Thyroid hormones play an important role in body weight regulation. In this study, we investigated which body composition parameters cause a change in body weight after total thyroidectomy.
Materials and methodWe performed a retrospective cohort study of a prospectively maintained database of patients who underwent total thyroidectomy. Demographics, thyroid function tests, indications for surgery, final pathology, and postoperative thyroid status were collected. Body composition analyses measured by the bioelectrical impedance analysis method were recorded at two-time points, 12 months apart.
ResultsForty-four patients were included in the study with a mean age of 51.6 years. There were statistically significant increases in weight (p=0.049), body mass index (p=0.021), and fat mass (p=0.001) over time. While 12 patients (27.3%) lost or maintained weight, 32 patients (72.7%) gained weight. There was no significant difference in age, sex, preoperative thyroid function tests, postoperative thyroid status, or pathology between those who gained weight and those who did not. Although changes in all body composition parameters were higher in males than in females, these differences were not significant overall. Multivariable regression analysis revealed a significant positive relationship between increase in fat mass and baseline free-T3 (p=0.041) and found that lower baseline percent body fat was a significant factor for greater fat mass gain (p=0.016). However, no predictors of change in weight were identified.
ConclusionWe conclude that total thyroidectomy results in a significant change in body weight and fat mass. Higher free-T3 and lower percent body fat at baseline were significant factors of fat mass gain.
Las hormonas tiroideas juegan un papel importante en la regulación del peso corporal. En este estudio, investigamos qué parámetro de la composición corporal provoca un cambio en el peso corporal después de la tiroidectomía total.
Materiales y métodosRealizamos un estudio de cohorte retrospectivo de una base de datos mantenida prospectivamente de pacientes que se sometieron a tiroidectomía total. Se recogieron datos demográficos, pruebas de función tiroidea, indicaciones de cirugía, afección final y estado tiroideo postoperatorio. Los análisis de composición corporal medidos por el método de análisis de impedancia bioeléctrica se registraron en 2 momentos, con 12 meses de diferencia.
ResultadosCuarenta y cuatro pacientes fueron incluidos en el estudio con una edad media de 51,6 años. Hubo aumentos estadísticamente significativos en el peso (p=0,049), el índice de masa corporal (p=0,021) y la masa grasa (p=0,001) a lo largo del tiempo. Mientras que 12 pacientes (27,3%) perdieron o mantuvieron el peso, 32 pacientes (72,7%) aumentaron de peso. No hubo diferencias significativas en la edad, el sexo, las pruebas de función tiroidea preoperatorias, el estado tiroideo postoperatorio o la afección entre los que aumentaron de peso y los que no. Aunque los cambios en todos los parámetros de composición corporal fueron mayores en los varones que en las mujeres, estas diferencias no fueron significativas en general. El análisis de regresión multivariable reveló una relación positiva significativa entre el aumento de la masa grasa y la T3 libre basal (p=0,041), y encontró que un porcentaje de grasa corporal inferior al basal era un factor significativo para una mayor ganancia de masa grasa (p=0,016). Sin embargo, no se identificaron predictores de cambio de peso.
ConclusiónConcluimos que la tiroidectomía total produce un cambio significativo en el peso corporal y la masa grasa. Una mayor cantidad de T3 libre y un menor porcentaje de grasa corporal al inicio del estudio fueron factores significativos del aumento de masa grasa.
Thyroid hormones play an important role in the regulation of metabolism and in a variety of developmental processes.1 Thyroid dysfunction and thyroid surgeries have significant effects on changes in body weight and body composition.2 Hyperthyroidism causes a hypermetabolic state characterised by weight loss, while thyroidectomy and hypothyroidism are associated with reduced metabolic activity and weight gain.1,3
Total thyroidectomy is a common surgical procedure performed for various benign and malignant thyroid disorders. Several studies have reported a significant weight gain following the treatment of hyperthyroidism, whether by antithyroid drugs, radioiodine ablation, or thyroidectomy. However, the effect of thyroidectomy in patients who are euthyroid or hypothyroid at presentation is controversial.4–6 Furthermore, these findings are largely based on results from previous retrospective studies that focused only on the change in body weight and body mass index (BMI) or are limited by the use of self-reported measurements.4,5,7
There is a complex relationship between thyroid hormones and body composition. Thyroid hormones regulate metabolism and growth through actions in the liver, fat, muscle, and bone. Therefore, using body weight or BMI to analyse the effect of thyroidectomy on overall body composition reduces the complexity of the human body to one basic parameter.8 In this study, we aimed to evaluate body composition changes measured by bioelectrical impedance analysis (BIA) after one year since total thyroidectomy and to examine whether this relationship differs between male and female patients, as well as between various patient-related factors.
