Thyroid hormones (THs) have important effects on cardiovascular (CV) physiology. Thyroid disorders are accompanied by serious effects on the CV system.
ObjectiveTo study the association between hyperthyroidism and the main CV risk factors (CVRFs), such as hypertension, dyslipidemia, diabetes and smoking in the Spanish population.
Material and methodsAn observational, retrospective, non-interventional study was performed using the statistical portal of the Spanish Ministry of Health associated with the Base de Datos Clínicos de Atención Primaria (BDCA) database.
ResultsIn 2019, 384,182 people [300,243 women (78.1%)] were diagnosed with hyperthyroidism, which represents 1.0% of the population with health problems registered in the BDCAP database (38,365,258 people). The prevalence of hyperthyroidism was more frequent in women (2.48 times) than in men and increased with age. When the whole population was considered, the prevalence of hypertension (34.90% vs. 19.90%; odds ratio, OR 2.16, 95% CI 2.14–2.17), dyslipidemia (34.47% vs. 21.57%; OR 1.90, 95% CI 1.88–1.91), diabetes (12.88% vs. 8.12%; OR 1.66, 95% CI 1.65–1.68) and smoking (10.89% vs. 7.61%; OR 1.48, 95% CI 1.46–1.49) was significantly (p<0.0001) higher in the population diagnosed with hyperthyroidism compared to those without this diagnosis. These significant differences were maintained in both women and men. A separate analysis of the age group 65 years or older showed statistically significant (p<0.0001) differences in the prevalence of hypertension (66.26% vs. 59.43%; OR 1.34, 95% CI 1.33–1.36), dyslipidemia (52.61% vs. 49.05%; OR 1.15, 95% CI 1.14–1.17) and smoking (6.29% vs. 5.93%; OR 1.06, 95% CI 1.04–1.09) between patients with and without a diagnosis of hyperthyroidism, but not in the prevalence of diabetes, which was similar (24.63% vs. 24.63%; OR 1.00, 95% CI 0.99–1.01; p=0.89).
ConclusionOur study shows that the diagnosis of hyperthyroidism is significantly associated with the main CVRFs in Spanish population attended by primary care regardless of the gender of the patients. This association disappears in those patients aged 65 years or older diagnosed with diabetes.
Las hormonas tiroideas tienen importantes efectos sobre la fisiología cardiovascular (CV). Los trastornos tiroideos se acompañan de graves efectos sobre el sistema CV.
ObjetivoEstudiar la asociación entre hipertiroidismo y los principales factores de riesgo CV (FRCV), como hipertensión, dislipemia, diabetes y tabaquismo, en la población española.
Material y métodosSe realizó un estudio observacional, retrospectivo y no intervencionista utilizando el portal estadístico del Ministerio de Sanidad español asociado a la Base de Datos Clínicos de Atención Primaria (BDCA).
ResultadosEn 2019, 384.182 personas (300.243 mujeres [78,1%]) fueron diagnosticadas de hipertiroidismo, lo que representa el 1,0% de la población con problemas de salud registrada en la base de datos BDCAP (38.365.258 personas). La prevalencia de hipertiroidismo fue más frecuente en mujeres (2,48 veces) que en hombres y aumentó con la edad. Cuando se consideró el conjunto de la población, la prevalencia de hipertensión (34,9% vs 19,9%; odds ratio [OR]:2,16; IC95%: 2,14-2,17), dislipemia (34,47% vs 21,57%; OR:1,90; IC95%: 1,88-1,91), diabetes (12,88% vs 8,12%; OR:1,66, IC95%: 1,65-1,68) y tabaquismo (10,89% vs 7,61%; OR:1,48, IC95%: 1,46-1,49) fue significativamente (p<0,0001) mayor en la población diagnosticada de hipertiroidismo en comparación con la población sin este diagnóstico. Estas diferencias significativas se mantuvieron tanto en mujeres como en hombres. Un análisis separado del grupo de edad de 65años o más mostró diferencias estadísticamente significativas (p<0,0001) en la prevalencia de hipertensión (66,26% vs 59,43%; OR:1,34, IC95%: 1,33-1,36), dislipemia (52,61% vs 49,05%; OR:1,15, IC95%: 1,14-1,17) y tabaquismo (6,29% vs 5,93%; OR:1,06, IC95%: 1,04-1,09) entre pacientes con y sin diagnóstico de hipertiroidismo, pero no en la prevalencia de diabetes, que fue similar (24,63% vs 24,63%; OR:1,00, IC95%: 0,99-1,01; p=0,89).
