Methicillin-resistance Staphylococcus aureus (MRSA) nasal carriage plays a key role in the pathogenesis of MRSA infections in hemodialysis patients. Our study was designed to evaluate the prevalence of MRSA nasal carriage in patients on chronic hemodialysis and its influence on development of MRSA bloodstream infections.
MethodologyOurs is a 12-month prospective observational study. A total of 50 patients who are on chronic maintenance hemodialysis were enrolled in this study. Prevalence of MRSA nasal carriage was studied using nasal swabs collected from the anterior nares. Swabs were inoculated on to Mannitol Salt Agar and HiCrom agar. Bactec blood culture was used to detect MRSA bloodstream infections.
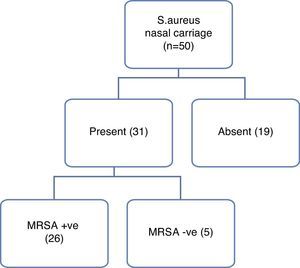
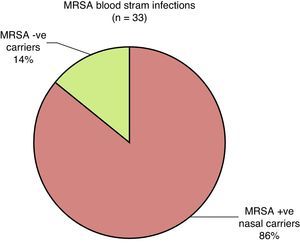
ResultsStaphylococcus aureus (S. aureus) nasal carrier state was detected 62% of patients. 83.87% of these S. aureus nasal carriers were found to be having MRSA. The incidence of MRSA bloodstream infections was 1.54 episode per 100 patient-months. MRSA bloodstream infection rates were significantly higher among MRSA nasal carriers as compared to non-MRSA carriers (p<0.001). Low hemoglobin levels were significantly more among MRSA positive nasal carriers as compared to non-MRSA nasal carriers.
ConclusionThis study reveals that MRSA nasal carriage is more prevalent among hemodialysis patients and it is an independent risk factor for the development of MRSA bloodstream infections. Early prevention and treatment of MRSA nasal carriage in hemodialysis patients may prevent MRSA bloodstream infections in hemodialysis patients.
El estado de portador nasal de Staphylococcus aureus resistente a meticilina (MRSA) desempeña un papel clave en la patogenia de las infecciones por MRSA en pacientes en hemodiálisis. Nuestro estudio se diseñó para evaluar la prevalencia de portadores nasales de MRSA en pacientes en hemodiálisis crónica y su influencia en la aparición de infecciones hemáticas por MRSA.
MetodologíaSe realizó un estudio prospectivo observacional de 12 meses. Participaron en el estudio un total de 50 pacientes en hemodiálisis de mantenimiento crónica. Se estudió la prevalencia de portadores nasales de MRSA con el empleo de muestras con escobillón nasales obtenidas de la parte anterior de los orificios nasales. Los escobillones se inocularon en Manitol Salt Agar y agar HiCrom. Se utilizó un hemocultivo Bactec para detectar las infecciones hemáticas por MRSA.
ResultadosSe detectó un estado de portador nasal de Staphylococcus aureus (S. aureus) en el 62% de los pacientes. En el 83,87% de estos portadores nasales de S. aureus se observó la presencia de MRSA. La incidencia de infecciones hemáticas por MRSA fue de 1,54 episodios por 100 meses-paciente. Las tasas de infección hemática por MRSA fueron significativamente superiores en los portadores nasales de MRSA en comparación con los no portadores de MRSA (p<0,001). Las concentraciones de hemoglobina bajas fueron significativamente más frecuentes en los portadores nasales positivos para MRSA en comparación con los no portadores nasales de MRSA.
ConclusiónEste estudio pone de relieve que el estado de portador nasal de MRSA es más prevalente en los pacientes en hemodiálisis y constituye un factor de riesgo independiente para la aparición de infecciones hemáticas por MRSA. La prevención y tratamiento precoces del estado de portador nasal de MRSA en los pacientes en hemodiálisis pueden prevenir las infecciones hemáticas por MRSA en los pacientes en hemodiálisis.
S. aureus is a ubiquitous microorganism in both healthy and compromised hosts. The anterior nares have been shown to be the main reservoir of S. aureus in adults.1 It has been proposed that approximately10–50% of adults were colonized with S. aureus.2,3 Nasal carriage of S. aureus has been demonstrated to be a significant risk factor for nosocomial and community-acquired infection in various populations. Self-inoculation occurs when organisms from the nose colonize other areas of the skin leading to infection. Studies have found that nasal colonization with methicillin-resistant S. aureus (MRSA) poses an increased risk of infection. MRSA strains are resistant to several groups of broad-spectrum antibiotics.4 This mechanism of increased spreading under antibiotic pressure may contribute to the worldwide increase in the prevalence of MRSA in hospitals. Hemodialysis patients are particularly vulnerable to staphylococcal colonization as well as infections.5 Little is known about the prevalence of MRSA among hemodialysis patients in India. The purpose of this study was to determine the prevalence of MRSA nasal carriage among hemodialysis patients and its influence on development of bloodstream MRSA infections.
