Typhoid fever with classical features presents no difficulty in recognition. However, when it presents atypically in the guise of one of its rare complications, diagnosis becomes difficult and appropriate treatment is delayed. Typhoid glomerulonephritis is one such rare complication. Mesangial proliferative glomerulonephritis, IgA nephropathy, acute diffuse proliferative glomerulonephritis and crescentic IgA nephropathy have been reported in the past. Membranoproliferative glomerulonephritis (MPGN) type II in association with typhoid fever has never been reported. We report a 13-year-old boy presenting with high grade fever, hematuria, proteinuria and Salmonella typhi bacteremia. Kidney biopsy showed MPGN type II. He had a complete recovery of his renal abnormality following treatment for his typhoid fever.
La fiebre tifoidea cuando se presenta con las características clásicas no es difícil de reconocer. No obstante, cuando se presenta de modo atípico, en forma de una de sus complicaciones excepcionales, el diagnóstico es difícil y el tratamiento apropiado se retrasa. Una de dichas complicaciones es la glomerulonefritis tifoidea. Previamente se han descrito la glomerulonefritis proliferativa mesangial, la nefropatía por depósito de IgA, la glomerulonefritis proliferativa difusa aguda y la nefropatía con semilunas y depósito de IgA. Nunca se ha documentado la glomerulonefritis membranoproliferativa (GNP) de tipo II asociada a fiebre tifoidea. Describimos a un adolescente de 13 años de edad que se presentó con fiebre alta, hematuria, proteinuria y bacteriemia por Salmonella typhi. En la biopsia renal se demostró GNP de tipo II. Tras el tratamiento de la fiebre tifoidea el paciente se restableció por completo de su anomalía renal.
Typhoid is usually contracted by ingestion of food or water contaminated by fecal or urinary carriers excreting Salmonella enterica serotype typhi. Most patients who present to hospitals with typhoid fever are children or young adults from 5 to 25 years of age.1 Complications occur in 10–15% of patients and are particularly likely in patients who have been ill for more than two weeks. Many complications have been described, of which gastrointestinal bleeding, intestinal perforation, and typhoid encephalopathy are the most important. Typhoid glomerulonephritis although uncommon, is not rare. Here we report a 13-year-old boy presenting with typhoid glomerulonephritis following Salmonella typhi bacteremia.
Case reportA 13-year-old boy, studying in a residential school presented to us with history of high grade fever with chills, loose stools with abdominal cramps and hematuria since 10 days associated with generalised myalgia and joint pains. He denied any history of pedal edema, oliguria, dysuria, urgency or precipitancy while passing urine. There was no history of skin rashes, haemoptysis and recent increase in blood pressure. He denied any history of sore throat in the recent past. His past history, personnel history and birth history were unremarkable. On examination, he was averagely built with a body mass index of 20.56kg/m2. He was febrile with a temperature of 38.8°C, blood pressure 120/80mmHg, pulse rate 94/min and a respiratory rate of 20/min. Rest of the physical examination and systemic examination were within normal limits.
Laboratory investigations at the time of admission were as follows: haemoglobin 10.8g/dL, total leukocyte count 11,800/cmm, platelet count 272,000/cmm, Blood Urea Nitrogen (BUN) 31mg/dL (11.06mmol/L), serum creatinine 0.9mg/dL (79.56mol/L), total proteins 5.4g/dL, albumin 2.3g/dL, C-reactive protein 15mg/L, procalcitonin 3.81ng/mL. Routine urine analysis showed a specific gravity 1.010, pH 5.0, proteins 2+, neutrophils 20–25/hpf, RBCs 35–40/hpf and his spot urine protein to creatinine ratio (PCR) was 3.04. His X-ray of chest was normal and his abdominal ultrasound revealed bilateral enlarged, swollen kidneys with increased cortical reflectivity and loss of corticomedullary differentiation. Patient's blood, urine and stool culture were negative and his serum was negative for malaria, leptospira and dengue infections. His 2D-echocardiography showed no vegetations. Patients serum complement 3 (C3) level were low (9mg/dL), C4 level were normal and Anti-Streptolysin O titre was negative. Patient's serum was negative for human immunodeficiency virus (HIV) 1 and 2, Hepatitis B Virus, Hepatitis C Virus and cryoglobulins. Work-up for vasculitis and connective tissue disorders was negative. High Resolution Computed Tomography of chest and Computed Tomography of abdomen and pelvis were performed; which revealed multiple, small, discrete, bilateral supraclavicular, hilar, retroperitoneal and mesenteric lymph nodes. He was empirically started on anti-tubercular therapy, following which his fever settled down and he became asymptomatic after having 3–4 days of high grade fever. His urinary abnormalities returned to normal and he was discharged after a fever free period of 48h.