ConclusionesNuestro estudio muestra que el diagnóstico de hipertiroidismo se asocia significativamente con los principales FRCV en población española atendida en atención primaria, independientemente del sexo de los pacientes. Esta asociación desaparece en aquellos pacientes mayores de 65años diagnosticados de diabetes.
Thyroid hormones (THs) have important effects on cardiovascular (CV) physiology.1,2 Triiodothyronine (T3) increases heart rate, stroke volume, speed and force of cardiac contractions and shortens diastolic relaxation time.3 All of these effects are accompanied by an increase in cardiac output and blood pressure, mainly systolic blood pressure. In addition, it reduces systemic resistance by causing vasodilation of the peripheral arterioles. The fundamental role of THs in the maintenance of cardiac homeostasis has been observed in different clinical studies suggesting that the CV system is negatively affected by fluctuations in circulating TH levels.4 Moreover, not only the myocardial tissue, but also the vascular endothelium has receptors for THs and, therefore, are sensitive to changes in circulating HT concentrations.5
Hyperthyroidism is a clinical situation characterised by increased synthesis and secretion of THs by the thyroid gland. The most common cause is Graves’ disease, followed by toxic multinodular goitre. The prevalence of hyperthyroidism in the general population varies between 0.8 and 1.4%6,7 and is more common in women, increasing with advancing age.6
During the last two decades, accumulated evidence has revealed the contribution of THs to CV events, exerting its action through genomic and non-genomic pathways within cardiomyocytes. Thyroid dysfunction has direct effects on myocardial contractility, systolic and diastolic blood pressure, cardiac mass, heart rate, ejection fraction, and cardiac output, which can ultimately lead to heart failure.4 Some possible mechanisms linking thyroid dysfunction with CVD are dyslipidemia, endothelial dysfunction, changes in blood pressure, and the direct effects of THs on the myocardium.5
THs have a significant influence on carbohydrate metabolism. Thyroid dysfunction may affect carbohydrate metabolism in type 2 diabetic (T2DM) patients more than in non-diabetic patients.8–12 Furthermore, levels of both free thyroxine (FT4) and free T3 (FT3) could be additional risk factors associated with incident diabetes, especially in the presence of overweight or obesity.13 On the other hand, thyroid disorders are accompanied by serious effects on the CV system through numerous mechanisms, such as dyslipidemia, hypertension, systolic and diastolic myocardial dysfunction, and endothelial dysfunction.14
In this context, we consider it of interest to understand more deeply the association of hyperthyroidism with CV risk factors (CVRFs) in our population to be able to establish a better relationship between hyperthyroidism and CV morbidity and mortality. The objective of our study was to study the association between hyperthyroidism and these CVRFs in our population.
Material and methodsStudy designAn observational, retrospective, non-interventional study was performed using the statistical portal of the Ministry of Health associated with the Base de Datos Clínicos de Atención Primaria (BDCA) database.15 This database has been constructed for statistical and research purposes, with the consensus of all the autonomous communities of Spain. It collects standardised clinical information annually on the care provided by the Primary Care level, from a large random sample (around 10%) of the clinical records of the population assigned to this level of care and is representative of each autonomous community. This study was approved by the local ethics committee of the Hospital Universitario Puerta de Hierro Majadahonda (Madrid, Spain) (PI 125/22).