Material and methodsStudy design and patientsWe performed a retrospective review of a prospectively maintained thyroid surgery database of operations performed from January 2015 to December 2018. Adult patients (age ≥18 years) who underwent total thyroidectomy were included in the analysis. Patients who had no preoperative or one-year postoperative body composition analyses and had other malignancies or body weight-modifying chronic conditions (pregnancy or bariatric surgery) and were using medications that influence body weight, such as anti-obesity drugs, glucocorticoids, or topiramate during the follow-up period, were excluded from the study. The study was approved by the Ethics Committee of the Ankara University School of Medicine (approval number: I7-480-20).
Data collectionDemographic parameters, preoperative thyroid function tests, indication for surgery, and postoperative thyroid status were recorded. Pathological diagnosis was determined by histological examination and obtained from the final pathology report. Data on whether patients received radioactive iodine (RAI) therapy were collected. Preoperative and one-year postoperative body composition analyses were recorded.
Free triiodothyronine (T3), free thyroxine (T4), and thyroid stimulating hormone (TSH) concentrations were measured in fasting morning samples using the chemiluminescence technique (Access DXI800, Beckman Coulter Diagnostics, Brea, California, USA). Reference ranges for thyroid function tests were as follows: free T3 3.5–6.5pmol/L, free T4 11.5–22.7pmol/L, and TSH 0.5–4.8μIU/mL.
Weight and body composition, including total body water, fat mass, free fat mass (FFM), muscle mass, and bone mass, were measured by BIA using TANITA BC-420 S (Tanita Corp., Tokyo, Japan). Measurements were taken at least 3h after waking, 3h after eating, and with an empty bladder. All patients were weighed without shoes and in light indoor clothing. Height was measured without shoes on a wall-mounted stadiometer and recorded to the nearest 0.5cm. BMI was calculated as weight in kilograms divided by height in metres squared. These measurements were performed in the same way at both baseline (preoperative) and after one year of follow-up.
Follow-upAfter the surgical procedure, all patients were placed on levothyroxine replacement or suppression therapy postoperatively, according to benign or malignant surgical outcome, and all patients were managed according to the 2015 American Thyroid Association guideline.9
Statistical analysis and sample sizePower analysis was performed using the G*Power software, version 3.1.9.6 to estimate the adequate number of participants needed for this study.10 A sample size calculation was performed based on pilot data of 10 patients. It was determined that if the mean weight change one year after the surgical procedure was 2.2±4.8kg, we would need to enrol at least 40 subjects to be able to reject the null hypothesis with a probability (power) of 0.80 and a type 1 error of 0.05.
Descriptive statistics were presented as means±standard deviation (range) and frequency of observations (%). Examinations of normal distribution assumptions for continuous variables were visually assessed with quartile-quartile plots and histograms and confirmed with the Shapiro–Wilk test. Associations between variables were evaluated using the Student's t-test or Whitney U test (for continuous variables) and the Pearson χ2 or Fisher exact tests (for categorical variables), where appropriate. Depending on the data distribution, the paired t-test or Wilcoxon signed-rank test was used to compare the differences between the preoperative and one-year postoperative body composition parameters. Independent variables with a significance of p<0.20 in the univariate analysis were entered into a backward stepwise multivariable regression model. For the linear regression model, the data were presented as β coefficients with 95% confidence intervals (CIs). All tests were two-sided and a p value <0.05 was considered statistically significant.
Data were extracted from the database and imported into the Statistical Package for the Social Sciences (SPSS) for Windows, version 16.0 (SPSS Inc., Chicago, USA) for analysis. Figures were created using GraphPad Prism version 8.0.0 for Windows (GraphPad Software Inc., California, USA).
ResultsA total of 44 patients who underwent total thyroidectomy and had both baseline and one-year postoperative body composition measurements available for comparison were identified. The mean age of the study cohort was 51.6±11.7 years and 81.8% were female. A total of 31 patients (70.5%) were euthyroid, six (13.6%) were hypothyroid, and seven (15.9%) were hyperthyroid on presentation with a mean TSH of 1.7μIU/mL, with a mean free T3 of 5.1pmol/L, and with a mean serum free T4 of 12.5pmol/L at baseline.
