Antibiotic resistance is a global problem today. The knowledge of bacterial resistances trend is crucial for antibiotic empiric therapy. Nephrology practice meets several sites of microbiological interest. We aimed to study the prevalence of bacterial pathogens and their emerging resistance patterns to antibiotics commonly used.
MethodsWe reviewed 1249 microbiologic reports obtained between January 2009 and December 2013 from patients admitted to Nephrology Department. We analyzed the antibiotic susceptibility patterns for the firsts 4 identified bacterial pathogens.
ResultsThe bacterial pathogens most frequently isolated were: Escherichia coli, Staphylococcus aureus, Enterococcus faecalis, Pseudomonas aeruginosa, Candida, Staphylococcus epidermidis, Klebsiella pneumoniae. The percentage of extended spectrum beta-lactamase-producer Escherichia coli was 37% and methicillin-resistent Staphilococcus aureus was 15%.
ConclusionAntibiotic resistance of bacterial pathogens to commonly used antibiotics is increasing. Our report on bacterial spectra of major antibiotic susceptibility patterns enables a more rational use.
La resistencia a los antibióticos es un problema mundial hoy en día. El conocimiento de las tendencias de resistencias bacterianas es fundamental para el tratamiento empírico con antibióticos. La nefrología confluye con varios puntos de interés microbiológico. Perseguimos estudiar la incidencia de patógenos bacterianos y sus patrones emergentes de resistencia a los antibióticos más comunes.
MétodosSe revisaron 1249 informes microbiológicos de entre enero de 2009 y diciembre de 2013 de pacientes ingresados a cargo de la unidad de nefrología. Se analizaron los patrones de sensibilidad a antibióticos para los primeros 4 patógenos bacterianos que se identificaron.
ResultadosLos patógenos bacterianos más comunes fueron: Escherichia coli, Staphylococcus cureus, Enterococcus faecalis, Pseudomonas aeruginosa, Candida, Staphylococcus epidermidis, Klebsiella pneumoniae. El porcentaje de cepas Escherichia coli productoras de betalactamasas de espectro extendido fue del 37% y de Staphylococcus aureus resistente a la meticilina fue de 15%.
ConclusiónLa resistencia de los patógenos bacterianos a los antibióticos comunes está en aumento. Nuestro informe sobre el espectro bacteriano de patrones de sensibilidad los principales antibióticos permite un uso más racional.
The antibiotic bacterial resistance is an important public health problem. The inappropriate use of antibiotics is critical to development of bacterial resistance. The Nephrology Departments in routine clinical practice meet several sites of microbiological interest: Urinary Tract, Central Venous Catheter (CVC) for hemodialysis treatment, Peritoneal Catheter (PC) for peritoneal dialysis (PD) treatment, the peritoneal dialysis fluid, the bloodstream, the CVC- or PD-skin exit-sites. Antibiotic resistance is a global problem today. The widespread use of antibiotics and the changing of bacterial pathogens susceptibility profiles requires regular review of treatment guidelines. The knowledge of the epidemiology of pathogens and the antibiotic resistance is necessary for timely and effective treatment of infections1–2 and it is crucial to use the most appropriate antibiotic empiric therapy (ET) for first-choice treatment. We studied the prevalence of bacterial pathogens and their emerging resistance patterns to antibiotics commonly used. We performed a retrospective analysis of microbiological reports from patients admitted to Nephrology Department between January 2009 and December 2013.
Materials and methodsThe infection sites were: urine (49.1%), soft tissues (12.1%), peritoneal dialysis fluid (10.1%), bloodstream (9.7%), CVC- or PD-skin exit-site (6.9%), CVC- or PC-tips (12.1%). We used commercial blood culture bottles to assess bacteraemia and sterile cotton for superficial infections; the urine samples and CVC- or PC-tips were collected in sterile single-use pots for microbiological culture. All samples were collected and processed from patients in accordance with standard protocols. Antibiotic susceptibility of the isolates was done by disc diffusion method according to international guidelines recommendations.