Study sampleThe data were collected throughout the first four months of 2022. At that time, the last update of this database in 2019 contained information on the people assigned to the primary care of the National Health System throughout the national territory. The data collected included, among others, health problems, and medications prescribed and that have been dispensed in pharmacies. The data source was the electronic medical record and the system allowed anonymous use of the data. The type of sampling used was a single-stage random sampling by clusters (basic health areas), stratified by autonomous community and size of the municipality in which the health centres were located, with a sample size of 4,864,058 people. The health problems were coded with ICD9, ICD10ES or ICPD2.
Information search and data collection methodologyBDCAP data are organized into separate information cubes, each containing a single analysis or study variable. There are currently seven available variables (health problems, comorbidity, consultations, medications, visits, procedures, and parameters). In our study, the “health problems” entry of the statistical portal associated with the BDCAP 2019 database was used. This entry included those health problems that had been “active” in the year of study and that were registered in the clinical record in coded form. All acute health problems recorded in the year of study were considered active, as well as chronic health problems that remained open in the year of study, because they were either permanent or long-term problems.
Study variablesWe performed a search for the health problem “hyperthyroidism/thyrotoxicosis”, coded as T85. To characterise the population studied, the following demographic and socioeconomic variables were described: gender (male, female) and age (age groups 0–14, 15–34, 35–64 and 65 and over years). Different subpopulation selection filters with health problems were used. The use of filters allowed the selection of a subpopulation of users based on the health problem or problems under study. In this way we were able to quantify the population with hyperthyroidism that also has another specific health problem. Using the appropriate filters, we were able to characterise the population with hyperthyroidism and the following specific CVRFs: arterial hypertension (HT) [uncomplicated HT (K86) and HT with target organ involvement (K87)], lipid metabolism disorders (T93), diabetes mellitus (DM) [insulin-dependent DM (T89) and non-insulin-dependent DM (T90)] and smoking (P17).
Statistical analysisQuantitative variables are expressed as absolute value (people with health problems) and percentage in relation to the total population or reference subpopulation. The calculation of the proportion of CVRFs in the population of patients with and without hyperthyroidism was used to calculate the relative risk using the odds ratio (OR) and its 95% confidence interval (CI). The same procedure was used to calculate the relative risk of each of the CVRFs studied in patients with a diagnosis of hyperthyroidism, as well as to analyse the possible differences in this relative risk based on age and gender of the studied subjects. The relationship between qualitative variables was studied using the chi-square test. Significant differences were considered when p<0.05.
ResultsPrevalence of hyperthyroidismIn 2019, 384,182 people [300,243 women (78.1%) and 83,939 men (21.8%)] were diagnosed with hyperthyroidism, which represented 0.82% of the total Spanish population (47,105,358), and 1.0% of the population with health problems registered in the BDCAP database (38,365,258 people) in that year. The prevalence of hyperthyroidism was higher in women (2.48 times) than in men and increased with increasing age (Table 1). Hyperthyroidism was more prevalent in women than in men in all age groups studied. This difference was more pronounced in the 15–34 age range (4.8 times more prevalent). The percentage distribution of patients with a diagnosis of hyperthyroidism in relation to age is shown in Table 1. The age group with the highest prevalence of hyperthyroidism was 35–64 years old [208,110 people (54.2%)].
Total population with health problems registered in the BDCAP database in 2019 and its distribution in patients with hyperthyroidism according to age, gender and cardiovascular risk factors.
