To investigate the association between neck circumference (NC), overweight, and metabolic syndrome (MS) in Turkish patients with type 2 diabetes.
MethodsA total of 264 diabetic patients (mean age: 52.9±8.1 years) were recruited from two centers in Istanbul to perform anthropometric measurements, including waist and hip circumference, NC, and body mass index. Blood pressure, fasting glucose, and lipid profile (total cholesterol, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, and triglyceride levels) were determined.
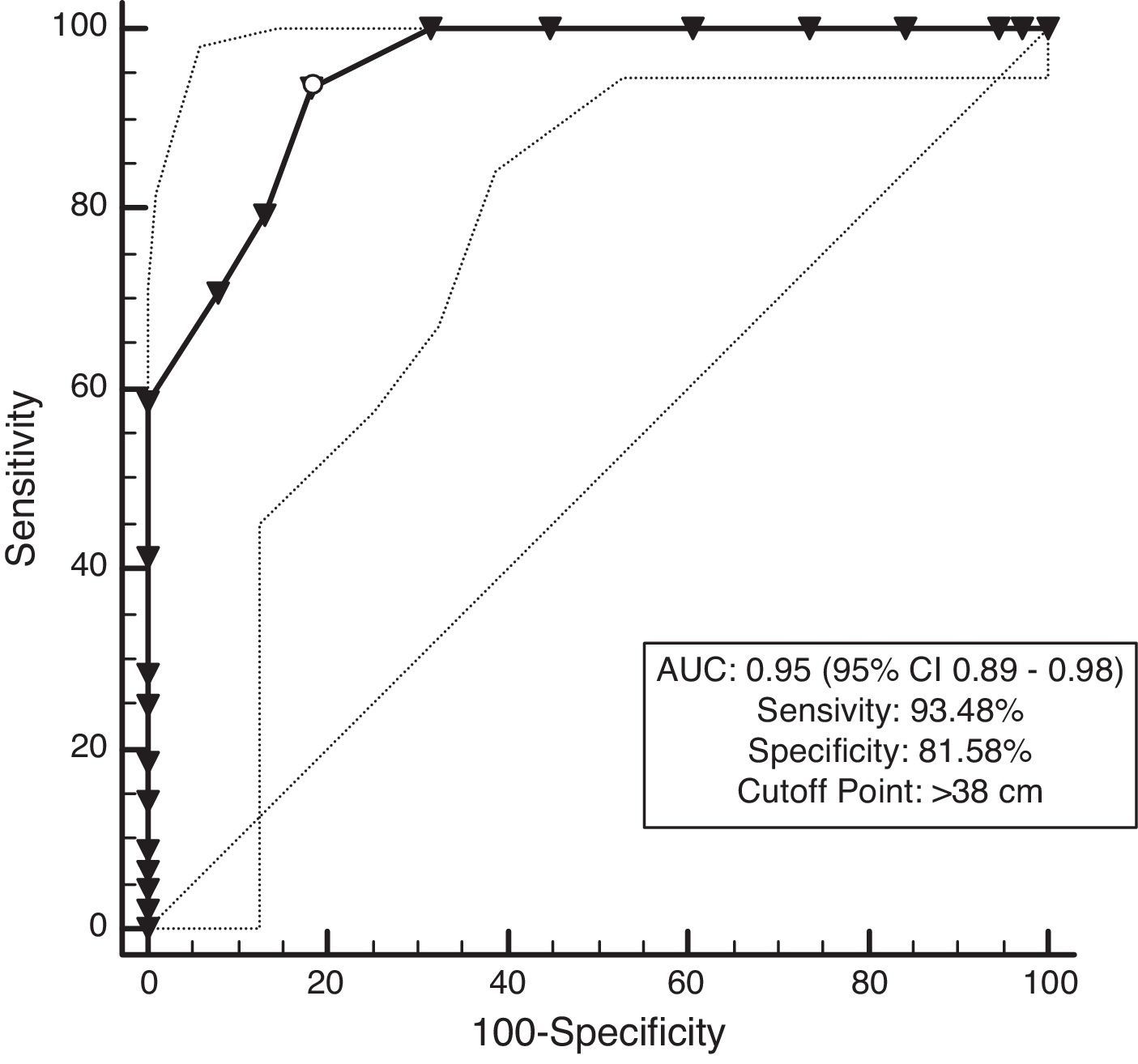
