Malnutrition in elderly patients with hip fracture has been described as a factor associated with poor outcomes. This evidence for elderly patients undergoing elective total hip arthroplasty (THA) for osteoarthritis is not well-established.
MethodsWe retrospectively studied a cohort of patients with an age ≥65 years admitted to the hospital for THA between January 2018 and December 2020. Demographic characteristics were collected. Albumin and total lymphocyte count were included in the pre-operative analysis and 24h postoperatively. Nutritional screening was carried out 24h postoperatively. GLIM criteria were applied for the diagnosis of malnutrition.
Results25 patients out of the total cohort of 65 (38.4%) were malnourished. Five out of six patients (83.3%) with postoperative complications presented malnutrition compared with 20 of 59 patients (33.8%) without postoperative complications (P=0.028). Mean length of stay (LOS) was 3.49±0.88 days. Five out of six (83.3%) patients with postoperative complications presented LOS >3 days compared with one out of six patients (16.6%) with LOS ≤3 days (P=0.009).
26 patients (40%) were referred to a community health centre, no differences in diagnosis of malnutrition were detected compared with patients who were discharged home.
Patients with a diagnosis of malnutrition were significantly older, had a lower body mass index (BMI), a lower preoperative and postoperative albumin and worse anthropometric parameters.
ConclusionsMalnutrition is associated with postoperative complications and longer LOS in elderly patients with elective THA. Risk factors for malnutrition are older age and low BMI.
La desnutrición en el paciente geriátrico con fractura de cadera es un factor asociado a un peor pronóstico. La evidencia en pacientes con cirugía electiva de prótesis de cadera por artrosis es escasa.
MétodosEstudio retrospectivo de una cohorte de pacientes con edad ≥65 años ingresados para cirugía electiva de prótesis de cadera entre enero del 2018 y diciembre del 2020. Se recogieron características demográficas, albúmina y el recuento total de linfocitos en el preoperatorio y postoperatorio. Se aplicaron los criterios GLIM para el diagnóstico de desnutrición a las 24 h postoperatorias.
ResultadosDe la cohorte total de 65 pacientes, 25 (38,4%) presentaron desnutrición; 5 de un total de 6 pacientes (83,3%) con complicaciones postoperatorias presentaban desnutrición en comparación con 20 de 59 pacientes (33,8%) sin complicaciones postoperatorias (p=0,028). La estancia media fue de 3,49±0,88 días; 5 de 6 pacientes (83,3%) con complicaciones postoperatorias presentaron una estancia media >3 días en comparación con 1 de 6 pacientes (16,6%) con una estancia media ≤3 días (p=0,009).
Un total de 26 pacientes (40%) fueron derivados a un centro sociosanitario al alta, sin diferencias en el estado nutricional en comparación con los pacientes que fueron dados de alta a domicilio.
Los pacientes con desnutrición tenían una edad significativamente más avanzada, un menor índice de masa corporal (IMC), una albúmina preoperatoria y postoperatoria significativamente más baja y una peor antropometría.
ConclusionesLa desnutrición se asocia a complicaciones postoperatorias y a una mayor estancia media hospitalaria en pacientes con edad ≥65 años ingresados para cirugía electiva de prótesis de cadera. Los factores de riesgo son la edad avanzada y el IMC bajo.