| Total population in BDCAP | Patients with hyperthyroidism | ||
|---|---|---|---|
| Number | Percentage | ||
| All | 38,365,258 | 384,182 | 1.00 |
| Gender | |||
| Male | 18,230,737 | 83,939 | 0.46 |
| Female | 20,134,521 | 300,243 | 1.49 |
| Age (years) | |||
| 0–14 | 5,598,051 | 2,327 | 0.04 |
| 15–34 | 7,591,284 | 32,664 | 0.43 |
| 35–64 | 17,119,977 | 208,110 | 1.21 |
| 65 and over | 8,055,946 | 141,080 | 1.75 |
| Cardiovascular risk factors | |||
| Hypertension | 7,690,491 | 134,090 | 1.74 |
| Dyslipidemia | 8,326,527 | 132,420 | 1.59 |
| Diabetes | 3,133,467 | 49,486 | 1.57 |
| Smoking | 2,931,070 | 41,832 | 1.42 |
The prevalence of hyperthyroidism in patients with CVRFs (hypertension, dyslipidemia, diabetes, and smoking) is shown in Table 1.
When the whole population was considered, the prevalence of hypertension (34.90% vs. 19.90%; odds ratio 2.26, 95% CI 2.14–2.17), dyslipidemia (34.47% vs. 21.57%; odds ratio 1.90, 95% CI 1.88–1.91), diabetes (12.88% vs. 8.12%; odds ratio 1.66, 95% CI 1.65–1.68) and smoking (10.89% vs. 7.61%; odds ratio 1.48, 95% CI 1.46–1.49) was significantly (p<0.0001) higher in the population diagnosed with hyperthyroidism compared to those without this diagnosis (Table 2). These significant differences were maintained in both women and men (Table 2). The most prevalent CVRF in women was dyslipidemia regardless of the presence (33.24%) or absence (21.72%) of hyperthyroidism. However, in men with hyperthyroidism, hypertension (41.75%) was the most prevalent CVRF, whereas in men without this diagnosis it was dyslipidemia (21.41%) (Table 2).
Prevalence of cardiovascular risk factors in the entire cohort of studied patients and in patients with and without hyperthyroidism according to gender and age.
| All subjects | Patients with hyperthyroidism | Patients without hyperthyroidism | OR | 95% CI | p | ||||
|---|---|---|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | ||||
| Hypertension | |||||||||
| All | 7,690,491 | 20.05 | 134,090 | 34.90 | 7,556,401 | 19.90 | 2.16 | 2.14–2.17 | <0.00001 |