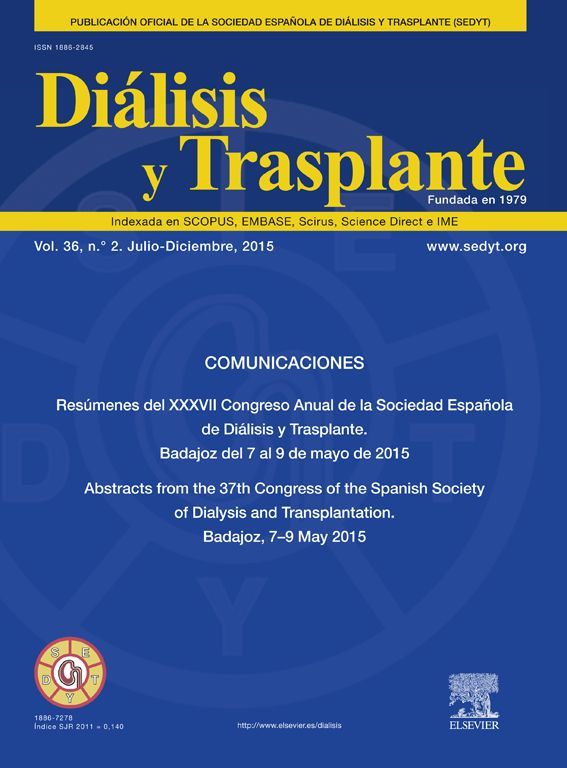
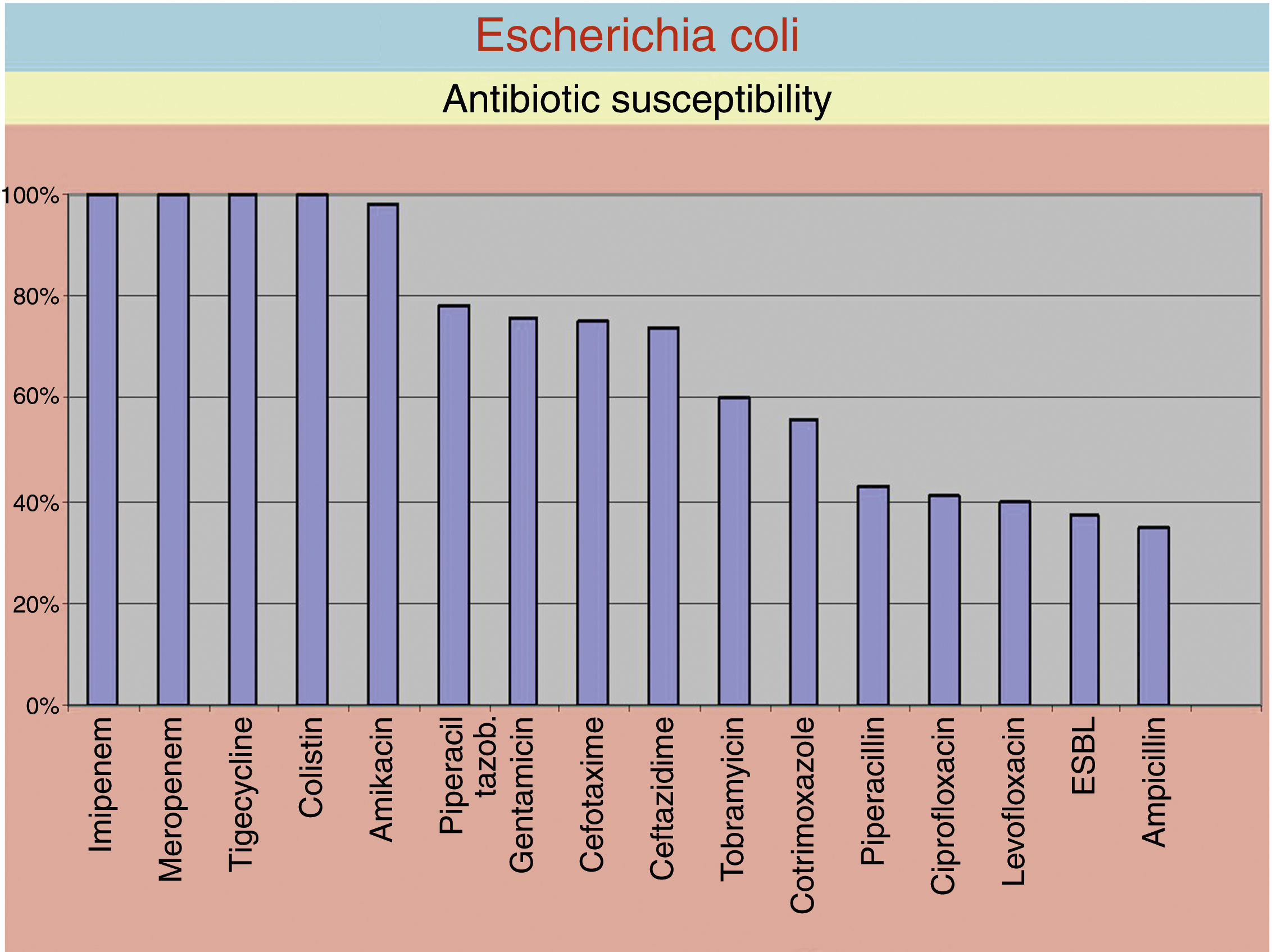
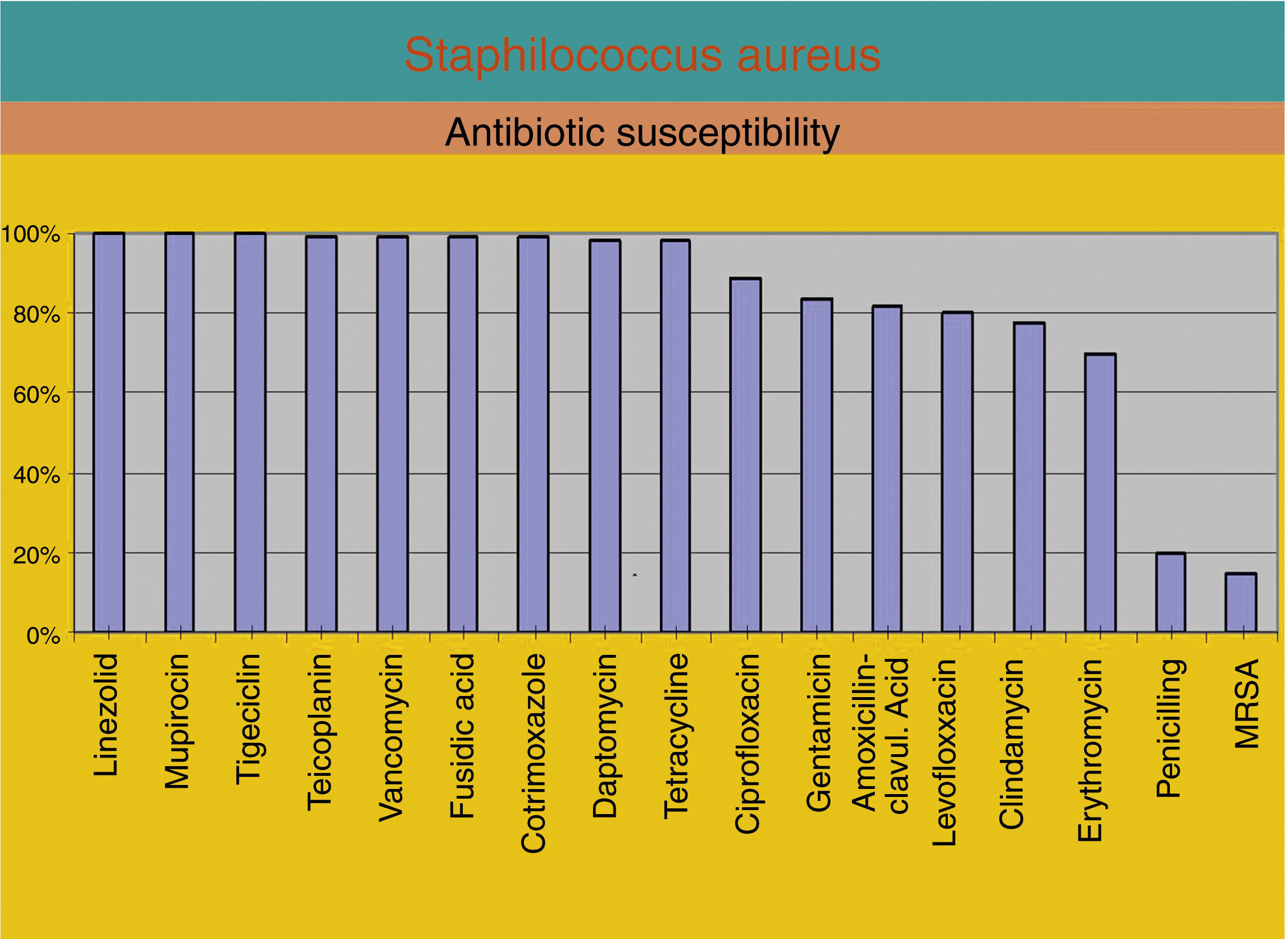
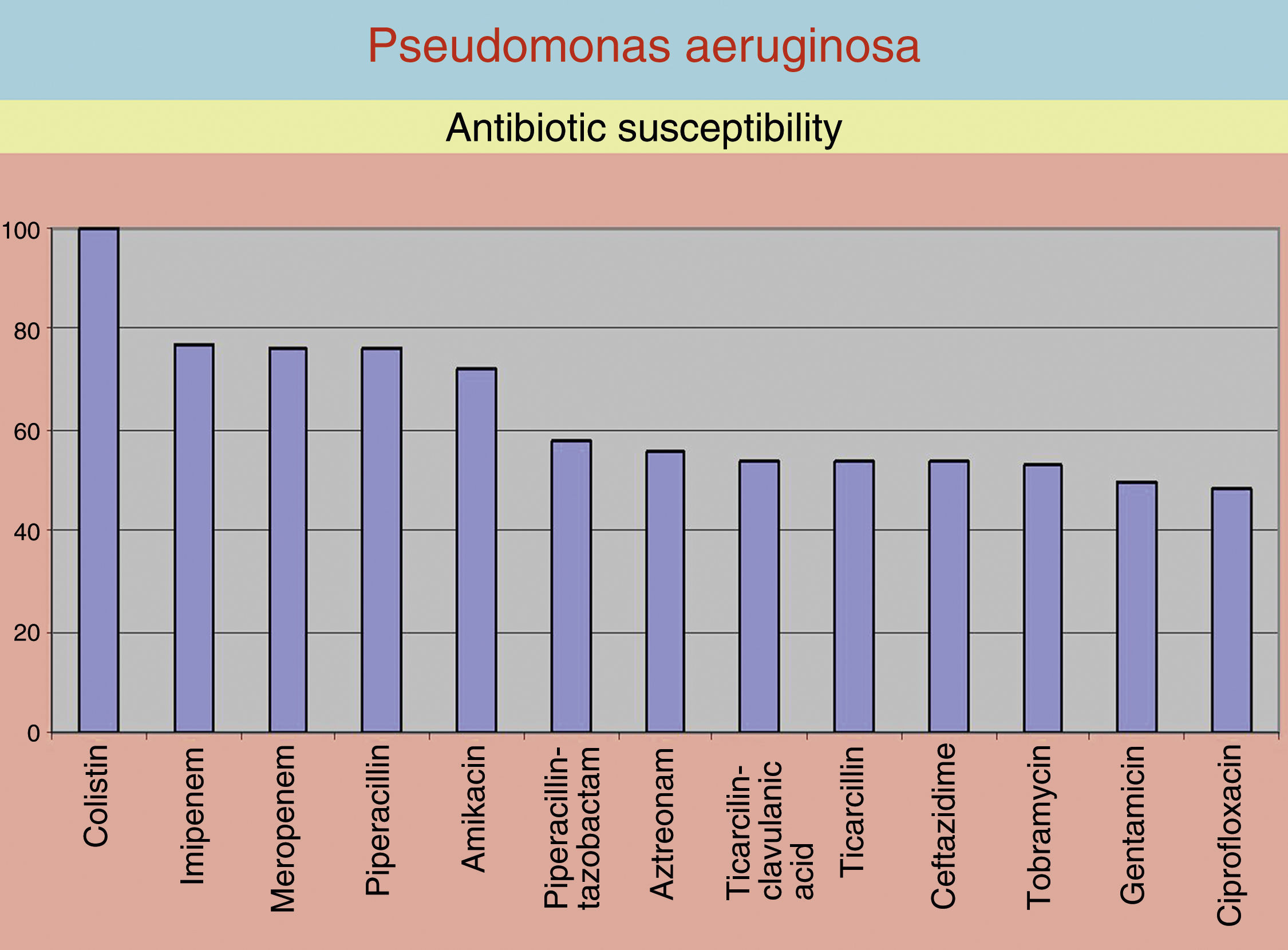
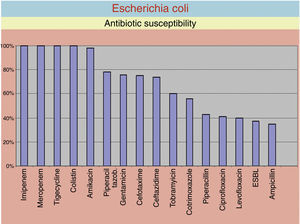
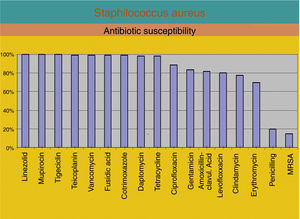
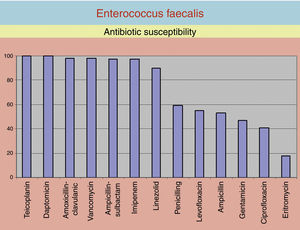
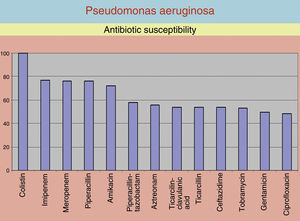
ResultsWe analyzed 1249 microbiological reports. The majority of the isolates were: Escherichia coli (19.3%), Staphylococcus aureus (13.4), Enterococcus faecalis (12.5); Pseudomonas aeruginosa (8.6), Candida (8.2), Staphylococcus epidermidis (7.6), Klebsiella pneumoniae (6.0), Staphilococcus haemoliticus (2.4), Enterococcus cloacae (2.0). We reviewed the antibiotic susceptibility patterns for the firsts 4 bacterial pathogens identified. We found: (a) E. coli: the susceptibility to imipenem, meropenem, colistin, ertapenem and tigecycline was 100%; to amikacin was 97.7%; the susceptibility to piperacillin-tazobactam, gentamicin, cefotaxime, ceftazidime, tobramycin, cotrimoxazole, piperacillin, ciprofloxacin, levofloxacin, ampicillin was under 90%. The proportion of extended spectrum betalactamase (ESBL)-producers was 37% (Fig. 1). (b) S. aureus: the susceptibility to linezolid, mupirocin and