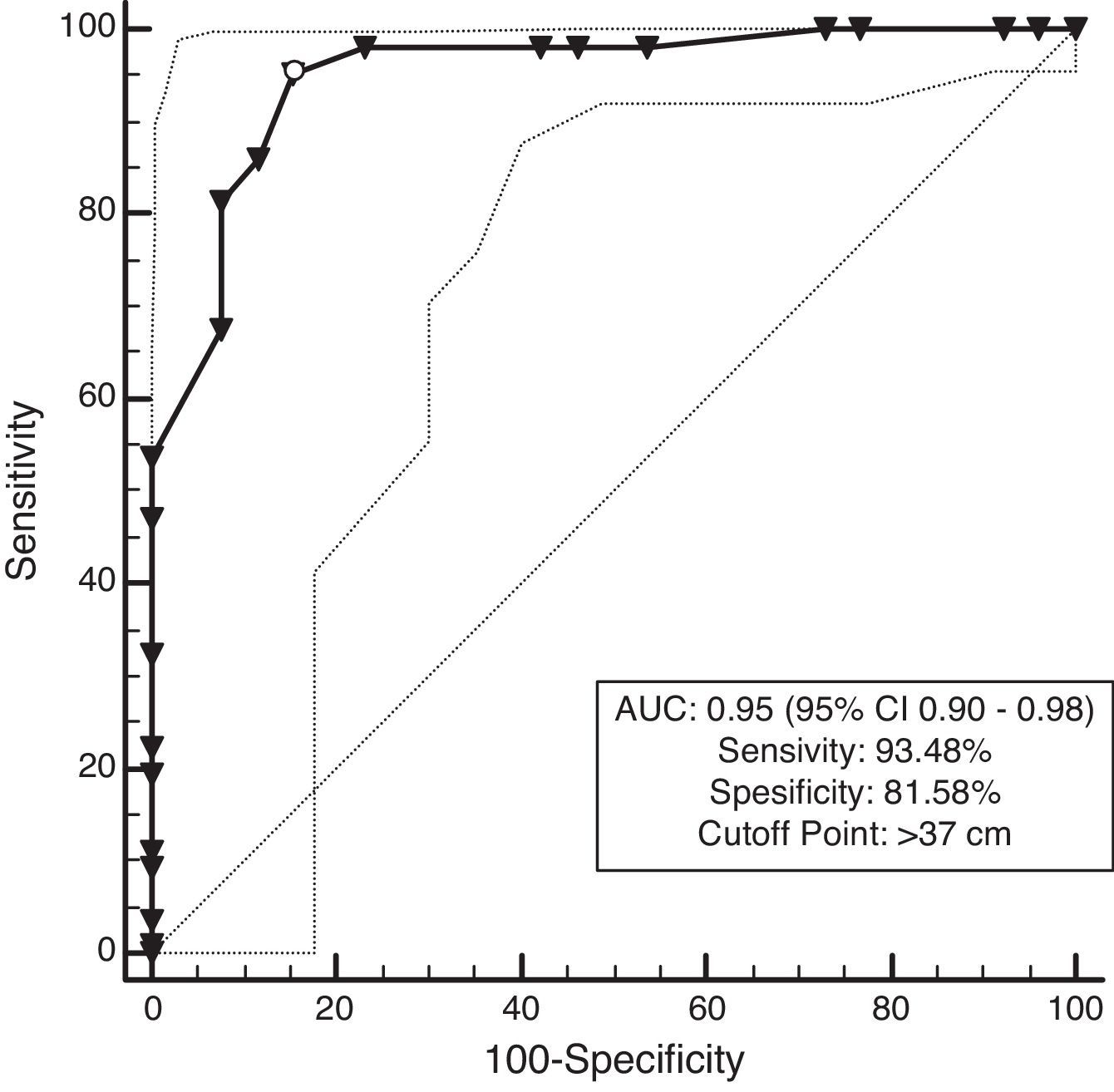
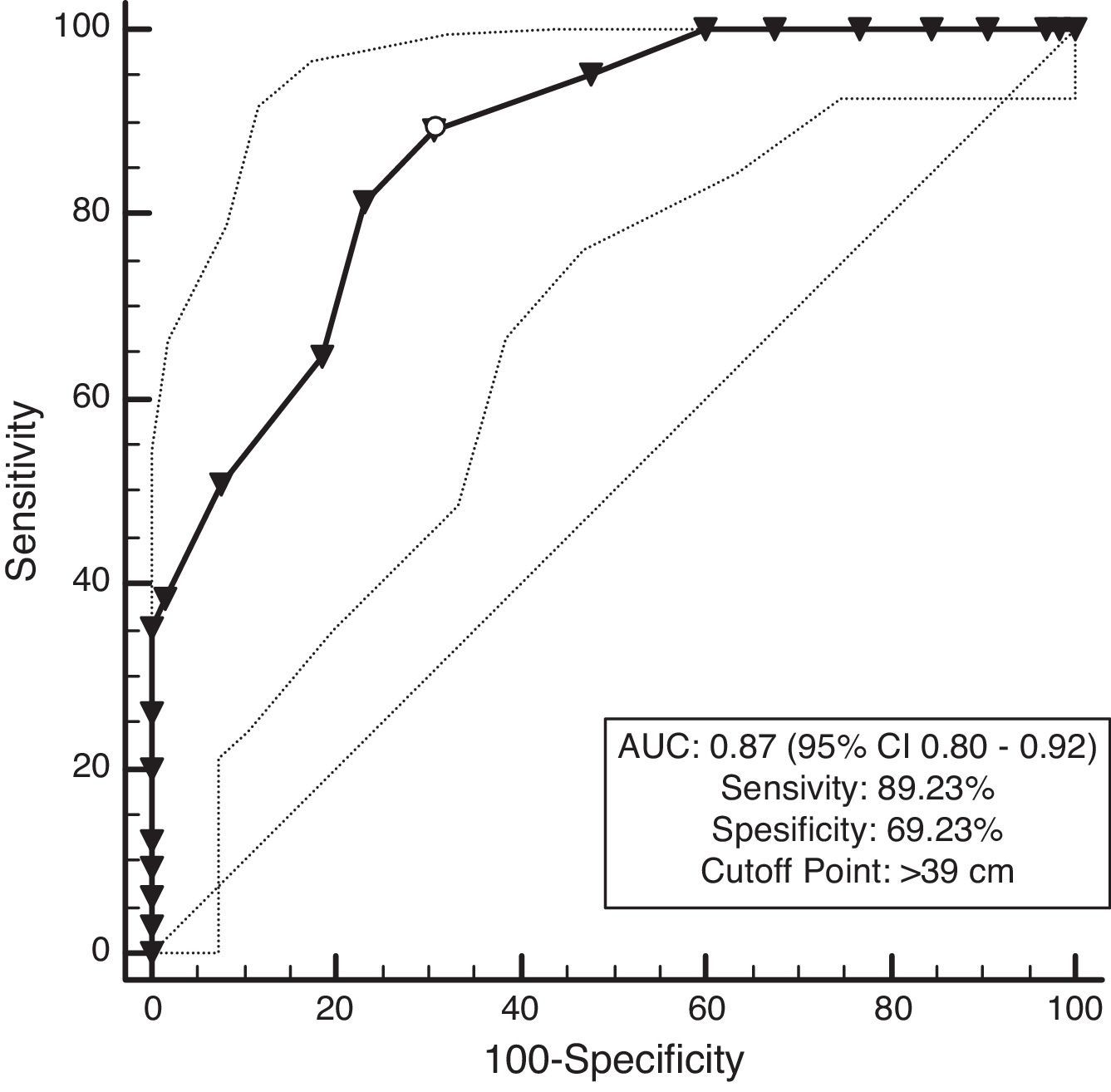
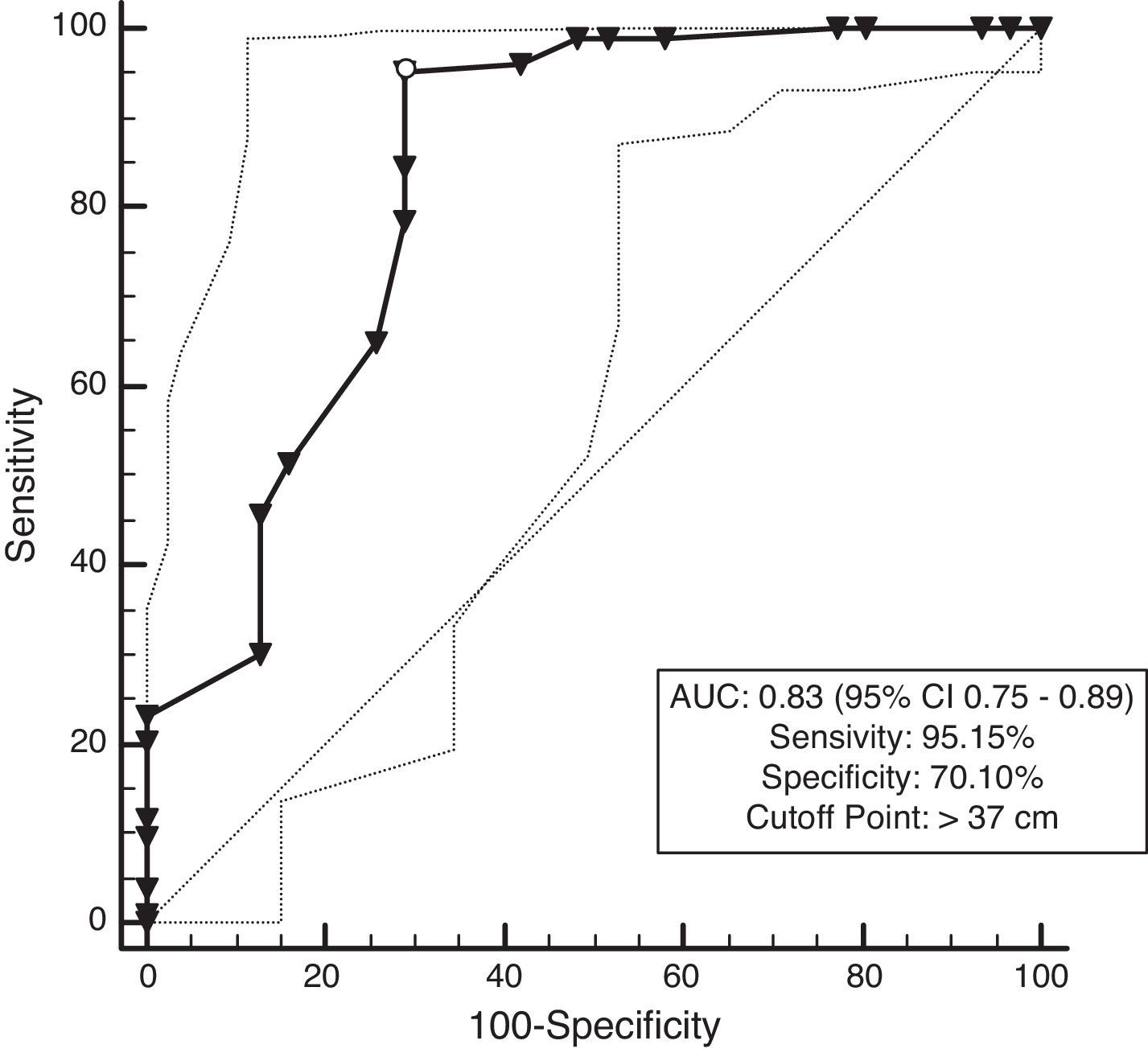
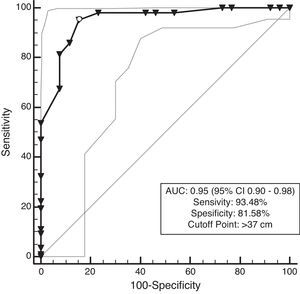
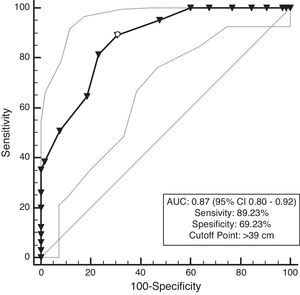
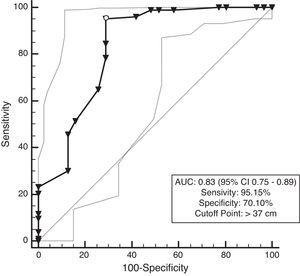
ResultsNC correlated with waist circumference, systolic blood pressure, and triglycerides in men, whereas NC only correlated with waist circumference in women. Additionally, NC was shown to negatively correlate with high-density lipoprotein cholesterol in both men and women. Receiver operating characteristic analysis showed that the area under the curve for NC and overweight was 0.95 for both men and women (P<0.001). Moreover, a NC of 38cm for men and 37cm for women was the best cut-off point for determining overweight. The area under the curve for NC and MS was 0.87 for men and 0.83 for women (P<0.001). A NC of 39cm for men and 37cm for women was the best cut-off point to determine participants with MS.
ConclusionsOur findings suggest a positive correlation of NC with MetS in Turkish patients with type 2 diabetes, and could be a useful and accurate tool to identify MS.
Investigar la asociación entre el perímetro del cuello (PC), el sobrepeso y el síndrome metabólico (SM) en pacientes turcos con diabetes tipo 2.
MétodosSe reclutó un total de 264 pacientes diabéticos (edad media: 52,9±8,1 años) de 2 centros de Estambul a quienes se realizaron medidas antropométricas, incluidas las de los perímetros de la cintura y la cadera, el PC y el índice de masa corporal. Se determinaron la presión arterial, la glucosa en ayunas y el perfil lipídico (colesterol total y de las lipoproteínas de alta y baja densidad y triglicéridos).