MethodologyThe present study was conducted as a prospective study between 1/10/2012 and 1/11/2013. 50 subjects who were on maintenance hemodialysis were observed for over 12months. All subjects gave informed consent for participation in the study, which was approved by the Human Ethics Committee. All of the procedures were in accordance with the Helsinki Declaration of 1975.
Nasal specimens were collected using 2 sterile dry cotton-wool swabs for each patient. The swab was circled through both nostrils consecutively while applying an even pressure. Swabs were inoculated on to Mannitol Salt Agar and HiCrom agar (Hi MeReSe Media, HiMedia, Mumbai) simultaneously. Inoculated Mannitol Salt Agar (MSA) plates were incubated at 37°C for 24h. Yellow colonies were identified as S. aureus by standard conventional techniques.6 MRSA was detected by Oxacillin (1μg, HiMedia) by disk diffusion (DD) method, further confirmed by using Cefoxitin disk (1μg, HiMedia) which is an accurate surrogate marker for mecA gene detection. The diameter of zone of inhibition was recorded as per CLSI (Clinical and laboratory standards institute) guidelines.7 HiCrom agar was prepared as per the instruction manual. Inoculated plates were incubated at 37°C for 24h. Bright blue colonies on HiCrom agar were identified by standard techniques and MRSA confirmed by Oxacillin and Cefoxitin DISC. ATCC strain of S. aureus was used as the standard control strain.
MRSA positive S. aureus carriage was defined by at least two positive cultures taken within a week. MRSA bloodstream infections are defined as the presence of MRSA bacteremia in bactec blood cultures in an HD patient in whom no other obvious source of infection was evident.
Data were analyzed by using the SPSS software, version 13.0. The t-test and the chi-square test were used where appropriate. Continuous variables were presented as mean±standard deviation. p values less than 0.05 were considered as significant.
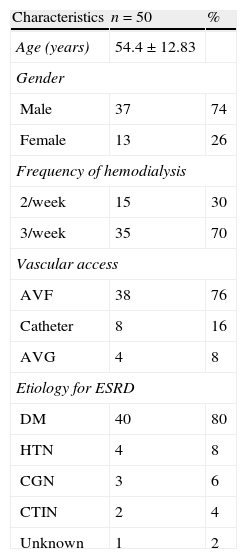
ResultsA total of 50 ESRD patients on chronic hemodialysis were enrolled into this study. The age range of our study population was 28–74 years with mean age being 54.4±12.83 years. 74% of our patients were males and 26% were females. 70% of our patients were on thrice weekly hemodialysis, and 30% on two times dialysis per week. In our study population diabetic kidney disease was the leading cause for ESRD (80%), followed by hypertension (8%), chronic glomerulonephritis (6%), chronic tubulointerstitial nephritis (4%) and unknown causes (2%). Hemodialysis was performed through arteriovenous fistula (AVF) as vascular access in 76% of patients, tunneled cuffed hemodialysis catheters in 16% and arteriovenous graft (AVG) in 8% of patients (Table 1).
Demographics of hemodialysis patients.
| Characteristics | n=50 | % |
| Age (years) | 54.4±12.83 | |
| Gender | ||
| Male | 37 | 74 |
| Female | 13 | 26 |
| Frequency of hemodialysis | ||
| 2/week | 15 | 30 |
| 3/week | 35 | 70 |
| Vascular access | ||
| AVF | 38 | 76 |
| Catheter | 8 | 16 |
| AVG | 4 | 8 |
| Etiology for ESRD | ||
| DM | 40 | 80 |
| HTN | 4 | 8 |
| CGN | 3 | 6 |
| CTIN | 2 | 4 |
| Unknown | 1 | 2 |
AVF, arterio-venous fistula; AVG, arterio-venous graft; DM, diabetes mellitus; HTN, hypertension; CGN, chronic glomerulonephritis; CTIN, chronic tubulointerstitial nephritis.
