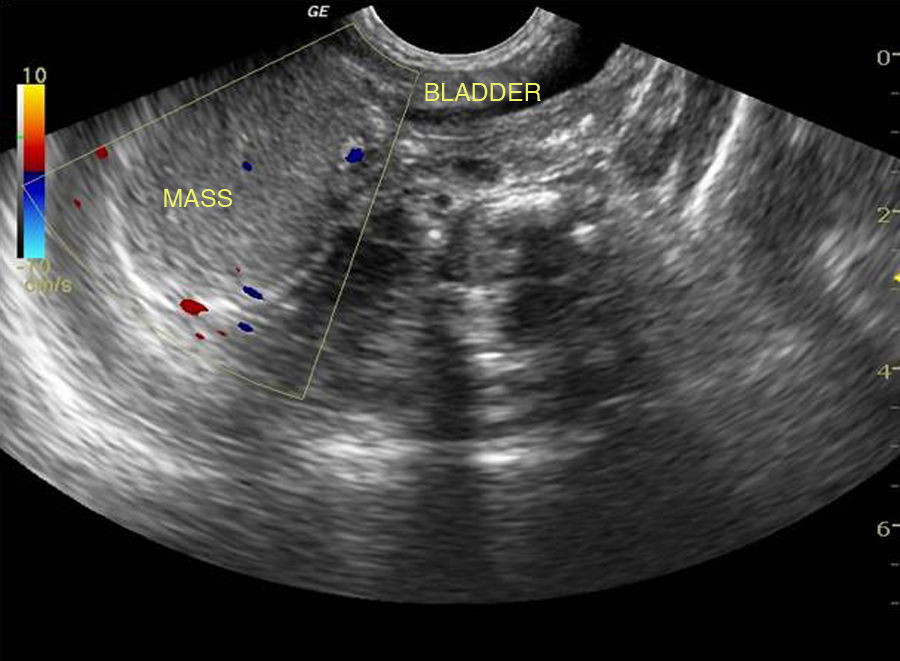
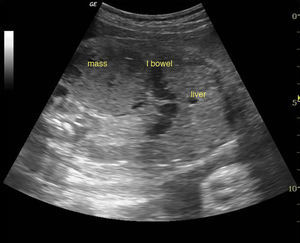
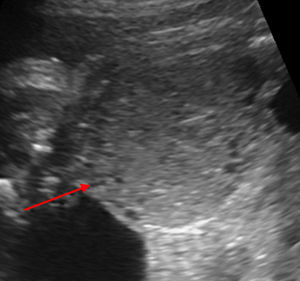
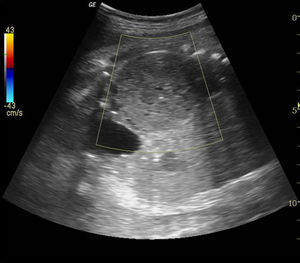
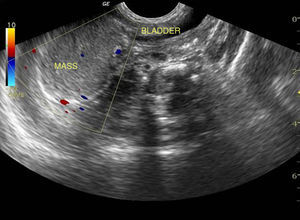
Case summaryA 29-year-old primigravida referred from a private practitioner to our hospital at 31 weeks of gestation for second opinion regarding a malformation scan suggesting congenital adrenal neuroblastoma. Subsequent evaluation by our foetal medicine specialist revealed a foetal intraabdominal diffusely hypoechoic well defined mass, measuring about 5cm by 4.8cm, seen just above, lateral and indenting the urinary bladder. Although appearing solid on echogenicity there was posterior acoustic enhancement suggesting the mass to be fluid filled (Fig. 1). Normally situated right kidney was seen above the mass, ruling out neuroblastoma of adrenal gland as a possibility, as adrenal tumours would be solid with no acoustic enhancement and located superior to the kidney. Mass appeared separate from the bowel, and stomach thus excluding these organs as the origin (Fig. 2). On zooming in on the margins of the abdominal mass there were presence of daughter cysts which convinced us of the ovarian origin of the mass (Fig. 3). There was no vascularity on colour Doppler flows (Fig. 4). By process of exclusion, identification of the female gender, position and characteristics of the mass and absence of Doppler flows, complicated ovarian cyst was the most likely diagnosis. Paediatric surgeons planned to re evaluate the baby post delivery.
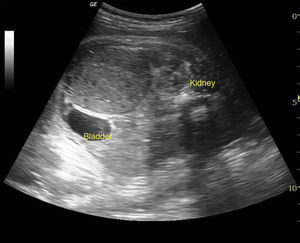
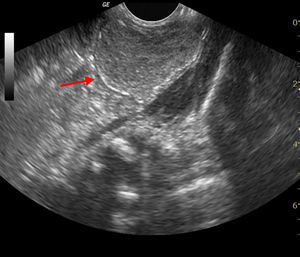
On follow up scan the lesion remained same with normal foetal growth and amniotic fluid. Patient had a spontaneous vaginal delivery at term of a baby girl weighing 2.9kg with an Apgar score of 9/10. The neonate was further managed under the supervision of the paediatric surgeon. An ultrasound and CT scan on the neonate on day 2 was suggestive of a peritoneal mass, probably a mesenteric cyst (Fig. 5). Even after the birth and with the use of advanced imaging tools like CT scan the diagnosis of the mass was still a dilemma. Since an initial diagnosis of complicated ovarian cyst was made antenatally, our inquisitive foetal medicine specialist rescanned the neonate on day 3 of life and visualised a normal uterus with normal left ovary and the right ovary replaced by the complex ovarian cyst with calcifications at the margins seen in the ovarian fossa with no vascularity suggesting torsion (Figs. 6 and 7).