ResultadosEl PC se correlacionaba con el perímetro de la cintura, con la presión arterial y con los triglicéridos en los varones, pero solo con el perímetro de la cintura en las mujeres. Se comprobó además una correlación negativa del PC con el colesterol de las lipoproteínas de alta densidad tanto en varones como en mujeres. El análisis de las características operativas del receptor mostró que el área bajo la curva del PC y el sobrepeso era de 0,95 tanto en varones como en mujeres (p<0,001). Además, un PC de 38cm en varones y de 37cm en mujeres era el mejor punto de corte para determinar los participantes con sobrepeso. El área bajo la curva del PC y el SM era 0,87 en los varones y de 0,83 en las mujeres (p<0,001). Un PC de 39cm en varones y de 37cm en mujeres era el mejor punto de corte para determinar los participantes con SM.
ConclusionesNuestros hallazgos indican una correlación positiva del PC con el SM en los pacientes turcos con diabetes tipo 2, que podría ser una herramienta útil y exacta para identificar el SM.
Metabolic syndrome (MetS) is a condition, which causes an increase in cardiovascular mortality and morbidity.1–3 In 2005, IDF (International Diabetes Federation) defined MetS, which is appropriate for clinical use worldwide,4 as central obesity plus two of the following four additional factors: elevated plasma triglycerides (TG), reduced high-density-lipoprotein-cholesterol (HDL-C), elevated blood pressure (BP), and elevated fasting plasma glucose (FBG).4 Based on this definition, central obesity is an absolute necessity for MetS and is determined by waist circumference (WC) values. The cutoff points for central obesity in Europeans were ≥94cm for males and ≥80cm for females.4
In 2009, IDF/IAS (International Atherosclerosis Society)/IASO (International Association for the Study of Obesity) established the most recent MetS criteria.5 It was agreed that central obesity should not be an obligatory component for determining MetS however; WCs should be continued to be used a useful preliminary screening tool. Three out of the five abnormal findings would be considered for qualifying a person with MetS. In this report, different WC cutoff points were defined for national or regional populations.5
Already, it has been demonstrated that there is a strong correlation between neck circumference (NC) and WC and that it may be used as an indicator of central obesity.6–11 In addition, the association between NC and MetS has also been revealed in different communities.12–19 Similarly, Onat et al.20 determined the association between MetS and NC in the Turkish population and defined a cutoff value. However, no study has been conducted to determine the association between NC and MetS in type 2 diabetes to date.
Therefore, the aim of this study was to evaluate the association between NC and MetS and to establish cutoff values of NC for the prediction of MetS in Turkish type 2 diabetic patients.
MethodsIn this study, a total of 289 type 2 diabetic patients were enrolled between January and December 2015 from the outpatient clinics of internal medicine at a Istanbul University Cerrahpasa Faculty of Medicine and Istanbul Florence Nightingale Hospital in Istanbul. Written informed consent was obtained from all participants, and the study was approved by the institutional review board and complied with the Declaration of Helsinki. Past medical history was determined using a standardized questionnaire.
Participants with a history of thyroid disease and malignancy (n=3), pregnancy (n=1), liver failure (n=1), renal failure (n=1), heart failure (n=1), goiter (n=5), females undergoing hormone replacement therapy (n=1) and diabetic patients with bad metabolic control (>7.5% HbA1c) (n=12) were excluded. Ultimately, the evaluation was made using 264 patients (134 women and 130 men).
Blood pressure (BP) was measured twice after each participant had been seated for 10min, and the average was used for analysis. Anthropometric measurements, including height, weight, WC, hip circumference, and NC, were performed. All measurements were conducted by two different observers on two separate days, and the mean of these values was calculated. Thus, any error involving intra and interobserver variability was prevented. The measurements were obtained in light clothes, under fasting, standing, and barefoot conditions and at the end of expiration. Weight was measured using a digital scale to within 0.1kg with only undergarments, and height was determined using a portable stadiometer with an accuracy to within 1mm in barefeet. WC was measured using a non-elastic tape with the subject in a standing position. The abdominal circumference midway between the lowest rib and the top of the iliac crest at the end of expiration was measured to obtain the WC. Hip circumference was measured at the level of the greater trochanters with the legs closed together.21,22 NC was measured on the middle of the neck, between the mid cervical spine and the mid anterior neck, to within 0.5mm with non-stretchable plastic tape. In men with a laryngeal prominence (Adam's apple), it was measured just below the prominence. While taking this parameter, the participant was asked to look straight ahead with shoulders down, but not hunched.10 Fasting glucose and lipid profiles (i.e., total cholesterol, HDL-C, low-density lipoprotein cholesterol [LDL-C], and TG) were determined using an autoanalyzer (Roche Cobas 6000, Hitachi High Technology Corp. Tokyo). The body mass index (BMI) was calculated as weight (kg) divided by the square of height (m). The waist to hip ratio (W/H) was calculated as the WC divided by the hip circumference.