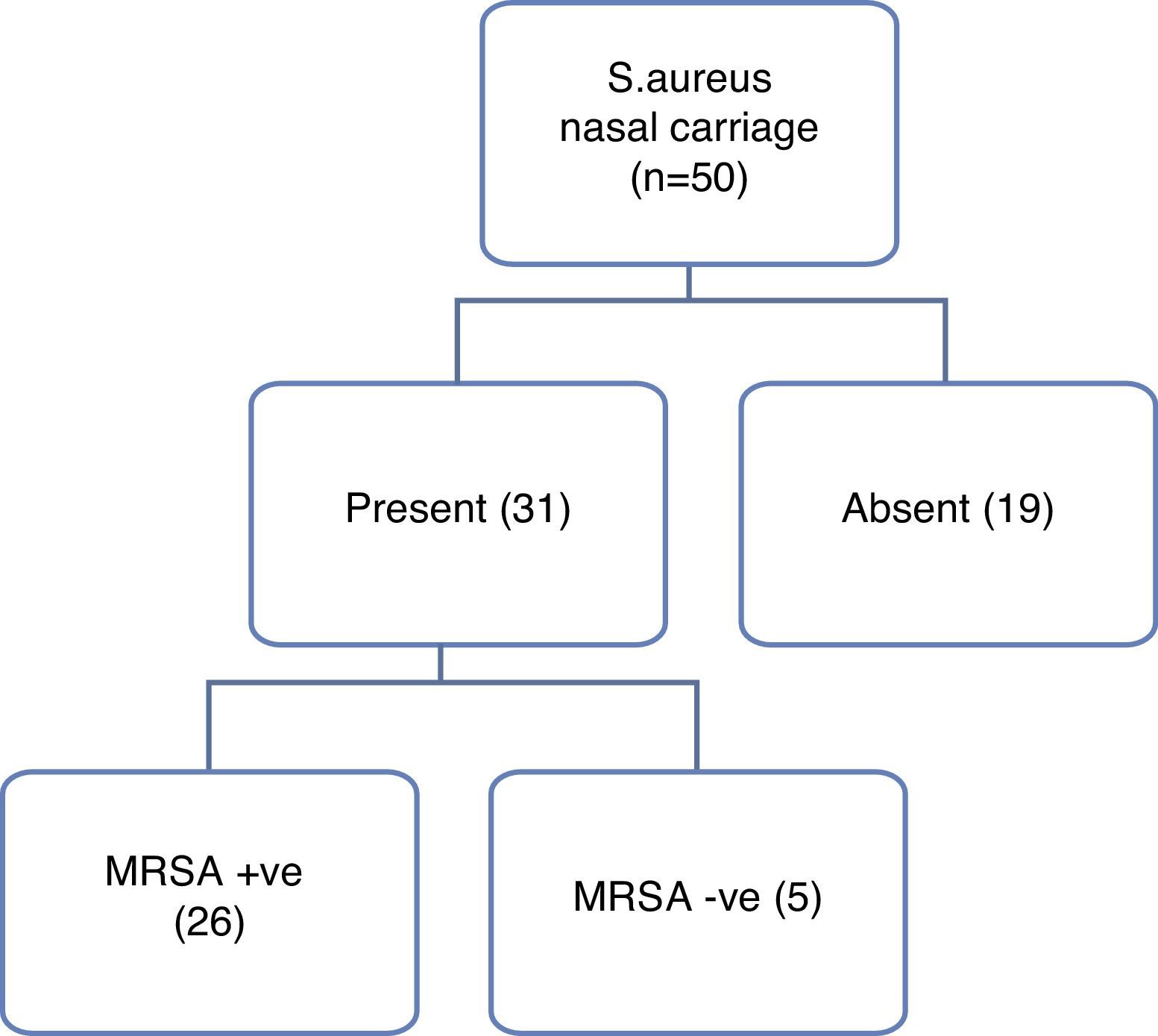
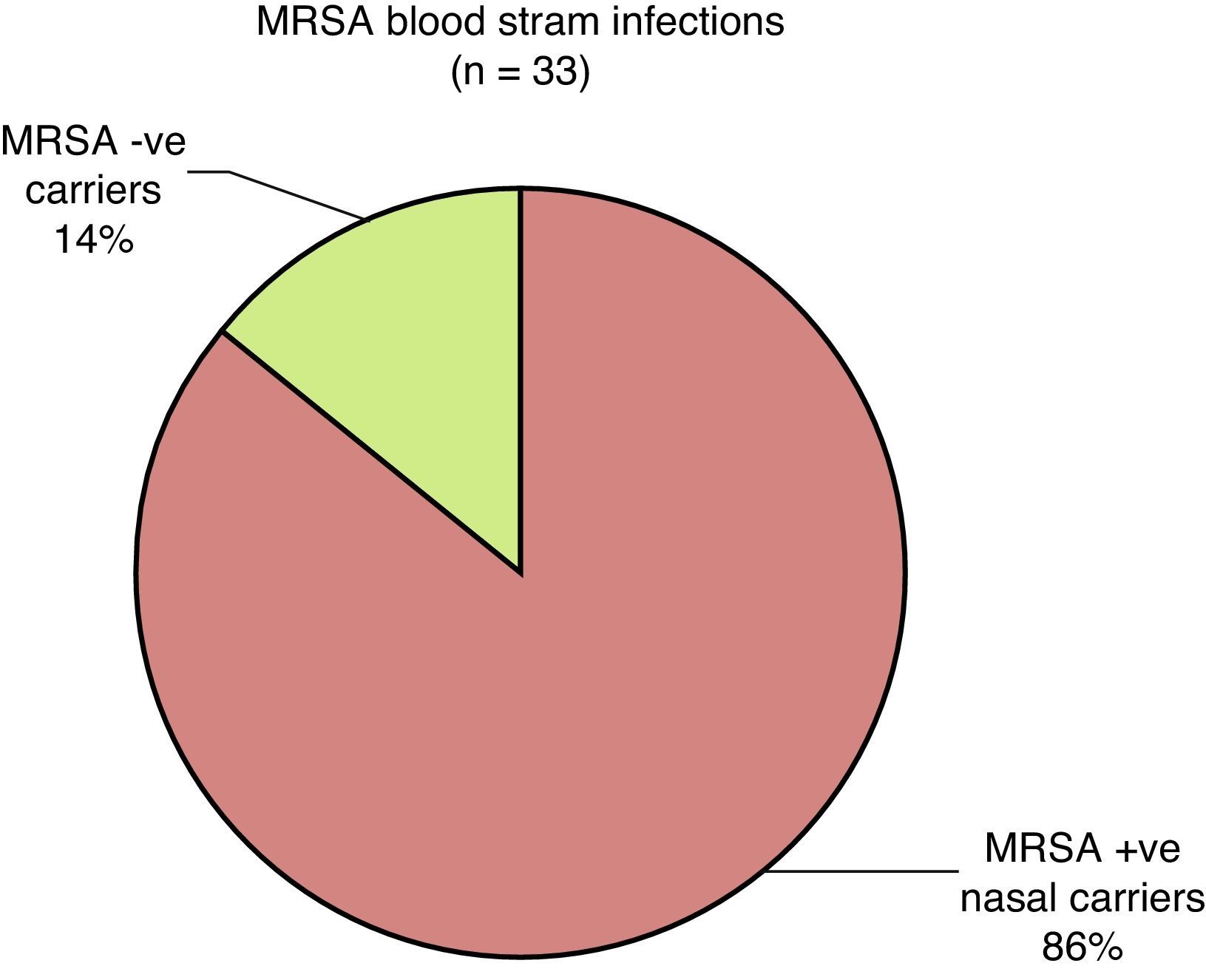
S. aureus nasal carrier state was detected in 31 of the 50 patients on hemodialysis (62%) (Fig. 1). Methicillin resistance rate was 83.87% (26 of 31) among the S. aureus nasal carriers. 33 episodes of bacteriologically proven MRSA bloodstream infections were detected in one-year period. 32 episodes of MRSA bloodstream infections are found in 26 MRSA positive nasal carriers as against only one episode of MRSA bloodstream infection in 5 non-MRSA nasal carriers (Fig. 2). MRSA bloodstream infection rates were significantly higher