Vascular Access is a fundamental element for the correct management of patients with Chronic Renal Insufficiency (CRI), who are included in the Haemodialysis (HD) programme.
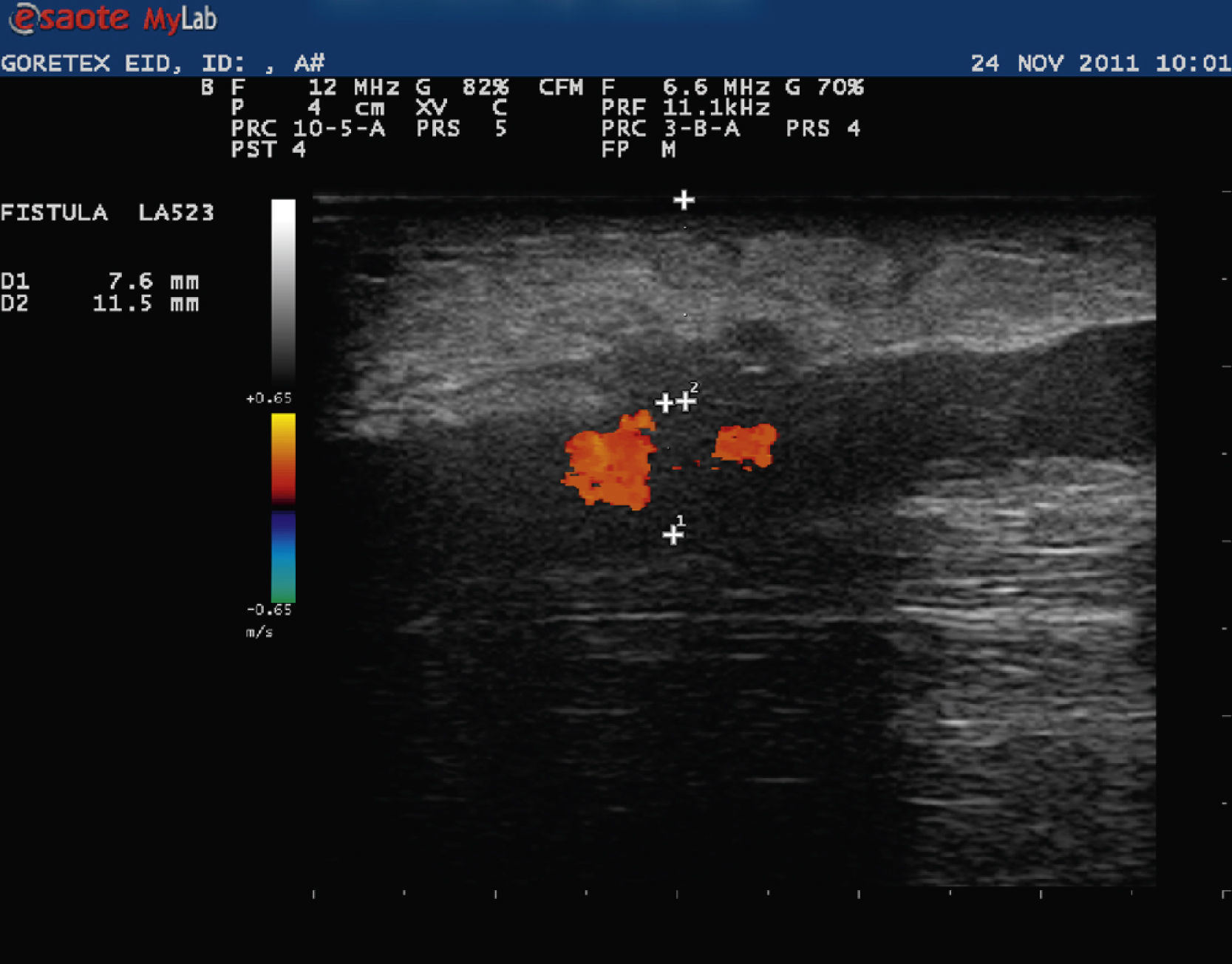
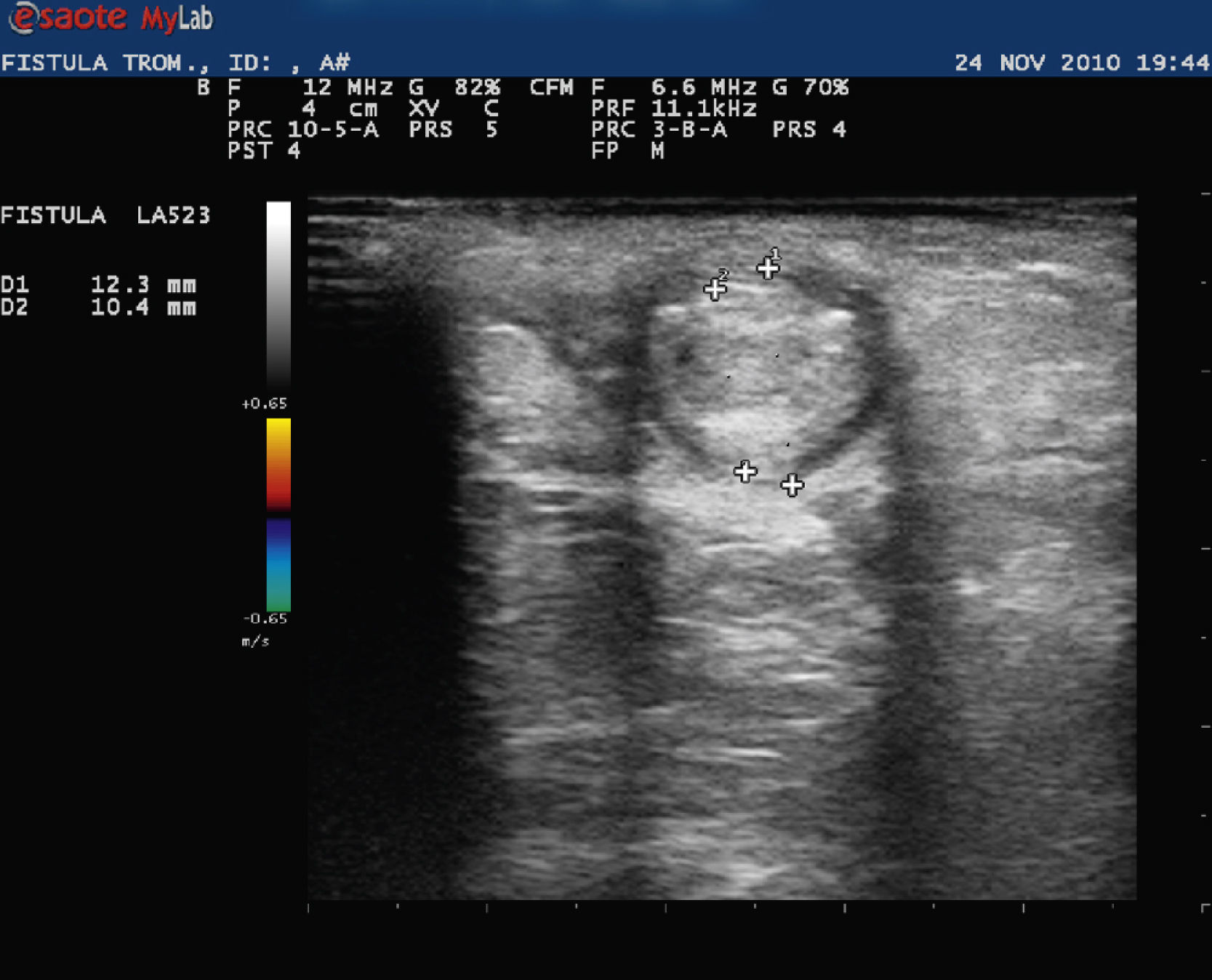
The autologous internal arteriovenous fistula (autologous IAVF) is the permanent vascular access of choice for patients who require haemodialysis. (degree of evidence a). (Figs. 1 and 2)
For these patients with CRI in HD programmes, the Vascular Access of choice is Internal Arteriovenous Fistula (IAVF), although it is not the only one. The alternative vascular access to IAVF is Arteriovenous Prosthesis (AVP), due to it being the most commonly used. The normal material used is EXPANDED POLYTETRAFLUOROETHYLENE (PTFE). The third access modality is Central Venous Catheter (CVC), both in temporary catheter and in permanent tunnelled catheter.