Overweight was defined as a BMI of 25–29.9kg/m2, and abdominal obesity was defined as a WC of ≥94cm (men) and ≥80cm (women).5 MetS was defined based on the IDF/IAS/IASO harmonizing criteria as the presence of any three out of the five following risk factors5: elevated WC (≥94cm in males and ≥80cm in females); raised TG (>150mg/dL or 1.7mmol/L) or current treatment for this condition; decreased HDL-C (40mg/dL or 1.03mmol/L in males and 50mg/dL or 1.29mmol/L in females) or current treatment for HDL-C; elevated blood pressure (systolic BP≥130mmHg or diastolic BP≥85mmHg) or treatment of previously diagnosed hypertension; and raised fasting plasma glucose (≥100mg/dL or 5.6mmol/L) or treatment of previously diagnosed type 2 diabetes.
Statistical analysisDescriptive parameters were shown as estimated mean±standard deviation or in percentages. Two-sided t-tests and Pearson's chi-square tests were used to analyze the differences between the means and proportions of groups. Odds Ratio (OR) and 95% confidence intervals (CI) were obtained using logistic regression analyses. Receiver operating characteristics (ROC) curve analyses were also performed. The Youden index defined as “sensitivity+specificity−1,” was used to determine the optimal cutoff points. P value <0.05 was considered statistically significant. The statistical analysis was conducted using IBM SPSS Statistics, Version 21 (IBM Corporation, Armonk, NY, USA).
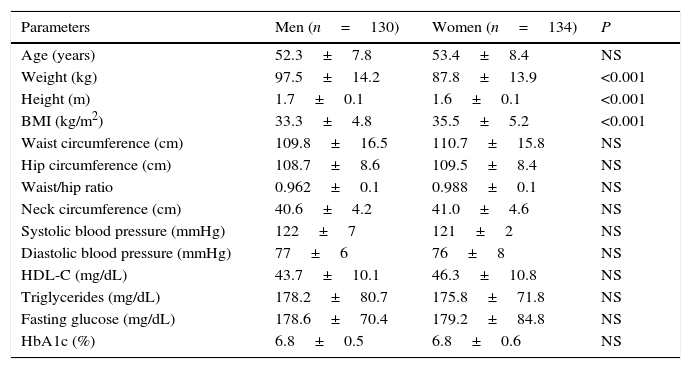
ResultsThe study sample comprised 264 individuals, including 130 men and 134 women with a mean age of 52.9±8.1 years. MetS was identified in 65 (50%) men and 103 (76.8%) women. The main characteristics of the study population are presented in Table 1. All parameters, except weight, height, and BMI, were similar between the genders.
Baseline study sample characteristics.
| Parameters | Men (n=130) | Women (n=134) | P |
|---|---|---|---|
| Age (years) | 52.3±7.8 | 53.4±8.4 | NS |
| Weight (kg) | 97.5±14.2 | 87.8±13.9 | <0.001 |
| Height (m) | 1.7±0.1 | 1.6±0.1 | <0.001 |
| BMI (kg/m2) | 33.3±4.8 | 35.5±5.2 | <0.001 |
| Waist circumference (cm) | 109.8±16.5 | 110.7±15.8 | NS |
| Hip circumference (cm) | 108.7±8.6 | 109.5±8.4 | NS |
| Waist/hip ratio | 0.962±0.1 | 0.988±0.1 | NS |
| Neck circumference (cm) | 40.6±4.2 | 41.0±4.6 | NS |
| Systolic blood pressure (mmHg) | 122±7 | 121±2 | NS |
| Diastolic blood pressure (mmHg) | 77±6 | 76±8 | NS |
| HDL-C (mg/dL) | 43.7±10.1 | 46.3±10.8 | NS |
| Triglycerides (mg/dL) | 178.2±80.7 | 175.8±71.8 | NS |
| Fasting glucose (mg/dL) | 178.6±70.4 | 179.2±84.8 | NS |
| HbA1c (%) | 6.8±0.5 | 6.8±0.6 | NS |
kg: kilogram, m: meter, BMI: body mass index, cm: centrimeter, mm: millimeter, Hg: mercury, mg: milligram, dL: deciliter, NS: nonsignificant.