Orthopaedic hip surgery for osteoarthritis and fractures has increased over the last decades in a population that is living longer. Complications such as infections have an important economic burden on health and quality of life, age and associated comorbidities being the main prognostic factors. A high percentage of geriatric patients are malnourished upon hospital admission. Malnutrition is associated with muscle weakness, decreased strength, immunodepression, apathy, and poor cardiac function.1 These conditions increase the likelihood of postoperative complications, prolonged recovery and increased mortality. Furthermore, observational studies have shown that malnutrition and advanced age in patients undergoing THA are early predictors of mortality.2,3 Moreover, 37% of patients with hip fractures have sarcopenia, which also makes rehabilitation more difficult.4 Retrospective studies have reported malnutrition in 30% of geriatric patients undergoing elective THA. In addition, it has been observed that male sex and older age are risk factors for suboptimal nutritional parameters such as hypoalbuminaemia and lower total lymphocyte count, both related to a longer hospital stay.5 Hypoalbuminaemia before total joint arthroplasty is predictive of surgical wound infection,6 and also complications and reintervention in the postoperative period of hip fracture.7–9
Clinical practice guidelines recommend nutritional assessment and intervention in elderly patients undergoing orthopaedic hip surgery.10–12 Implementation of nutritional screening in this population group allows for the identification of individuals with malnutrition and therefore early nutritional intervention. This intervention may have a positive effect on postoperative complications, length of hospital stay and costs. These evidence-based recommendations are supported mostly by studies including elderly patients with hip fracture. The evidence reported in the literature on the benefits of nutritional intervention in elderly patients undergoing elective THA for osteoarthritis is scarce.
The aim of this study was to describe the nutritional status of a cohort of elderly patients undergoing THA for osteoarthritis and to determine the associations between malnutrition and postoperative complications, LOS and discharge to a care centre. Additionally, we evaluated factors (especially pre-surgical) related to a higher risk of malnutrition in this cohort.
This study was approved by the hospital's Ethical Committee. Ref. PR118/21 (CSI 21/22).
Patients and methodsThis is a retrospective observational study. Following the evidence-based recommendations, a clinic protocol focused on the screening of nutritional status in elderly patients undergoing orthopaedic hip surgery was approved and implemented by the Endocrinology and Nutrition and Orthopaedic Surgery Services of Centre d’Atenció Integral Dos de Maig, Barcelona. The inclusion criteria were individuals over 65 years of age who underwent elective THA for osteoarthritis from January 2018 until December 2020. Exclusion criteria were patients with hip fractures, since most of them were referred to a tertiary hospital, and the lack of availability in the clinical records of the variables necessary to carry out the specific analysis of the study.
The baseline information collected was: age, sex, the date of surgery, comorbidities assessed with the Charlson index (which includes a number of chronic diseases that predict mortality). The Charlson index was classified into two groups: patients with an index <1%, and patients with an index ≥1% in order to differentiate patients with no comorbidities from patients with one or more comorbidities.
Albumin and total lymphocyte count were included in the pre-operative analysis and 24h postoperatively by the orthopaedic surgeon. Height, weight and body mass index (BMI) were obtained from the records of the anaesthesia visit and at time of admission. Nutritional screening was carried out by a dietitian at 24h postoperatively. Nutritional evaluation included the registration of food intake for the last 24h, the percentage of weight loss, mid-arm circumference measured on the non-dominant arm, triceps skin fold thickness using skin fold calliper, calf circumference, and grip strength, which was measured using a dynamometer on the non-dominant hand.
GLIM criteria were applied for the diagnosis of malnutrition. The diagnosis of malnutrition was established when at least one phenotypic criterion (non-voluntary weight loss, BMI<20kg/m2 for individuals aged <70 years or <22kg/m2 for individuals aged ≥70 years, reduced muscle mass: mid-arm circumference below the 50th percentile, calf circumference <31cm, altered grip strength) and one aetiological criteria (reduced oral intake, acute or chronic illness) was found. Once the diagnosis of malnutrition was made, the severity was defined as moderate malnutrition identified by: loss of 5–10% of body weight, BMI<20kg/m2 in individuals aged <70 years or <22kg/m2 in individuals aged ≥70 years, reduced muscle mass: mid-arm circumference or triceps skin fold thickness between the 50th and 25th percentiles. Severe malnutrition was defined by: loss of more than 10% of the body weight, BMI<18.5kg/m2 in individuals aged <70 years or <20kg/m2 in individuals aged ≥70 years, reduced muscle mass: mid-arm circumference or triceps skin fold thickness below 25th percentile, calf circumference <31cm or altered grip strength.
Once the nutritional assessment was carried out, we prescribed oral supplements in the following cases: Patients were diagnosed with malnutrition defined by GLIM criteria, or when we predicted that oral intake could not be maintained above 50% of the necessary nutritional requirements for at least seven days. The type of oral supplement was chosen on the basis of anthropometry, biochemical parameters, registration of food intake for the last 24h and the presence of altered grip strength. Data on prescription of oral nutritional supplements at discharge was collected.