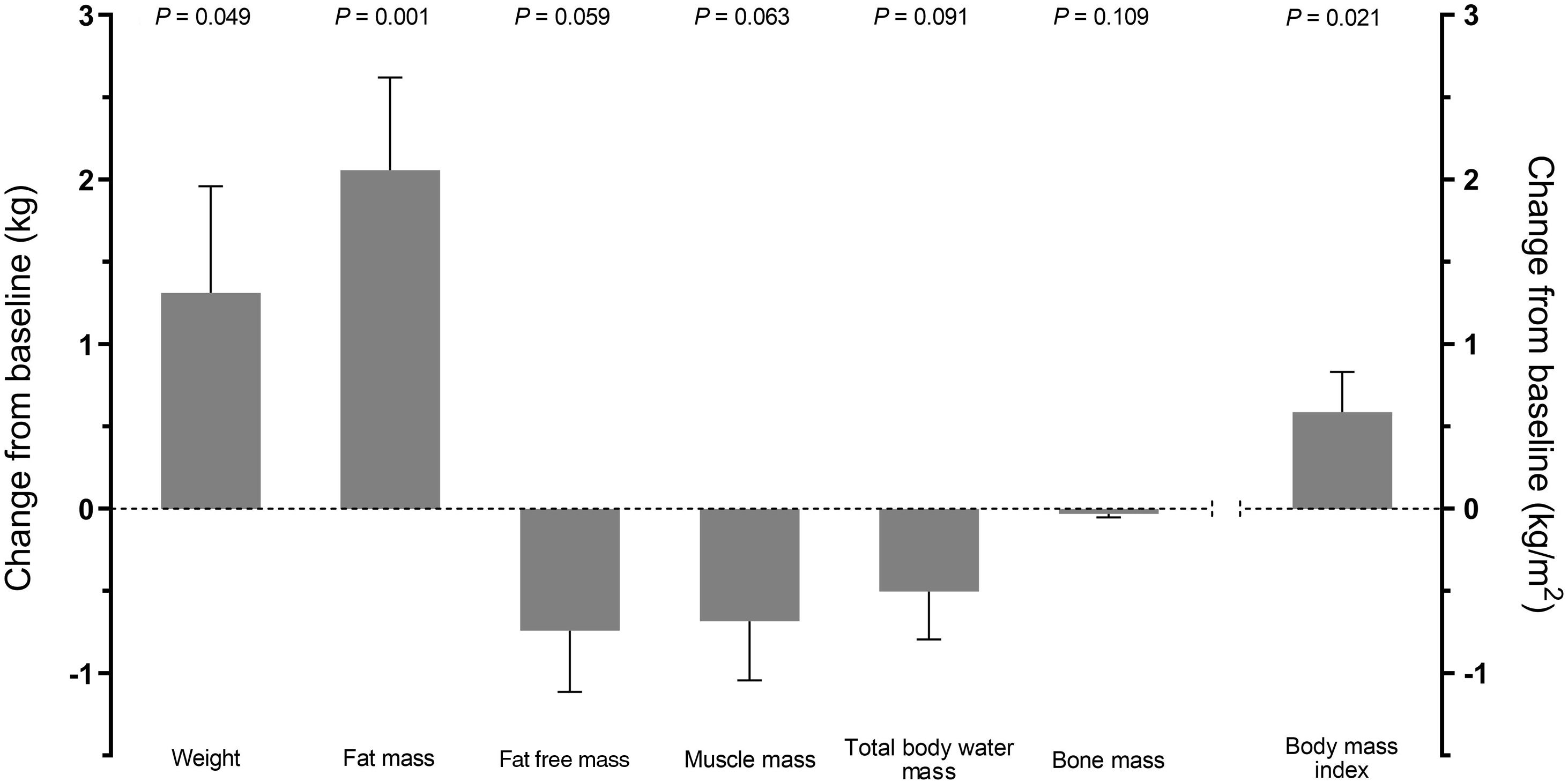
Baseline and one-year body composition measurements of patients are summarised in Table 1. The mean preoperative weight and BMI for the entire cohort were 77.3±13.8kg and 30.6±6.2kg/m2, respectively. There were statistically significant increases in weight (from 77.3 to 78.6kg), BMI (from 30.6 to 31.2kg/m2), and fat mass (from 28.8 to 30.9kg) over time (p=0.049, p=0.021, and p=0.001; respectively). For FFM, muscle mass, total body water, and bone mass, nonsignificant modest decreases were observed (Fig. 1). The results of the effect of various factors on a change in fat mass are shown in Fig. 2. There was no relationship between the change in fat mass and sex, preoperative thyroid function, BMI group, final pathology, postoperative RAI treatment, or postoperative thyroid status.