| Gender | |||||||||
| Female | 4,052,320 | 20.13 | 99,042 | 32.99 | 3,953,278 | 19.93 | 1.98 | 1.96–1.99 | <0.00001 |
| Male | 3,638,171 | 19.96 | 35,048 | 41.75 | 3,603,123 | 19.86 | 2.89 | 2.85–2.93 | <0.00001 |
| Age (years) | |||||||||
| 35–64 | 2,822,581 | 16.49 | 40,053 | 19.25 | 2,782,528 | 16.45 | 1.21 | 1.19–1.22 | <0.00001 |
| 65 and over | 4,796,913 | 59.54 | 93,482 | 66.26 | 4,703,431 | 59.43 | 1.34 | 1.33–1.36 | <0.00001 |
| Dyslipidemia | |||||||||
| All | 8,326,527 | 21.70 | 132,420 | 34.47 | 8,194,107 | 21.57 | 1.90 | 1.88–1.91 | <0.00001 |
| Gender | |||||||||
| Female | 4,408,286 | 21.89 | 99,815 | 33.24 | 4,308,471 | 21.72 | 1.79 | 1.78–1.81 | <0.00001 |
| Male | 3,918,241 | 21.49 | 32,605 | 38.84 | 3,885,636 | 21.41 | 2.33 | 2.30–2.36 | <0.00001 |
| Age (years) | |||||||||
| 35–64 | 4,053,320 | 23.68 | 56,452 | 27.13 | 3,996,868 | 23.63 | 1.20 | 1.19–1.21 | <0.00001 |
| 65 and over | 3,956,245 | 49.11 | 74,218 | 52.61 | 3,882,027 | 49.05 | 1.15 | 1.14–1.17 | <0.00001 |
| Diabetes | |||||||||
| All | 3,133,467 | 8.17 | 49,486 | 12.88 | 3,083,981 | 8.12 | 1.66 | 1.65–1.68 | <0.00001 |
| Gender | |||||||||
| Female | 1,439,118 | 7.15 | 33,348 | 11.11 | 1,405,770 | 7.09 | 1.64 | 1.62–1.66 | <0.00001 |
| Male | 1,694,349 | 9.29 | 16,138 | 19.23 | 1,678,211 | 9.25 | 2.34 | 2.30–2.38 | <0.00001 |
| Age (years) | |||||||||
| 35–64 | 1,079,844 | 6.31 | 14,281 | 6.86 | 1,065,563 | 6.30 | 1.09 | 1.07–1.11 | <0.00001 |
| 65 and over | 1,982,978 | 24.62 | 34,748 | 24.63 | 1,948,230 | 24.61 | 1.00 | 0.99–1.01 | 0.89 |
| Smoking | |||||||||
| All | 2,931,070 | 7.64 | 41,832 | 10.89 | 2,889,238 | 7.61 | 1.48 | 1.46–1.49 | <0.00001 |
| Gender | |||||||||
| Female | 1,302,763 | 6.47 | 30,428 | 10.13 | 1,272,335 | 6.41 | 1.64 | 1.62–1.66 | <0.00001 |
| Male | 1,628,307 | 8.93 | 11,404 | 13.59 | 1,616,903 | 8.91 | 1.61 | 1.58–1.64 | <0.00001 |
| Age (years) | |||||||||
| 35–64 | 2,097,583 | 12.25 | 30,696 | 14.75 | 2,066,887 | 12.22 | 1.24 | 1.23–1.26 | <0.00001 |