Information about postoperative complications, hospital length and discharge to a care centre was collected from medical notes during admission and post-discharge with a follow up of 6 months. Complications included: superficial and deep wound infection, surgical wound dehiscence, pneumonia, respiratory failure that required endotracheal intubation, pulmonary thromboembolism, deep vein thrombosis, acute kidney failure, urinary tract infection, stroke, acute coronary syndrome, significant anaemia requiring transfusion, septicaemia, coxofemoral luxation, and death.
Statistical analysisThe data were analysed using the IBM Statistical Package for Social Sciences (SPSS) version 22. Continuous variables were presented as mean and standard deviation (SD) and categorical variables as frequencies. Either chi-squared or Fisher's exact test were used to test associations of categorical variables and Student's t-test for continuous variables. A P value ≤0.05 was considered statistically significant. The factors associated with the presence of malnutrition were analysed with a logistic regression model that included as independent variables age, sex and other variables with significant associations in the univariate analysis. Results were presented as odds ratios and 95% confidence intervals.
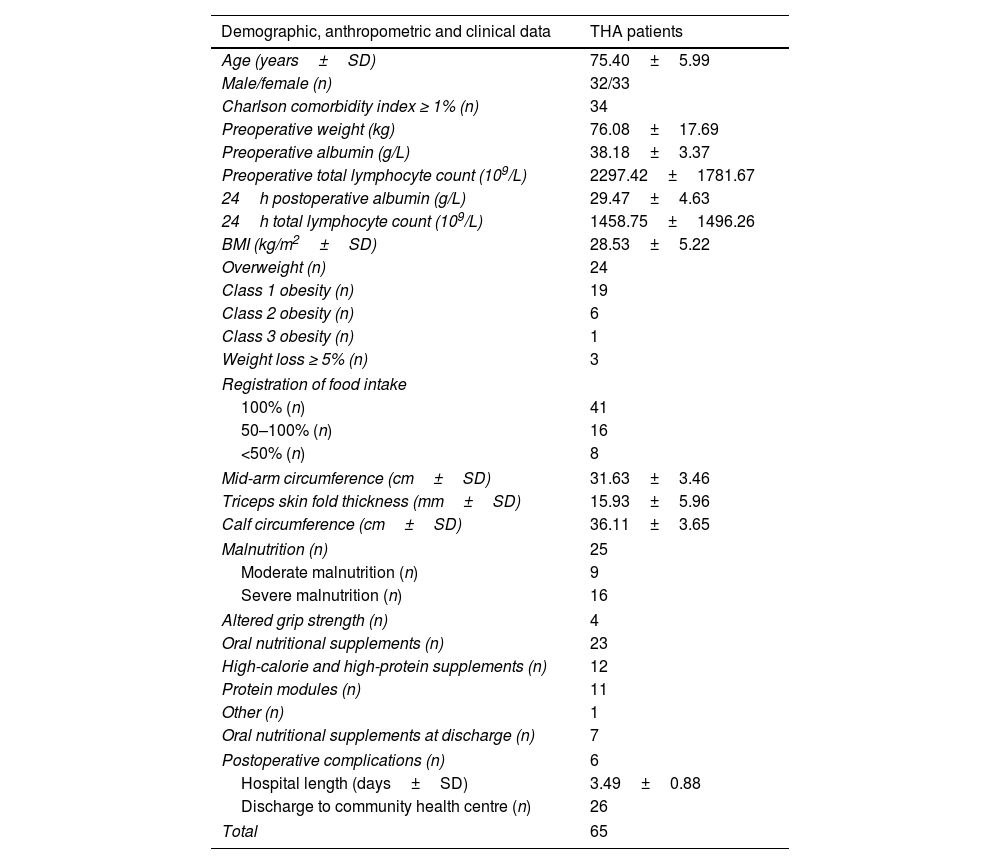
ResultsA total of 65 patients undergoing THA for osteoarthritis met our inclusion criteria between January 2018 until December 2020. The overall mean age was 75.40±5.99. The sex distribution were 32 men and 33 women. We classified 31 individuals into Charlson Comorbidity Index <1% and 34 individuals into Charlson Comorbidity Index ≥1% The mean BMI was 28.53±5.22kg/m2, and specifically, 15 patients had a BMI <25kg/m2, 24 were overweight, 19 had class 1 obesity, 6 had class 2 obesity and there was one patient with class 3 obesity. The mean preoperative albumin value was 38.18±3.37g/L, and 24h postoperatively it was 29.47±4.63g/L. The preoperative median total lymphocyte count was 2297.42±1781.67×109/L and 24h postoperatively it was 1458.75±1496.26×109/L. Registration of food intake for the last 24h showed eight patients with an oral intake <50% of the calculated requirements, and 16 patients with an oral intake between 50 and 100% of the calculated requirements. Weight loss from the anaesthesia visit until admission for surgery was observed in six patients, three of them showing a percentage of weight loss ≥5%. Anthropometric measurement demonstrated only one patient with a mid-arm circumference below the 50th percentile and 32 patients with a triceps skin fold thickness below the 50th percentile; only two patients showed a calf circumference