10 days after the discharge he got readmitted with high grade fever with chills and hematuria. Laboratory investigations during this admission revealed haemoglobin 10.6mg/dL, total leukocyte count 10,100/cmm, platelet count 498,000/cmm, BUN 11mg/dL (3.92mmol/L), creatinine 0.71mg/dL (62.76mol/L), calcium 7.51mg/dL, total protein 4.4g/dL and albumin 2.2g/dL. Urinalysis showed proteins 3+, neutrophils 25–30/hpf, RBCs 15–20/hpf with spot urine PCR of 12. Patients C3 levels were persistently low (7mg/dL), serum for angiotensin converting enzyme levels was normal and IgM-Cytomegalovirus, IgM-Epstein Barr Virus, Paul Bunnel test and serum protein electrophoresis were negative. Patients blood and urine culture were resent and bone marrow aspiration (BMA) and kidney biopsy were performed after obtaining a written informed consent. Patients BMA and bone marrow biopsy were unremarkable.
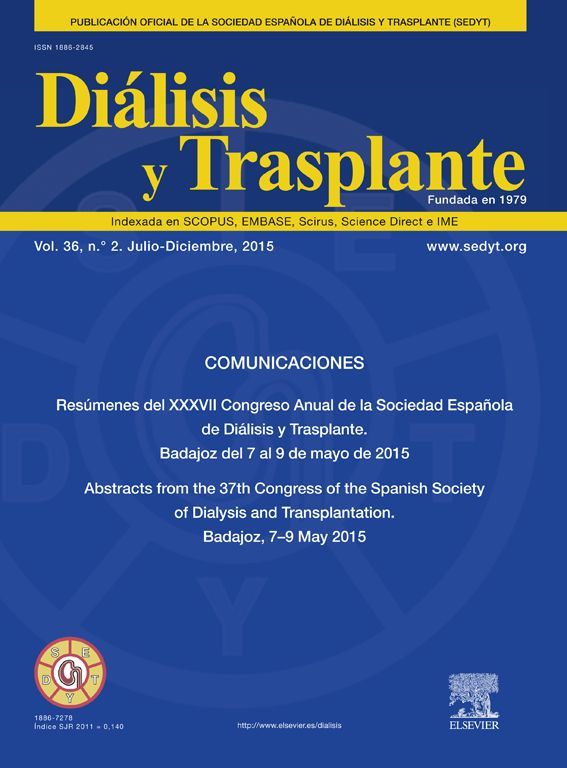
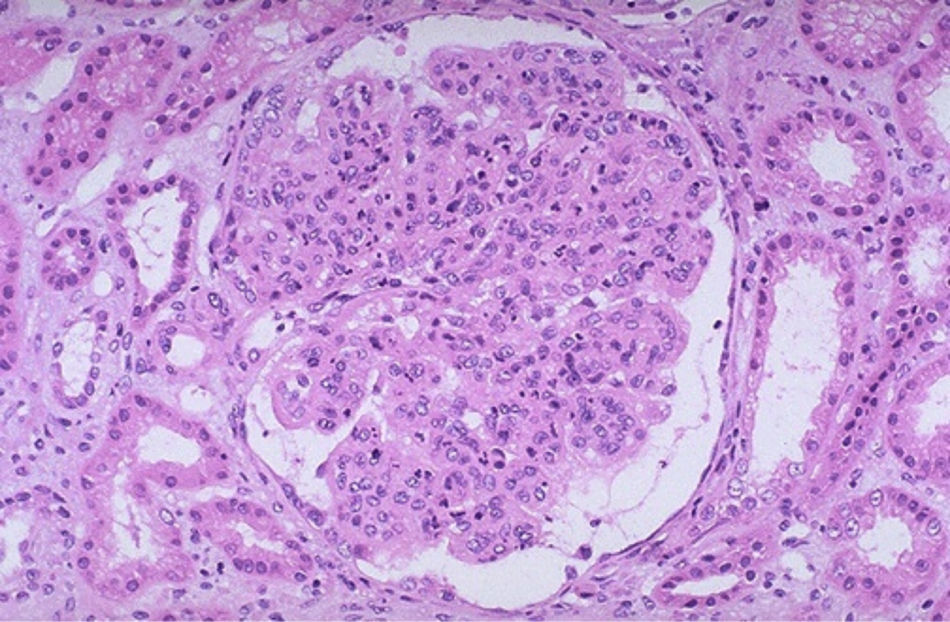
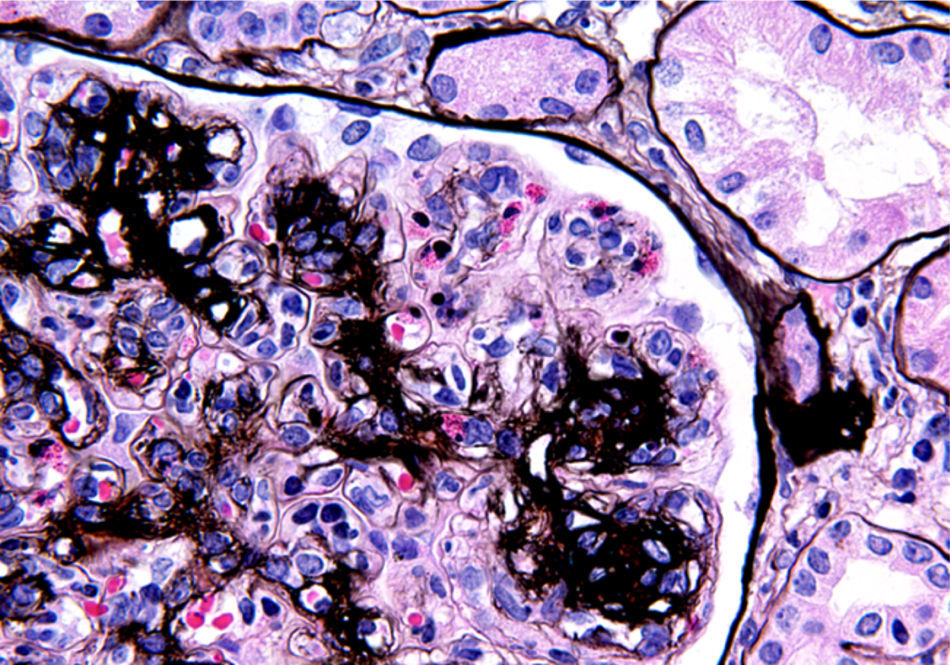
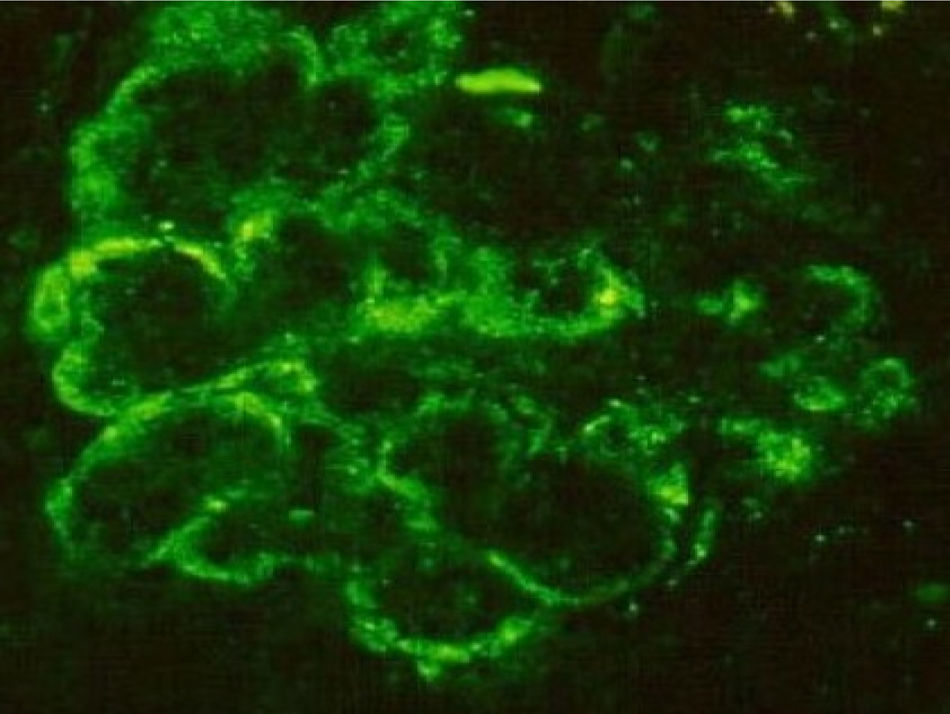
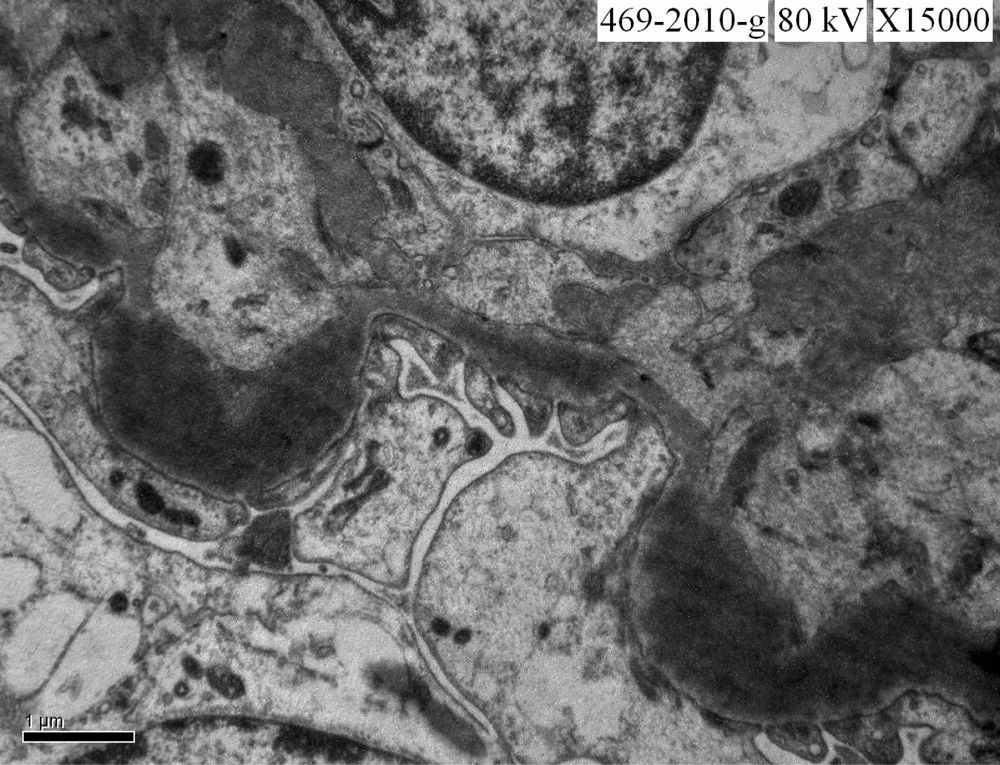
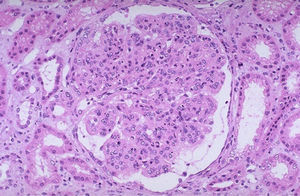
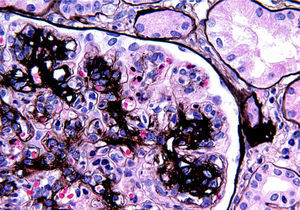
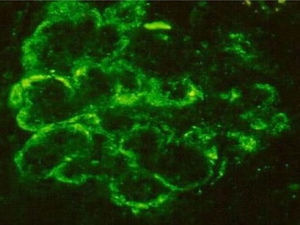
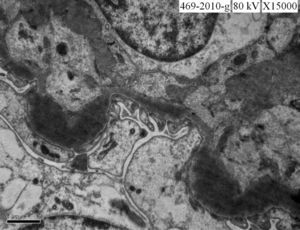