One of the aims of haemodialysis units is for the majority of patients to be able to start the haemodialysis via a good vascular access, which, by choice, is the autologous internal arteriovenous fistula (IAVF A). The IAVF A has an average life of 5 to 10 years’ survival. The AVP has an average life of 2 to 3 years’ survival.
Whilst haemodialysis, as a technique, has evolved spectacularly during the second half of the 20th century, no vascular access has surpassed the success and initial effectiveness of the internal arteriovenous fistula (IAVF). It has been demonstrated that the radiocephalic IAVF, described by Brescia-Cimino, is still, today, the best vascular access for haemodialysis. It has a low complication rate and it presents an excellent long-term permeability and use rate. It also satisfies the objective of ideal vascular access, as it is a peripheral access, which is easy to approach (extensive and surface venous trajectory), with sufficient flow for the haemodialysis and it offers the possibility of carrying out more proximal fistulae.
Any internal vascular access must be assessed and its evolution tracked, since creation, by the haemodialysis nursing staff of the Dialysis Unit, nephrologists and the actual patient.
During the monitoring of the access function, a systematic physical examination is compulsory before and after each haemodialysis session:
1) Direct observation, 2) Palpation, and 3) Auscultation.
ObservationEvaluate the venous trajectory, noticing the existence of haematomas, stenosis, aneurysms, pseudo-aneurysms, oedema, reddening, infected points, scabs, coldness of the limb, venous hypertension.
PalpationEvaluate the Thrill, murmur, vibration of the access in the anastomosis and the rest of the venous trajectory. And if necessary.
AuscultationEvaluate the murmur of the access and venous route by auscultation.
The haemodynamic parameters must also be assessed on a regular basis: Access flow, circuit flow, dynamic pressures and static pressures, to be able to detect changes that occur in time.
After detecting a dysfunction of the access (puncture difficulty, low flow, venous hypertension, high recirculation, etc.) or complication (suspicion of infection, aneurysms, pseudo-aneurysms, ischemia, oedema, etc.) the diagnosis must be confirmed.
A good measure to confirm the diagnosis and evolution of the vascular access, since its creation until its use, and later during the life of the IAVF, by nursing staff would be the use of ultrasound.
From the moment the access is created and matured, the control by nursing staff is important to detect possible dysfunctions. The Doppler Ultrasound can be a very important tool.
At the time of the puncture, quite a frequent complication is that difficult IAVF, due to limited maturity, limited development, stenosis in juxta-anastomotic vein and the existence of collateral, non-puncturable accessory veins, previous haematomas from earlier punctures. Even not knowing the direction of the cannulation.
Faced with these difficulties at the time of the puncture, the nursing staff must have a valid tool, such as the Doppler Ultrasound. It is a non-invasive test and with reliable results. The ultrasound is an immediate image technique. It enables us to differentiate between IAVF, soft parts, stenosis, extralumen haematomas, abscesses, aneurysms, pseudo-aneurysms and oedemas. The only diagnostic method that provides anatomic and haemodynamic information at the same time. It permits measuring the flow of the Vascular Access. The examination of the Vascular Access can be carried out with the translator both in longitudinal plane and in transverse plane (with or without colour).
The Doppler Ultrasound is a very important tool for the nursing staff, once trained in its use, because it enables us to evaluate the IAVF immediately, as it is a non-invasive procedure. As it provides us with information related to the arterial and venous permeability. Direction of flow. The existing depth between the surface of the skin and the wall of the vessel. The diameter of the vessel (measured from intima to intima). And the possibility of carrying out a guided puncture.
Further readingNational Kidney Foundation. K/DOQI Clinical Practise Guidelines for Vascular Access. Update 2000. Am. J. Kidney Dis. 37. 2001.
Manual de protocolos y procedimientos de Actuación de Enfermería Nefrológica. SEDEN. Madrid. 2001.
Consensos SEDYT. Accesos vasculares en hemodiálisis. 2007. http://www.sedyt.org
Ocharan-Corcuera J, Mayor JM, San-Vicente J, Hernández J, Jimeno I, Minguela JI, Chena A, Ruiz-de Gauna R. Uso y cuidados de los accesos venosos. Dial Traspl. 2008; 29:188-92.
Clinical Doppler Ultrasound. Alan, Dubbins. Harcourt Publishers Limited. 2000.
Hernández J. Punción con Ecografía dirigida de la Fístula Arterio-Venosa dificultosa. Dial Traspl. 2011; 32:126-7.