below 31cm. 42 patients with triceps skin fold thickness below the 50th percentile presented malnutrition compared with seven patients with triceps skin fold thickness above the 50th percentile (P=0.001). Four patients had an altered grip strength and all of them met diagnostic criteria for malnutrition. According to GLIM criteria, nine patients showed moderate and 16 severe malnutrition; therefore 25 patients (38.4%) from the whole cohort presented malnutrition.
We prescribed oral nutritional supplements in 23 patients during admission and in seven patients at discharge. The most common types of supplements given were high-calorie and high-protein supplements and protein modules.
Descriptive statistics of the study population are summarised in Table 1.
Baseline characteristics.
| Demographic, anthropometric and clinical data | THA patients |
|---|---|
| Age (years±SD) | 75.40±5.99 |
| Male/female (n) | 32/33 |
| Charlson comorbidity index ≥ 1% (n) | 34 |
| Preoperative weight (kg) | 76.08±17.69 |
| Preoperative albumin (g/L) | 38.18±3.37 |
| Preoperative total lymphocyte count (109/L) | 2297.42±1781.67 |
| 24h postoperative albumin (g/L) | 29.47±4.63 |
| 24h total lymphocyte count (109/L) | 1458.75±1496.26 |
| BMI (kg/m2±SD) | 28.53±5.22 |
| Overweight (n) | 24 |
| Class 1 obesity (n) | 19 |
| Class 2 obesity (n) | 6 |
| Class 3 obesity (n) | 1 |
| Weight loss ≥ 5% (n) | 3 |
| Registration of food intake | |
| 100% (n) | 41 |
| 50–100% (n) | 16 |
| <50% (n) | 8 |
| Mid-arm circumference (cm±SD) | 31.63±3.46 |
| Triceps skin fold thickness (mm±SD) | 15.93±5.96 |
| Calf circumference (cm±SD) | 36.11±3.65 |
| Malnutrition (n) | 25 |
| Moderate malnutrition (n) | 9 |
| Severe malnutrition (n) | 16 |
| Altered grip strength (n) | 4 |
| Oral nutritional supplements (n) | 23 |
| High-calorie and high-protein supplements (n) | 12 |
| Protein modules (n) | 11 |
| Other (n) | 1 |
| Oral nutritional supplements at discharge (n) | 7 |
| Postoperative complications (n) | 6 |
| Hospital length (days±SD) | 3.49±0.88 |
| Discharge to community health centre (n) | 26 |
| Total | 65 |
Regarding postoperative complications, these were reported in six patients, four patients with anaemia requiring transfusion, one patient with acute renal failure, anaemia requiring transfusion, coxofemoral luxation and wound infection, and one patient with septicaemia and death. Five out of six patients (83.3%) with postoperative complications presented malnutrition compared with 20 out of 59 patients (33.8%) without postoperative complications (P=0.028). No differences were observed in patients who received oral nutritional supplements compared with patients who did not receive them.