Kidney biopsy light microscopy revealed 17 glomeruli, which are enlarged and lobulated. There was increase in mesangial matrix and cellularity, capillary basement membrane was thickened with focal tramtracking (Fig. 1) suggestive of membranoproliferative glomerulonephritis and to rule out Class IV Systemic Lupus Erythematosus by immunofluorescence (IF) and electron microscopy (EM). The diagnosis of MPGN was confirmed using PAM Silver stain (Fig. 2). Immunofluorescent analysis reveals the presence of the complement protein C3 which produces a characteristic ribbon-like staining pattern of the peripheral capillary loops (Fig. 3). IF was negative for C1q and C4. Segmental staining for IgM is also seen with absent staining for IgG and IgA. EM revealed enlarged glomerulus due to diffuse cellular proliferation particularly mesangial. There was marked thickening at basement membrane which is painted with ribbon like homogenous electron dense intramembranous deposits with absent subepithelial deposits confirming the diagnosis of MPGN type II, also known as Dense Deposit Disease (Fig. 4). Meanwhile the blood culture, which was sent earlier has grown S. typhi and his urine culture was sterile. A diagnosis of S. typhi glomerulonephritis was made and he was treated with intravenous ceftriaxone as per culture and sensitivity reports. He responded promptly to ceftriaxone and after 2 weeks of therapy he became asymptomatic with complete resolution of his renal parameters.