Body composition measurements of the patients before and 12 months after total thyroidectomy.
| Variables | Baseline | Follow-up | p value |
|---|---|---|---|
| Height (m) | 1.59±0.77(range, 1.47–1.74) | ||
| Weight (kg) | 77.3±13.8(range, 54.2–108.0) | 78.6±14.2(range, 53.5–109.1) | 0.049 |
| Body mass index (kg/m2) | 30.6±6.2(range, 20.9–46.6) | 31.2±6.4(range, 20.9–49.1) | 0.021 |
| Fat mass (kg) | 28.8±10.8(range, 7.2–52.5) | 30.9±10.8(range, 12.3–56.1) | 0.001 |
| Fat free mass (kg) | 48.5±6.6(range, 35.9–67.0) | 47.7±6.5(range, 36.1–66.5) | 0.053 |
| Muscle mass (kg) | 46.0±6.2(range, 34.1–63.7) | 45.3±6.2(range, 34.2–63.2) | 0.063 |
| Total body water (kg) | 34.4±5.2(range, 23.9–48.4) | 33.9±5.2(range, 24.2–49.0) | 0.091 |
| Bone mass (kg) | 2.5±0.3(range, 1.8–3.3) | 2.4±0.3(range, 1.9–3.3) | 0.109 |
When we analysed differences in body composition changes between female and male patients undergoing total thyroidectomy, there was an increase in mean weight (0.7kg vs. 4.0kg, p=0.051), BMI (0.4kg/m2 vs. 1.5kg/m2, p=0.086), and fat mass (1.7kg vs. 3.5kg, p=0.249) over time in both sexes. Although changes in all parameters were higher in males than in females, these differences were not statistically significant overall. Regarding the percentage changes from baseline of all parameters, a significant difference in the change in BMI was only observed between females and males (1.2% vs. 5.5%, p=0.025).
On average, patients gained 1.3kg of body weight during the 12 months. While 12 patients (27.3%) lost or maintained their weight, 32 patients (72.7%) gained weight. However, there was no significant difference in age (p=0.527), sex (p=0.413), preoperative free T3 (p=0.257), free T4 (p=0.354), and TSH (p=0.453), preoperative BMI (p=0.084), postoperative thyroid status (p=0.475), and final pathology (p=0.214) between those who gained weight and those who did not. When patients were divided into two groups, based on postoperative thyroid status (suppressive vs. replacement), the findings revealed no significant differences in changes in body composition parameters between the groups.
Consequently, we performed a multivariable analysis to identify associations between patient characteristics and changes in body weight or fat mass (Table 2). While preoperative free T3 was found to be positively associated (β=0.47; 95% CI: 0.04–1.96, p=0.041), baseline fat mass percent was negatively associated with the change in fat mass (β=−0.36; 95% CI: −0.28 to −0.030, p=0.016). On the contrary, no association was revealed between the change in body weight and any variables in the multivariable analysis.
Multivariate linear regression analysis of factors associated with mean fat mass and weight change.