The mean LOS was 3.49±0.88 days. 11 out of 20 patients (55%) with LOS >3 days presented malnutrition compared with 14 of 45 patients (31%) with LOS ≤3 days (P=0.068). Five out of six patients (83.3%) with postoperative complications presented LOS >3 days compared with one out of six patients (16.6%) with LOS <3 days (P=0.009).
Regarding discharge to a care centre, 26 patients were referred to a community health centre. Nine out of 26 patients (34.6%) referred to community health centre presented malnutrition compared with 16 out of 39 (41%) discharged home (P=0.603). The percentage of malnutrition did not differ significantly between patients discharged to a care centre or discharged home.
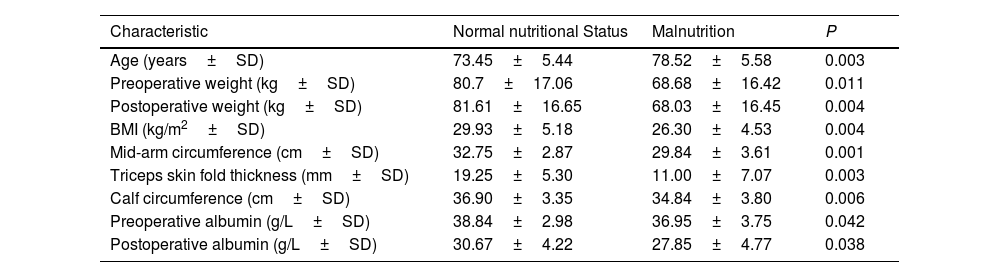
The characteristics of patients that were significantly associated with malnutrition were older age, lower BMI, preoperative and postoperative low levels of albumin and worse anthropometric parameters such as mid-arm circumference, triceps skin fold thickness and calf circumference. We did not observe differences in gender and Charlson Comorbidity Index (Table 2).
Factors related to malnutrition.
| Characteristic | Normal nutritional Status | Malnutrition | P |
|---|---|---|---|
| Age (years±SD) | 73.45±5.44 | 78.52±5.58 | 0.003 |
| Preoperative weight (kg±SD) | 80.7±17.06 | 68.68±16.42 | 0.011 |
| Postoperative weight (kg±SD) | 81.61±16.65 | 68.03±16.45 | 0.004 |
| BMI (kg/m2±SD) | 29.93±5.18 | 26.30±4.53 | 0.004 |
| Mid-arm circumference (cm±SD) | 32.75±2.87 | 29.84±3.61 | 0.001 |
| Triceps skin fold thickness (mm±SD) | 19.25±5.30 | 11.00±7.07 | 0.003 |
| Calf circumference (cm±SD) | 36.90±3.35 | 34.84±3.80 | 0.006 |
| Preoperative albumin (g/L±SD) | 38.84±2.98 | 36.95±3.75 | 0.042 |
| Postoperative albumin (g/L±SD) | 30.67±4.22 | 27.85±4.77 | 0.038 |
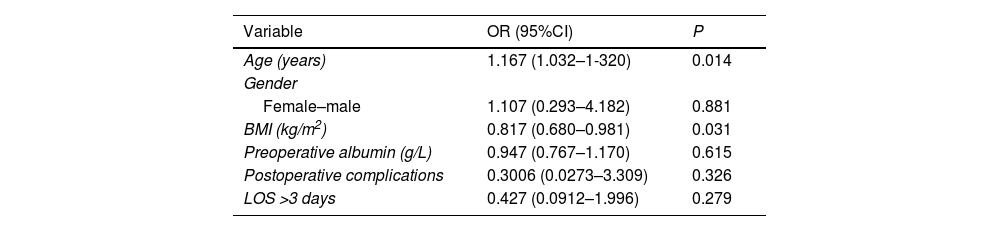
On multivariate analysis, variables that remained independently associated with the presence of malnutrition were age (OR 1.167 [95% CI: 1.032–1.320]), and BMI (OR 0.817 [95% CI: 0.680–0.981]) (Table 3). Anthropometric measurements with collinearity with BMI were excluded from the logistic regression model. The variables of postoperative complications and LOS >3 days did not remain independently associated with presence of malnutrition on the multivariate analysis.