tigecycline was 100%; to teicoplanin and vancomycin, fusidic acid, daptomycin, trimethoprim/sulfamethoxazol, tobramycin and tetracycline was over 90%. The proportion of methicillin resistant Staphilococcus aureus (MRSA) was 15% (Fig. 2). (c) E. faecalis: the susceptibility to teicoplanin, daptomycin was 100%; to amoxicillin and clavulanic acid, vancomycin, ampicillin-sulbactam, imipenem and linezolid was over 90%. (Fig. 3) (d) P. aeruginosa: the susceptibility to colistin was 100; to imipenem was 78%; to meropenem and piperacillin was 77%; to amikacin was 75% (Fig. 4).
DiscussionPatients with chronic kidney disease are at risk for infections caused by nosocomial multidrug resistant (MDR) pathogens exhibiting decreased susceptibility to many antimicrobials. Suboptimal antibiotic stewardship practices, such as using antibiotics when unnecessary and using broad-spectrum antibiotics or multiple antibiotics, have been linked to the epidemic of MDR organisms. The antimicrobial regimens can be modified when the infecting strain has been identified and antimicrobial susceptibilities are known. The susceptibility profile may vary from one geographical location to another and may also change with time. Systematic monitoring of antimicrobial susceptibility trends can help to guide ET.3–6 The nephrology practice meets multiple pathologies of microbiological interest: post-infectious glomerulonephritis, complicated Urinary Tract Infections (UTI), acute pyelonephritis, CVC-related infections, PD-related peritonitis, CVC- or PD-catheter skin exit-site infections, bloodstream infection (sepsis, bacteraemia). The prevalence of MDR bacterial pathogens, e.g. MRSA, ESBL-producing Enterobacteriaceae or vancomycin-resistant enterococcus (VRE), is increasing.7–10 The wide availability and the inappropriate use of broad-spectrum antibiotics in the community may explain this situation. Therefore periodic evaluation of drug resistance patterns is necessary. The antibiotic resistance can be minimized by periodic epidemiological surveys of aetiological agents and their antibiotic sensitivity patterns leading to recognition of the most frequently encountered pathogens in a particular geographical area.11 In our study, Escherichia coli, Staphylococcus aureus and Enterococcus faecalis showed different antibiotic susceptibility patterns (Figs. 1–3). Pseudomonas aeruginosa showed high percentage of susceptibility to colistin only (Fig. 4). Both Gram-positive and Gram-negative were resistant to fluoroquinolones. We believe that the ET should prescribe the antibiotics with a balanced cost-effectiveness and cover both Gram-positive and Gram-negative bacteria. Based on our survey, in the case of suspected UTI and/or pyelonephritis we prescribe as ET: amikacin, amoxicillin/clavulanic acid, also it is recommended to supplement with metronidazole. In the case of suspected CVC infection we prescribe as ET: trimethoprim/sulfamethoxazole and amikacin. Should not be used fluoroquinolones in UTI as ET because the susceptibility is less than 55%. Penicillin G should not be used as ET because its lowest susceptibility field.
ConclusionsInfections caused by MDR organisms are becoming more frequently in daily practice. Antibiotic resistance of bacterial pathogens to commonly used antibiotics is increasing and is important to review the recommended guidelines for ET in line with local patterns of bacterial pathogens and antibiotic susceptibilities. The surveillance of antimicrobial resistance is necessary. Depending on antibiotic susceptibility pattern of the isolates, antibiotic ET should be updated.
Conflict of interestThe authors have declared that no conflict of interest exists.