among MRSA nasal carriers as compared to non-MRSA carriers (1.34 vs. 0.24 episode/100 patient-months, p<0.001).
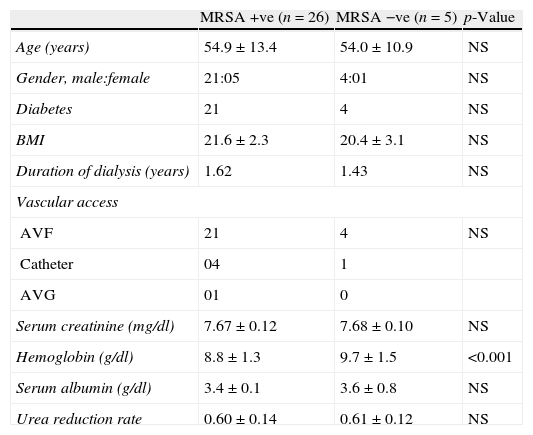
Risk factors for the development of MRSA bloodstream infections were analyzed between MRSA positive and non-MRSA nasal carriers. There were no differences in age, gender, Diabetes, BMI, mode of dialysis, vascular access and duration of dialysis in either univariate or multivariate analysis (Table 2). Low hemoglobin levels were found in MRSA positive nasal carriers as compared to non-MRSA nasal carriers and these findings were statistically significant.