Logistic regression model to analyse factors associated with malnutrition.
| Variable | OR (95%CI) | P |
|---|---|---|
| Age (years) | 1.167 (1.032–1-320) | 0.014 |
| Gender | ||
| Female–male | 1.107 (0.293–4.182) | 0.881 |
| BMI (kg/m2) | 0.817 (0.680–0.981) | 0.031 |
| Preoperative albumin (g/L) | 0.947 (0.767–1.170) | 0.615 |
| Postoperative complications | 0.3006 (0.0273–3.309) | 0.326 |
| LOS >3 days | 0.427 (0.0912–1.996) | 0.279 |
The main finding of our study is that malnutrition is associated with postoperative complications in patients undergoing elective THA. In addition, the percentage of malnutrition is also higher (although statistically non-significant) in patients with a longer LOS (>3 days), while a longer LOS is related to a greater number of complications.
Our data are consistent with previous reported studies. Thus, several systematic reviews and meta-analyses observed an association between malnutrition and an increased risk of postoperative complications in patients undergoing elective THA.13
Biochemical markers of malnutrition like total lymphocyte count and albumin have been related as well, in these group of patients, to a longer LOS.5,14 These findings have also been confirmed in patients undergoing revision of THA in which hypoalbuminaemia was associated with a 50% increased risk of reoperation, bleeding, surgical site infections, and unplanned reoperation.15
In our cohort, risk factors associated with malnutrition were older age and lower BMI, similar to previously reported studies. In addition, some studies have identified other risk factors like sex (although with heterogeneous results)5 and previous comorbidities.14 We used the Charlson index to assess comorbidities, finding one or more of them in about half of the patients; however, we have not observed an association with malnutrition, probably due to a small sample size.
Obesity has been identified classically as an important risk factor for the development of lower extremity osteoarthritis. Although some studies have reported more postoperative complications in patients with class II and III obesity, when adjusted for albumin levels this association is attenuated.16 With the ageing of the population and the increasing prevalence of obesity in the last decades, sarcopenic obesity is becoming increasingly important. Previous studies in patients undergoing elective hip surgery reported a prevalence of 30% of sarcopenic obesity which, in turn, makes rehabilitation more difficult,17 and also an association between pinch grip <6.3kg with a higher LOS.18 In another previous study focused on patients undergoing elective hip surgery, a higher operative time, longer average LOS and 30-day readmissions have been found, especially in patients with BMI >50kg/m2.19 In our cohort, 26 patients have obesity and the group of patients with BMI below 25kg/m2 presented a significantly higher percentage of malnutrition compared to the group of patients with obesity. It should be noted that we do not have any patients with BMI >50kg/m2. This is consistent with other studies in which BMI <15kg/m2 is associated with increasing postoperative complications and a mean LOS more than twice as long19 and a BMI <20kg/m2 was associated with an eight-fold increased risk of two-year mortality and an increased LOS.20 Therefore, existing previous supporting data that nutritional intervention would be useful in patients with extreme BMI to improve postoperative outcomes.