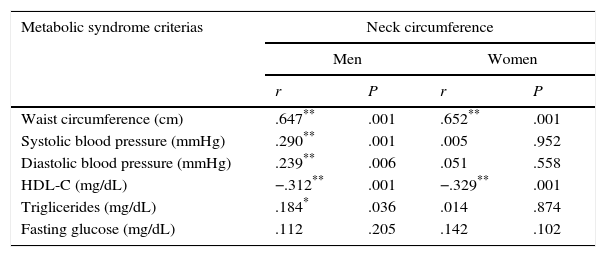
NC was 40.6±4.2cm and 41.0±4.6cm among 130 men 134 women, respectively. There were no significant differences (P>0.05) between men and women for NC. Correlations between NC and MetS markers are presented in Table 2. NC was associated with WC, systolic BP, and TG in men, whereas it was correlated with only WC in women. Additionally, NC exhibited a negative correlation with HDL-C in both men and women.
Correlations between the neck circumference and metabolic syndrome criterias.
| Metabolic syndrome criterias | Neck circumference | |||
|---|---|---|---|---|
| Men | Women | |||
| r | P | r | P | |
| Waist circumference (cm) | .647** | .001 | .652** | .001 |
| Systolic blood pressure (mmHg) | .290** | .001 | .005 | .952 |
| Diastolic blood pressure (mmHg) | .239** | .006 | .051 | .558 |
| HDL-C (mg/dL) | −.312** | .001 | −.329** | .001 |
| Triglicerides (mg/dL) | .184* | .036 | .014 | .874 |
| Fasting glucose (mg/dL) | .112 | .205 | .142 | .102 |
cm: centrimeter, mm: millimeter, Hg: mercury, HDL-C: high density lipoprotein-cholesterol, mg: milligram, dL: deciliter, NS: nonsignificant.
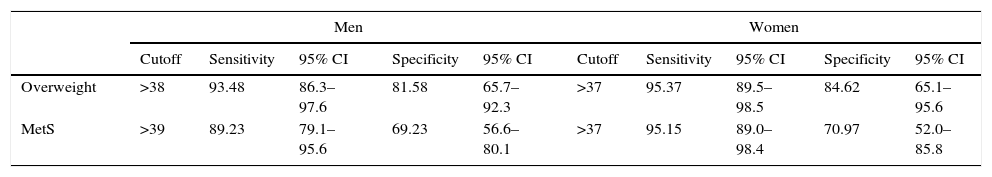
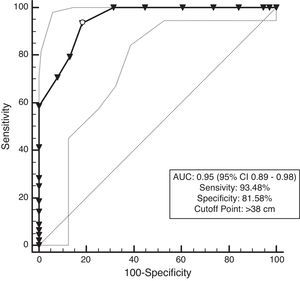
The ROC curves are presented in Figs. 1–4. All the AUCs for NC were statistically significant (P<0.001). The prevalence of overweight individuals was 75.7%. NC in the overweight group was 42.4±3.4cm. An NC of >38cm for men and >37cm for women was the optimal cutoff point for determining overweight participant (P<0.001) (Table 3). The AUC was 0.95 for both men and women (Figs. 1 and 2).
Cutoff values for determining the type 2 diabetic patients with overweight and MetS according to ROC analysis.
| Men | Women | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Cutoff | Sensitivity | 95% CI | Specificity | 95% CI | Cutoff | Sensitivity | 95% CI | Specificity | 95% CI | |
| Overweight | >38 | 93.48 | 86.3–97.6 | 81.58 | 65.7–92.3 | >37 | 95.37 | 89.5–98.5 | 84.62 | 65.1–95.6 |
| MetS | >39 | 89.23 | 79.1–95.6 | 69.23 | 56.6–80.1 | >37 | 95.15 | 89.0–98.4 | 70.97 | 52.0–85.8 |
The prevalence of MetS was 63.6%, and participants with MetS (168) had a 5.3cm wider NC than those without MetS (96) (42.7–37.4cm; P<0.001). The ROC analysis showed that the AUC for NC and MetS was 0.87 for men and 0.83 for women. The optimal NC cutoff value was >39cm for men, and it was >37cm for women. (P<0.001) (Figs. 3 and 4, Table 3).