Tumour markers in the neonate were α foetoprotein 20,471mg/mL and β HCG<2mU/mL. The high value of alpha foetoprotein could be explained by the passive transfer via placenta in the 3rd day old neonate. The neonate was operated the same day. Intra operatively a right ovarian cyst of 5 by 5cm was found which had undergone torsion and was completely necrosed (Fig. 8). Right salpingo-oophorectomy was performed. The intraoperative and postoperative periods were uneventful. Histopathology report confirmed a benign ovarian tumour with torsion.
DiscussionIn the past few years the ability to diagnose foetal abdominal masses has improved because of technical advances in imaging. However definitive diagnosis of these abdominal masses is still quite challenging. They may arise virtually from any abdominal organ. Excluding cystic masses arising from the urinary system (hydronephrosis, multicystic dysplastic kidneys, paranephric pseudo cysts, hydroureter, and distended bladder) or dilated bowel, the most common intra-abdominal cystic mass include an ovarian cyst, meconium pseudo cyst, enteric duplication cyst, or mesenteric cyst.1 Solid appearing masses are liver and adrenal tumours, retroperitoneal teratoma or complicated/torsion in an ovarian cyst. Only 1% of foetal ovarian cysts have been reported in literature as purely echodense.2 The case we have presented was giving a false appearance of a solid tumour that may have misled the previous sonographer on it being an adrenal neuroblastoma. Although diffusely hypoechoic due to long-standing torsion, there was posterior acoustic enhancement suggesting it to be fluid filled.
An ovarian cyst should be suspected on ultrasound when a female foetus has a cystic intra-abdominal mass which is separate from the organs of the urinary and gastrointestinal tract. Quarello et al. have described the “daughter cyst sign”, which consists of presence of small (2–8mm), round, anechoic structures seen within or outside the main cyst as a diagnostic feature of an ovarian cyst. This feature confirmed the ovarian origin of the cysts in Lee's study with a sensitivity of 82% and specificity of 100%.3 The presence of these daughter cysts at the periphery of the mass clinched the diagnosis of foetal ovarian cyst with greater degree of surety in our case (Fig. 3).
USG appearance of an ovarian cyst is variable, depending on its size or complications, such as haemorrhage or torsion. There is no established correlation between the sonographic findings and the histological nature of the ovarian cyst. Uncomplicated ovarian cyst typically appears as a unilocular anechoic purely cystic mass with an imperceptible cyst wall in the pelvis or more often abdomen of a female foetus. The cysts may subsequently increase, decrease, disappear or undergo complications such as torsion, haemorrhage or rupture.
When haemorrhage or torsion occurs, the morphology of the cyst dramatically alters. The appearance of such a complicated ovarian cyst will depend on the time elapsed between the bleeding and the imaging evaluation. As the intracystic clotted blood evolves, the appearance changes from diffuse echogenic material to diffuse echoes with visible fibrin strands, retracting thrombus or fluid debris levels. There may or may not be perceptible colour or spectral Doppler flow. Appearance of an echodense solid appearing ovarian cyst, as in our case, is an extremely rare presentation of a complicated ovarian cyst. Complicated cysts may have a definable thin echogenic wall due to dystrophic calcifications. This peripheral calcification was not perceptible in our foetus but on scanning the neonate after birth the echogenic rim of calcification was evident (Fig. 6).
Despite improvement in prenatal ultrasonographic diagnosis, the management of foetal ovarian cyst remains controversial. The majority of ovarian cysts undergo spontaneous regression and involution following delivery or in utero. Torsion of the enlarged ovarian cyst causing loss of an ovary is the most common complication of foetal ovarian cyst and occurs more frequently before than after birth. This risk must be weighed against the probability of cyst regression. The decision to intervene should depend on cyst size, USG characteristics, clinical symptoms and its progression. Serial ultrasound examinations during pregnancy are recommended to monitor the growth of the cyst and possible complications.
To avoid these potential complications, antenatal percutaneous aspiration of ovarian cysts has been suggested by most authors at a size cut off of 4–5cm. In utero decompression of foetal ovarian cyst facilitates preservation of ovarian function both by reducing the risk of torsion and the need for neonatal surgery.4 We deferred in utero intervention in our foetus because the initial diagnosis at 31 weeks itself suggested torsion with absent blood flow on Doppler.
Postnatal treatment options include conservative management, antenatal/postnatal cyst aspiration, cystectomy, oopherectomy. Most researchers believe, presence of signs of torsion or size more than 5cm requires early neonatal intervention. When postnatal surgery is contemplated cystectomy with preservation of maximal ovarian tissue is preferred over oopherectomy.5
ConclusionWide variety of masses can be detected in the foetal abdomen which poses a diagnostic dilemma. Attempt should be made to arrive at an accurate diagnosis and search for possible complication. Rare diagnosis is rare and often wrong. Most likely diagnosis is usually suggested by assessment of characteristic of the mass, foetal sex, position of the abdominal mass, its relation with other structures and the normality of other organs. The presence of daughter cyst seen at the periphery is a diagnostic feature of an ovarian cyst.
The case report highlights the importance of continuum of care through pregnancy and neonatal period. Expertise can be improved by making a dedicated attempt towards clinical–sonographic–pathological correlation.
Conflict of interestThe authors declare no conflict of interest.