We observed a prevalence of 38% of malnutrition in our cohort. Previously published data reported a variable prevalence (from 4 to 30%)5,14 probably concerning the different criteria used for the diagnosis of malnutrition, as most studies used only biochemical markers (classically albumin <35g/L and/or total lymphocyte count <1500×109/L). On the other hand, it is well known that albumin levels can be influenced by the stress of acute illness, inflammation and severity. In fact, it has been described that patients with lower albumin levels have a higher Charlson index, so albumin could be also a marker of comorbidity and not only a biochemical marker of malnutrition.21 There are limited references in the literature evaluating malnutrition with parameters other than albumin and total lymphocyte count. One of them identified a higher Nutritional Risk Screening 2002 score among patients with periprosthetic infections,22 and a meta-analysis described three of the studies significantly associated the Mini Nutritional Assessment questionnaire with increased hip fracture mortality.23
We applied GLIM criteria for the diagnosis of malnutrition. The first meeting of the GLIM working group was held at the ESPEN Congress in 2016. They recommended the implementation of the nutrition community use GLIM Criteria in prospective and retrospective cohort studies as well as in clinical trials to validate its relevance for clinical practice and reached a global consensus for the diagnosis of malnutrition in the clinical setting.24
Our study protocol included GLIM criteria for the diagnosis of malnutrition, and it was a useful tool to identify those patients who needed nutritional intervention. To our knowledge there is only one previous study prospectively evaluating the effects of a nutritional intervention in malnourished patients with elective joint arthroplasty, but again, the diagnosis of malnutrition was made using only albumin <3.4g/L. In this referenced study, LOS, re-admission rate, and 90-day charges were compared for differential change between patients in study and control hospitals for all elective hip and knee arthroplasty patients, and for malnourished patients over time as the nutrition intervention was implemented. Charges associated with initial hospitalisation, individual re-admissions, and total 90 days of care decreased significantly for the malnourished cohort at the study hospital who received nutritional assessment. However, they observed a significant increase in all charges that occurred for the malnourished cohort over the time at the control hospitals.25 The results of this study suggested that nutritional intervention in this group of patients would be beneficial in terms of cost-effectiveness.
Regarding the type of supplementation used, the most prescribed supplements were hypercaloric hyperproteic following the latest recommendations for geriatric patients and on the basis of anthropometric and biochemical parameters.
Few studies have previously evaluated the type of supplementation in this group of patients. A systematic review identified that carbohydrate-containing fluid improved insulin-like growth factor levels, reduced hunger, nausea, and LOS, and attenuated the decrease in the whole-body insulin sensitivity and the endogenous glucose release. Amino acid supplementation reduced muscle atrophy and accelerated the return to functional mobility.26 Another previous study evidenced that perioperative immunonutrition in elderly patients undergoing total hip and knee arthroplasty reduced infectious complications by 55% and reduced LOS compared with a control group.27 Protein supplementation plus exercise training improved muscle mass, muscle strength and functional outcomes, and reduced pain in older adults with lower-limb osteoarthritis, particularly in those who had undergone total joint replacement.28
In the last decades, some clinical guidelines recommended nutritional intervention in patients with hip fracture based on meta-analyses demonstrating reduction of postoperative complications.10,29 However, New Cochrane review points stated that trials should be large and adequately powered to detect differences in mortality and morbidity and be sufficiently blinded to protect against performance and measurement biases.30
Based on these recommendations, we implemented a new clinical protocol for the screening of nutritional status in elderly patients undergoing orthopaedic hip surgery. Obviously, the results of our study should be validated by prospective studies with a larger number of patients. If benefits are confirmed in the future, we should consider a nutritional intervention ideally, prior to surgery.
The limitations of our study are the retrospective analysis, although this may have been mitigated by following the protocol in clinical practice, which has allowed us to have few “missing” variables since the nutritional evaluation and intervention were well standardised in all patients. Note that dynamometry was only evaluated in 36 patients, and this may have affected one of the GLIM criteria (reduced muscle mass) although anthropometry was evaluated in all patients. Another limitation is a reduced sample size, which could explain the fact that we did not find a relationship between comorbidities and malnutrition described in other studies.
The strengths of our study are that a complete nutritional evaluation was made including registration of food intake, weight loss percentage, anthropometry and biochemical evaluation applying recommended criteria for the diagnosis of malnutrition which conducted a nutritional intervention. Complications were follow-up for the first six months after surgery.
ConclusionMalnutrition in elderly patients undergoing total hip arthroplasty is related to postoperative complications and longer LOS. In addition, postoperative complications are associated with a longer LOS. Risk factors for malnutrition are older age and low BMI. Therefore, these two factors should alert clinicians to better assess the risk of malnutrition in elderly patients with elective total hip arthroplasty.
Conflicts of interestNone.
FundingThis research has not received specific support from public sector agencies, commercial sector or non-profit entities.
We wish to thank all the individuals enrolled in the study.