Typhoid fever is a systemic infection with the bacterium S. enterica serotype typhi. The absence of specific symptoms or signs makes the clinical diagnosis of typhoid difficult. Blood cultures are the standard diagnostic method, they are positive in 60–80% of patients with typhoid. Culture of bone marrow is more sensitive. The result is positive in 80–95% of patients with typhoid, even patients who have been taking antibiotics for several days, regardless of the duration of illness.2 In our patient during his first admission, blood culture was negative for S. typhi and he was misdiagnosed as having tuberculosis. Therefore several samples should be examined because of the irregular nature of shedding of the bacteria.
There are various renal complications of typhoid. Cystitis, pyelonephritis, and pyelitis have been described. Dehydration if not managed correctly may lead to acute tubular necrosis. Typhoid glomerulonephritis is a rare complication affecting 2–4% of typhoid patients in endemic areas and in subjects travelling from endemic regions.3 In addition to the clinical symptoms of typhoid fever, patients with renal complications usually show edema for prolonged periods, macro- or micro hematuria, and proteinuria. In some patients signs of volume overload and hypertension are present. C3 concentrations are frequently reduced, as is IgG and IgM, although IgA values are significantly elevated, presumably due to antigenic stimulation of plasma cells within the lamina propria of the gastrointestinal tract, which is the site of entry of the bacteria. Renal biopsy has shown both mesangial proliferative glomerulonephritis4 and IgA nephropathy.5 Acute diffuse proliferative glomerulonephritis6 and crescentic IgA nephropathy7 in an HIV-positive patient with enteric salmonella infection have also been described. The glomerular disease is frequently mild and transient. Hematuria and proteinuria usually disappear within 2–3 weeks, but in others the symptoms may persist for at least 4 weeks. Consistent with this our patient showed complete recovery from his illness within 2 weeks of treatment for his typhoid fever.
Our patient had gross hematuria, nephritic range proteinuria and persistent low levels of C3 without any signs of volume overload and hypertension. His kidney biopsy revealed MPGN. The glomerular lesion in our patient is most probably immune-complex mediated as suggested by persistent low C3 and subendothelial electron dense deposits. Such a presentation has not been reported in patients with typhoid fever. This case demonstrates the value of kidney biopsy in diagnosing glomerular lesions in association with S. typhi and future directions for the new insights into the pathogenic events in typhoid glomerulonephritis.