| Variables | Mean weight change (kg) | Mean fat mass change (kg) | ||||
|---|---|---|---|---|---|---|
| Standardised β-coefficient | 95% Confidence interval | p | Standardised β-coefficient | 95% Confidence interval | p | |
| Univariate analysis | ||||||
| Age (years) | −0.094 | −0.148; 0.079 | 0.545 | −0.097 | −0.130; 0.068 | 0.529 |
| Sex: female | 0.296 | −0.021; 6.532 | 0.051 | 0.177 | −1.239; 4.644 | 0.249 |
| Free T3 (pmol/L) | 0.137 | −0.649; 1.690 | 0.374 | 0.238 | −0.215; 1.784 | 0.121 |
| Free T4 (pmol/L) | −0.054 | −0.508; 0.357 | 0.727 | 0.187 | −0.144; 0.597 | 0.224 |
| TSH (μIU/mL) | −0.074 | −0.848; 0.521 | 0.633 | 0.054 | −0.494; 0.701 | 0.728 |
| Final pathology: Benign | −0.177 | −4.149; 1.108 | 0.250 | −0.148 | −3.412; 1.192 | 0.336 |
| Postop. RAI therapy: no | 0.067 | −2.265; 3.521 | 0.664 | 0.088 | −1.801; 3.233 | 0.569 |
| Postop. thyroid status: suppressive | 0.260 | −0.369; 5.116 | 0.088 | 0.210 | −0.755; 4.086 | 0.172 |
| Baseline weight (kg) | −0.077 | −0.120; 0.073 | 0.621 | −0.009 | −0.087; 0.082 | 0.951 |
| Baseline BMI (kg/m2) | −0.039 | −0.244; 0.189 | 0.800 | 0.023 | −0.175; 0.203 | 0.881 |
| Baseline fat mass (kg) | −0.159 | −0.185; 0.059 | 0.303 | −0.172 | −0.166; 0.047 | 0.264 |
| Baseline fat mass (%) | −0.255 | −0.260; 0.039 | 0.143 | −0.306 | −0.259; −0.004 | 0.044 |
| Multivariateanalysisa | ||||||
| Free T3 (pmol/L) | – | – | – | 0.474 | 0.043; 1.959 | 0.041 |
| Baseline fat mass (%) | – | – | – | −0.361 | −0.280; −0.030 | 0.016 |
BMI, body mass index; RAI, radioactive iodine; T3, tri-iodothyronine; T4, thyroxine; TSH, thyroid stimulating hormone.
Changes in thyroid function are believed to contribute to concomitant alterations in resting metabolic rate and body composition over time.2,7 However, studies addressing changes in body composition in patients undergoing thyroid surgery are limited and inconclusive.4,5,11 In this study, we found a statistically significant increase in mean body weight from 77.3 to 78.6kg, BMI from 30.6 to 31.2kg/m2, and fat mass from 28.8 to 30.9kg at the end of a one-year follow-up. Unlike these parameters, there were no statistically significant differences in FFM, muscle mass, total body water, and bone mass.
There have been many studies on the effects of total thyroidectomy on body weight, while only a limited number of studies assessed the body composition via BIA exist. In one study, Kormas et al.12 analysed the changes in body composition in eight postmenopausal women undergoing total thyroidectomy for a non-toxic goitre. Overall, BMI increased by 0.7%, lean mass increased by 1.6%, and fat mass decreased by 2.4% over 12 months; however, no significant changes in body weight or any parameters of body composition were revealed at four or 12 months postoperatively compared to baseline. In a recent study that evaluated the changes in body weight, body composition, calorimetric, and metabolic parameters of female patients with differentiated thyroid carcinoma at regular intervals up to 12 months, Izkhakov et al.13 found no significant change in body weight, BMI, fat mass, lean body mass, and abdominal fat distribution. However, mean systolic and diastolic blood pressures, heart rate, and resting energy expenditure were significantly higher, and the respiratory quotient was significantly lower in the subclinical hyperthyroidism phase than at baseline. Similar to these findings, a prospective study focusing on the changes in body composition after total thyroidectomy for benign multinodular goitre by Ozdemir et al.14 revealed no significant differences at six months of follow-up in changes in body weight, BMI, FFM, fat percentage, waist circumference, triceps skinfold, and basal metabolic rate in patients with euthyroid state or in patients with subclinical hypothyroid state.
In many studies and meta-analyses, a mild but not statistically significant increase in body weight was reported in patients with benign thyroid nodules or thyroid malignancies who underwent total thyroidectomy.3,5,12–16 On the contrary, some studies demonstrated a significant increase in body weight and BMI.4,17–19 In the present study, we found a statistically significant increase in mean body weight, BMI, and fat mass. However, when patients were stratified according to sex or postoperative thyroid status, there were no significant differences in changes in body composition measurements or body weight and BMI. Preoperative thyroid function status, pre-existing obesity, or postoperative thyroid status were previously shown to be the predictors of weight gain after treatment of hyperthyroidism.6,19 Our findings demonstrated that neither hyperthyroid patients nor euthyroid or hypothyroid patients experienced a significant change in body weight. In addition, obesity (a BMI ≥30kg/m2) and TSH suppressive levothyroxine therapy (subclinical hyperthyroid state) after thyroidectomy were not associated with weight change. Based on the multivariable analysis, no independent variables were predictive of change in weight. Similarly, in a study by Glick et al.5, univariate analysis did not identify any significant predictors of weight gain.