| 65 and over | 478,367 | 5.94 | 8,871 | 6.29 | 469,496 | 5.93 | 1.06 | 1.04–1.09 | <0.00001 |
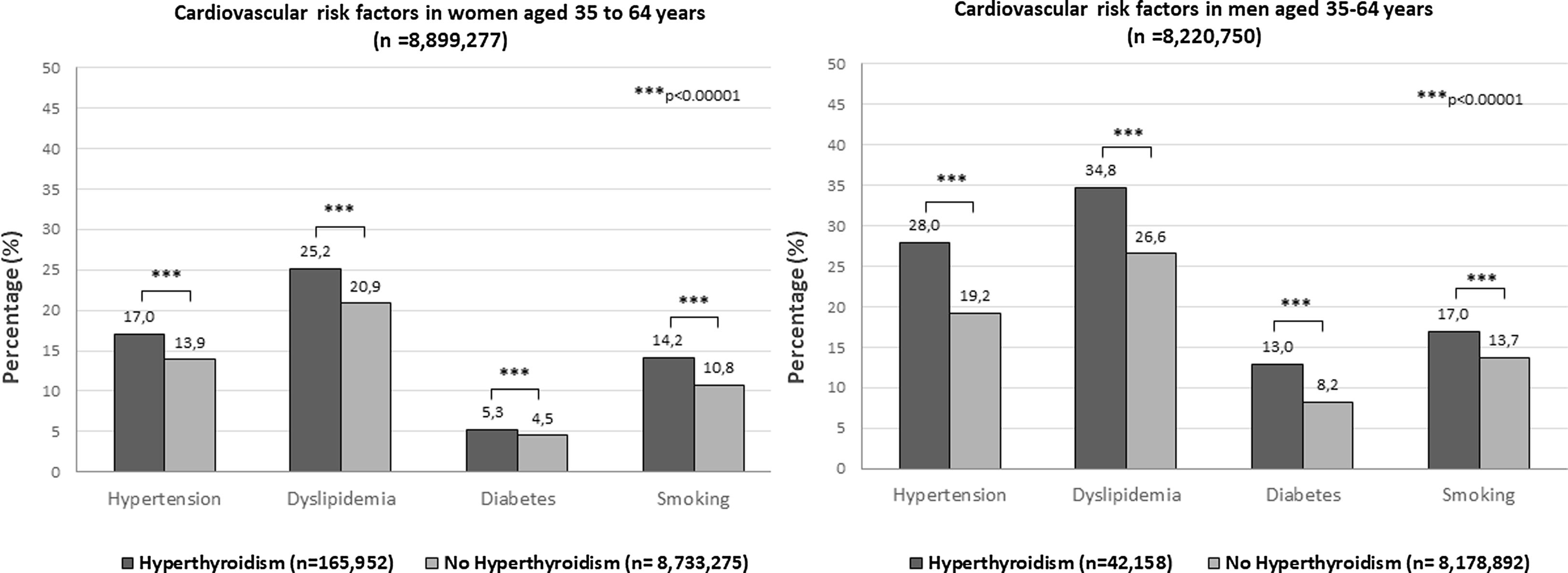
Since the highest prevalence of CVRFs was observed in the 35–64yr and 65yr and older age groups, a separate analysis was performed for these groups (Table 2, Figs. 1 and 2). When we considered the age group 35–64yr, we also observed a significantly (p<0.0001) higher prevalence of hypertension (19.25% vs. 16.45%; odds ratio 1.21, 95% CI 1.19–1.22), dyslipidemia (27.13% vs. 23.63%; odds ratio 1.20, 95% CI 1.19–1.21), diabetes (6.86% vs. 6.30%; odds ratio 1.09, 95% CI 1.07–1.11), and smoking (14.75% vs. 12.22%; odds ratio 1.24, 95% CI 1.23–1.26), in the group of patients with hyperthyroidism compared to those without this diagnosis (Table 2). These same significant differences were observed when women and men were considered separately (Fig. 1). In this age group, the most prevalent CVRF in both women and men was dyslipidemia in both the group with (27.13%) and without (23.63%) a diagnosis of hyperthyroidism (Table 2, Fig. 1).
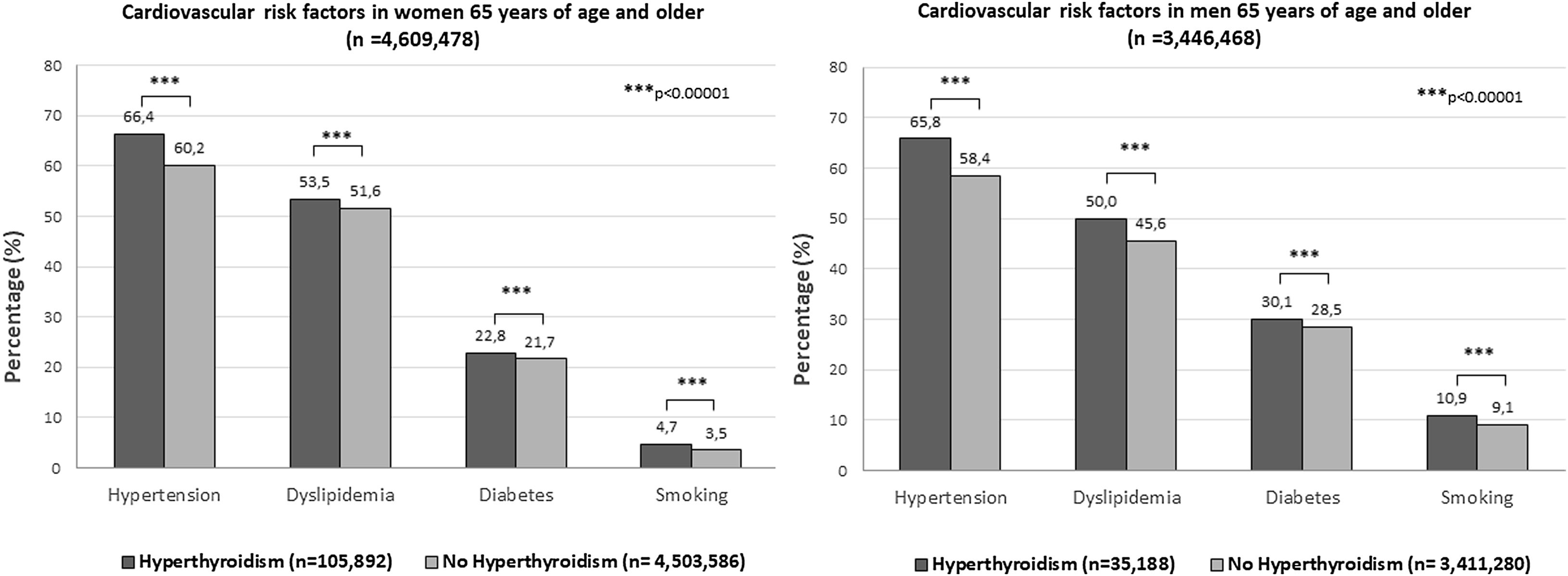
A separate analysis of the age group 65 years or older showed statistically significant (p<0.0001) differences in the prevalence of hypertension (66.26% vs. 59.43%; odds ratio 1.34, 95% CI 1.33–1.36), dyslipidemia (52.61% vs. 49.05%; odds ratio 1.15, 95% CI 1.14–1.17) and smoking (6.29% vs. 5.93%; odds ratio 1.06, 95% CI 1.04–1.09) between patients with and without a diagnosis of hyperthyroidism, but not in the prevalence of diabetes, which was similar (24.63% vs. 24.63%; odds ratio 1.00, 95% CI 0.99–1.01; p=0.89) (Table 2). When the groups were analyzed according to gender significant differences (p<0.0001) were maintained for all CVRFs between the groups with and without the diagnosis of hyperthyroidism (Fig. 2). Lastly, in this age group, the most prevalent CVRF in patients with (66.4% vs. 65.8% women vs. men) and without (60.2% vs. 58.4% women vs. men) hyperthyroidism was hypertension (Fig. 2).