Characteristics of patients with and without MRSA nasal carriage.
| MRSA +ve (n=26) | MRSA −ve (n=5) | p-Value | |
| Age (years) | 54.9±13.4 | 54.0±10.9 | NS |
| Gender, male:female | 21:05 | 4:01 | NS |
| Diabetes | 21 | 4 | NS |
| BMI | 21.6±2.3 | 20.4±3.1 | NS |
| Duration of dialysis (years) | 1.62 | 1.43 | NS |
| Vascular access | |||
| AVF | 21 | 4 | NS |
| Catheter | 04 | 1 | |
| AVG | 01 | 0 | |
| Serum creatinine (mg/dl) | 7.67±0.12 | 7.68±0.10 | NS |
| Hemoglobin (g/dl) | 8.8±1.3 | 9.7±1.5 | <0.001 |
| Serum albumin (g/dl) | 3.4±0.1 | 3.6±0.8 | NS |
| Urea reduction rate | 0.60±0.14 | 0.61±0.12 | NS |
AVF, arterio-venous fistula; AVG, arterio-venous graft; BMI, body mass index; MRSA, methicillin resistant Staphylococcus aureus.
Nasal carriage of S. aureus plays a key role in the epidemiology and pathogenesis of staphylococcal infections. S. aureus nasal carriage has been shown to be more common in hemodialysis patients than in the general population.8 In our study the prevalence of S. aureus nasal carriage among hemodialysis patients was found to be 62%. This prevalence is consistent with the prevalence rates of 44.0–84.0% reported in other studies.9,10 Methicillin resistance in staphylococci has a low binding affinity for all β-lactam antibiotics. This MRSA is responsible for several difficult to treat infections in humans and their prevalence is progressively increasing. Nasal colonization of MRSA in patients on hemodialysis is reported to be 12–65%.11,12 In our study the prevalence of MRSA nasal carriage was found to be 52%. 83.87% of S. aureus nasal carriages were found to be MRSA.
Hemodialysis patients with nasal carriage of S. aureus have a 1.8–4.7-fold increase of S. aureus bloodstream infections compared with non-carriers.10 The strains of S. aureus, which were recovered from the nostrils, are same as those recovered from subsequent bloodstream infections suggesting majority of S. aureus bloodstream infections are autoinfections.13 Hemodialysis patients are particularly vulnerable to the development of MRSA carrier state and MRSA bloodstream infection. In our study, 33 episodes of MRSA bloodstream infections were detected in one-year period. Studies have shown that S. aureus nasal carriage act as an independent risk factor for the development of S. aureus bloodstream infections. In a study of 138 patients on peritoneal dialysis, almost 50% of patients with S. aureus bloodstream infections had nasal carriage of S. aureus.14 Lai and co-workers proposed that MRSA nasal carriage in patients receiving hemodialysis is associated with a 4.99-fold increased risk of infection-related mortality.15 In our study, the incidence of MRSA bloodstream infections were significantly high among MRSA nasal carriers (1.34 vs. 0.24 episodes per 100 patient-months, p<0.001).
Prior histories of bacterial infection, history of diabetes, old age, the use of a dialysis catheter, lower hemoglobin level, lower serum albumin and iron overload are independent risk factors for bacterial infections in chronic hemodialysis patients.16–19 In our study, no statistically significant difference was observed in age, gender, diabetes, BMI, serum albumin levels, mode of dialysis, duration of dialysis, type of vascular access and urea reduction rate between MRSA and non-MRSA nasal carriers. Anemia was found be significantly more prevalent among MRSA carriers in our study. Our finding was consistent with those of Keane and Collins.20
Our study has several limitations. Firstly, the number of study group was small. Secondly, the follow up period was short. Thirdly, characterization of the strains of MRSA in nasal carriers and bloodstream infections was not done in our study. Thus, we cannot establish the exact causal relationship between MRSA carriers and MRSA bloodstream infections.
ConclusionThe present study demonstrates that MRSA nasal carriage was more prevalent in hemodialysis patients and it is an independent risk factor for the development of MRSA bloodstream infections. Prevention and treatment of MRSA nasal carriers with appropriate antibiotics may translate into reduction of MRSA bloodstream infections and infection-related mortality.
Conflict of interestThe authors declare no conflict of interest.