The main mechanism of weight gain in patients with hypothyroidism is believed to be caused by an increase in total body water and weight loss after therapy of hypothyroidism is primarily due to excretion of excess body water.1,20 However, it is unclear whether the change in body weight observed after total thyroidectomy is due to differences in total body water or changes in body fat.20 In this study, the most prominent change among body composition parameters over time was a significant increase in mean fat mass (from 28.8 to 30.9kg, 10.7% increase). Therefore, it can be concluded that significant weight gain was caused by increased fat mass. In contrast, there was a slight decrease in mean total body water (from 34.4 to 33.9kg, 1.4% decrease). However, this result was not confirmed by Kormas et al.12 suggesting that fat mass initially increased at six weeks postoperatively but decreased to baseline levels at 12 months with adequate thyroxine replacement. In another study, Wu et al.21 studied 28 patients with well-differentiated thyroid cancer. They found that body composition analysis using BIA revealed no significant changes in lean mass and fat mass from baseline to one month after withdrawal from thyroxine or two months after resumption of thyroxine administration. The median gain in fat mass observed in the present study was more pronounced in patients with hypothyroidism before thyroidectomy than in patients with euthyroid or hyperthyroid hormonal states. Furthermore, patients with levothyroxine replacement therapy in the postoperative period had a higher median fat mass than those with suppression therapy. However, these differences in fat mass were not statistically significant. Although multivariable regression analysis revealed a significant positive relationship between the change in fat mass and baseline free T3; interestingly, it was also shown that a lower percentage of body fat at baseline was a significant factor for the greater gain in fat mass. This may mean that those with a lower percentage of body fat tend to gain more fat mass after total thyroidectomy. A plausible explanation for the increase in fat mass after total thyroidectomy in patients with higher baseline free T3 levels may be that free T3 levels in the upper normal range or even higher, which increases the basal metabolic rate, could not be reached postoperatively in patients adequately treated with levothyroxine. Similarly, we speculate that the higher gain in fat mass after thyroidectomy in patients with lower preoperative body fat may be due to the loss of a higher basal metabolic rate postoperatively under levothyroxine replacement.
This study has several limitations. First, due to the cross-sectional design of the study, it is difficult to determine the potential direction of the association and causality. Thus, further longitudinal studies are needed to clarify the relationship between total thyroidectomy and the changes in body composition. Second, this study did not assess lifestyle-related factors or weight loss efforts of patients during the postoperative period, so it cannot be known whether any alterations in body composition were affected by changes in caloric intake or exercise status. Third, the number of patients and the number of male patients in this study were relatively small and the patients were heterogeneous with respect to the underlying thyroid disease. Therefore, future studies with a larger number of patients are needed to elucidate the effect of gender difference and diagnosis on body composition. Changes in body composition are likely to be observed for a longer period of time. However, confounding factors such as ageing could make it difficult to analyse the outcomes. Lastly, while BIA, which is a widely used and non-invasive technique, is not the gold standard for evaluating the body composition, the present study focused on change, rather than absolute values, of parameters.
ConclusionsAlthough the ageing process causes many changes in body composition, increases in body weight and fat mass after total thyroidectomy at the end of a one-year follow-up should be based on assumptions different from those of ageing. The importance of this study is that it shows that the effect of thyroidectomy on weight, which has been widely evaluated before, may be primarily due to the change in body fat, by evaluating body composition changes measured via BIA. Further studies that also take into account the metabolic parameters are necessary to investigate the potential mechanism of thyroid surgery on changes in body weight, fat mass, and other parameters of body composition.
AuthorshipAll named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Ethical statementAll procedures performed in the study involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration. The study was approved by the Ethics Committee of the Ankara University School of Medicine (I7-480-20). Informed consent for the study and surgical treatment was obtained from all patients before the procedure.
Data availabilityThe datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
FundingNo funding or sponsorship was received for this study or the publication of this article.
Conflict of interestSuleyman Utku Celik and Can Konca declare that they have no conflict of interest.