DiscussionThe present study shows that the diagnosis of hyperthyroidism is significantly associated with the main CVRFs, such as hypertension, dyslipidemia, diabetes, and smoking in Spanish population attended by primary care. This association is maintained regardless of the gender of the patients. Regarding age, this association is present in patients older than 35 years and only disappears in those patients aged 65 years or older diagnosed with diabetes.
Hyperthyroidism is a well-known secondary cause of isolated systolic hypertension.16 It is due to elevated THs, increasing systolic blood pressure by decreasing systemic vascular resistance, increasing heart rate, and raising cardiac output. These pathological effects can potentially lead to CV consequences, such as atrial arrhythmias (especially atrial fibrillation), pulmonary hypertension, left ventricular hypertrophy, and heart failure.17
Some studies suggest that hyperthyroidism may predispose to a permanent increase in blood pressure, with associated CV morbidity not only during the acute episode of hyperthyroidism, but also long after hyperthyroidism has been well controlled.18–20 Increased long-term CV morbidity has been reported in hyperthyroid patients treated with antithyroid drugs despite normalization of thyroid hormone levels.18 The risk of hypertension has been found to be elevated for decades (up to 35 years) after treatment of hyperthyroidism with radioiodine (RAI) compared to the general population.19 In 2014, Ryödi et al.20 reported a population-based cohort study conducted in 4,334 hyperthyroid patients (median age 46 years) treated with thyroidectomy showing that hyperthyroidism increased the risk of hospitalization due to hypertension and the risk was sustained up to two decades after effective surgical treatment. Our findings confirm the association between hyperthyroidism and hypertension, although our study does not allow us to establish a causal effect between the two entities.