After completing the logistic regression analysis, considering MetS and overweight as dependent variables and NC as an independent variable, the results showed that the relationship between NC and MetS (odds ratio: 1.67 [95% CI: 1.47–1.91]; P<0.001) and between NC and those who were overweight (odds ratio: 2.33 [95% CI: 1.85–2.93]; P<0.001) were statistically significant.
DiscussionThis study among Turkish type 2 diabetic patients showed that an NC >38cm for men and >37cm for women was the optimal cutoff point to determine overweight participants. An NC of >39cm for men and >37cm for women was the optimal cutoff point to determine participants with MetS.
NC measurements were significantly associated with WC in both men and women. Additionally, NC was significantly associated with systolic BP and TG only in men. There was also a significant negative association between NC and HDL-C (one of the important parameters of MetS) both in women as well as in men. Zhou et al. determined similar results as they found a positive correlation between NC and BP. Additionally, FBG and TG negatively correlated with HDL-C in both males and females.13
Our results indicate that an increase in NC and WC increases the chance of developing MetS by 1.67- and 2.33-fold for males and females, respectively. A Brazilian MetS study found that an increase in NC increased the likelihood of MetS for female by 1.13-fold but had no association in men.17 The same study also found that an enlargement in WC increased the likelihood of MetS by 1.08-fold in females and by 1.16-fold in men.17 The reason for the discrepancies between the results of this study and our findings may be because of the fact that our entire study population comprised diabetic patients.
In studies performed in different age groups in various communities, different NC cutoff levels were defined for overweight and obese persons.16,23–25 Similar data were identified for Turks, and NC of 29, 32.5, 28, and 31cm determined Turkish overweight boys, obese boys, overweight girls, and obese girls, respectively.26
The correlation between MetS and NC and the cutoff values for MetS have been studied in different communities and groups of age, and various cutoff values were determined.12,25–28 Specifically in Turks, NC cutoff value of ≥39cm for men and ≥35cm for women were considered as MetS indicator (20). In the present study, we have only determined NC cutoff values in men and women with diabetes. Yang et al. determined NC cutoff values for MetS in Chinese diabetic patients as ≥39cm for men and ≥35cm for women.25 Our results were similar for men but were higher for women by 2cm. Another study in which 29% of the study samples comprised type 2 diabetic patients presented NC cutoff values of 39.6cm for men and 36.1cm for women for the prediction of MetS.17
The other studies that have determined NC cutoff values were community-based, and the values obtained are similar to our data, despite the fact that there has not been any other study that has examined diabetic patients exclusively.12,17,20
The mechanisms underlying the association between metabolic disorders, cardiometabolic risk, and NC have not precisely identified. The increase in the lipolytic activities of upper body fat, obesity, and free fatty acids because of insulin resistance related to obesity, increase in very low-density lipoprotein cholesterol (VLDL-C) production, oxidative stress, and vascular damage may be potential underlying factors of MetS.29–30 It has been shown that there was free fatty acid release into the systemic circulation from the upper body subcutaneous tissue in obese persons.31 Diabetes is also associated with insulin resistance and other metabolic abnormalities.
WC has been established as a useful measurement for determining central obesity and is essential for the IDF MetS criteria. However, WC measurements may be affected by cultural and environmental factors. The room temperature, clothing, as well as sociocultural and religious hindrances for undressing may prevent the performance of an accurate measurement. In addition, dyspepsia may also lead to obtaining inaccurately high measurements. The results of this study, indicate an independent association between NC and MetS. Specifically, NC is a simple method that can be used to identify MetS in type 2 diabetic patients.
This study had certain limitations: 1) this study was performed in only two centers, and therefore, it may not reflect the entire population of Turkey; 2) our data may not accurately represent other communities and ethnic groups because it was performed exclusively on Turks; and 3) our data cannot be extrapolated to the overall population as it comprised only diabetic patients. Therefore, further study is warranted considering these factors.
ConclusionsIn conclusion, this study demonstrated that NC was associated with MetS in Turkish type 2 diabetic patients. Thus, NC might be a useful and accurate tool to identify MetS in type 2 diabetic patients.
Ethics approval and consent to participateAll procedures performed in studies involving human participants were conducted in accordance with the ethical standards of the Istanbul University Cerrahpasa Faculty of Medicine Ethical Committee Protocol Number: 28463/November 1, 2013 and the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Author contributionsİsmail Özkaya wrote the manuscript, designed the study and collected data. Emine Kır Biçer and Bülent Yardimci contributed to the writing of the manuscript and collected data. Aydın Tunckale contributed to designed study, performed statistical analysis and the interpretation
Conflict of interestThe authors declare that they have no conflicts of interest.
There is no acknowledgements.