TH excess is associated with a decrease in serum total cholesterol, LDL-cholesterol, ApoB, and lipoprotein (a) levels, a decrease in HDL-C without changes in triglyceride levels.21 In our study, we found a higher prevalence of dyslipidemia in the group of patients diagnosed with hyperthyroidism compared to those without this diagnosis. The explanation for this finding is not clear, since, as previously commented, hyperthyroidism is generally associated with a more favourable lipid profile. We cannot rule out the fact that this significantly higher prevalence of hyperlipidemia found in patients with a diagnosis of hyperthyroidism could be due to the association of other risk factors for developing hyperlipidemia, also associated with the diagnosis of hyperthyroidism, such as diabetes and smoking, as we have found in the present study. However, although in our study the association between hyperthyroidism and hyperlipidemia was significant, this finding does not necessarily imply a causal relationship between the two clinical entities.
Excess circulating TH is associated with insulin resistance, increased intestinal glucose absorption, elevated hepatic glucose output and glucose turnover, hyperglycaemia, and increased free fatty acid concentrations.22 Different studies have established an association between thyroid dysfunction and diabetes mellitus.9–12 Hyperthyroidism has also been related to diabetes mellitus.9,10,23 More recently, an analysis of prospective studies addressing the association between thyroid function and T2DM incidence, showed an association of hyperthyroidism with the risk of T2DM, although not statistically significant 1.16 (95% CI, 0.90–1.49).24 Our study showed a significant association between hyperthyroidism and diabetes, regardless of the gender of the patients. This positive association was observed in the whole population and in subjects aged 35–64 years. However, it disappeared when the population over 65 years of age was considered. The explanation for this finding is unclear and warrants further studies to confirm this association and to establish or rule out a causal relationship between hyperthyroidism and diabetes.
Several studies have shown that cigarette smoking is related to different changes in thyroid function.25 In this setting, smoking has been associated with a reduction in TSH and an increase in TH, probably through an activation of the sympathetic nervous system. In addition, smoking can activate thyroid autoimmunity, positively influencing the development of Graves’ disease, even reducing the effectiveness of treatment and promoting relapses. Lastly, smokers have a higher prevalence of thyroid multinodularity and toxic nodular goitre.25 These data seem to be in agreement with the findings obtained in our study that show a higher prevalence of smoking in the group of patients diagnosed with hyperthyroidism, mainly in the younger population, although the causal relationship cannot be demonstrated with our study.
The main strength of our study is the large sample size and an adequate distribution of the population studied, since the majority of the Spanish population receives health care through the general practitioners of the public health system. The BDCAP database is a nationwide database that includes data from most of the Spanish population and contains all active health problems, thus allowing an accurate assessment of disease prevalences without data selection bias. Limitations include the absence of information in the BDCAP on the time of diagnosis of the hyperthyroidism and the duration of the disease, as well as the degree of control of thyroid hyperfunction. Our study was also unable to provide data on thyroid autoimmunity, iodine intake, duration of antithyroid treatment or type of non-pharmacological treatment (radioiodine or surgery). Neither did we know the etiology, duration or degree of thyroid hyperfunction in our patients. Another important limitation was the impossibility of ensuring a causal effect between hyperthyroidism and the different CVRFs evaluated. In addition, it is necessary to consider the possibility of information bias in those patients with an active disease, in this case hyperthyroidism, who could have been more likely to have been screened for the CVRFs analyzed.
We consider our results to be relevant for health planning due to the demonstration of an increased risk of the main CVRFs (hypertension, dyslipidemia, diabetes, and smoking) in people diagnosed with hyperthyroidism, with the associated clinical implications in terms of increased CV morbidity and mortality. Our findings allow us to suggest that the CV risk screening programmes currently in force in the general population should be carried out with greater insistence in subjects diagnosed with hyperthyroidism.
In conclusion, the present study based on clinical information obtained from the care provided at the primary care level in our country shows that hyperthyroidism is associated with the main CVRFs (hypertension, dyslipidemia, diabetes and smoking). These findings should lead us to consider hyperthyroidism as an independent CVRF.
Conflict of interestsThe authors declare they have no conflict of interest.