Collision tumors represent two morphologically different tumors attached to one another at a single anatomical site. While collision tumors have been reported in various organs, the concomitant presence of a pituitary adenoma with a second sellar lesion is an uncommon occurrence. When this does occur, radiation-induced sarcomas may coexist with a pituitary adenoma as result of previous radiation therapy aimed at treating the pituitary adenoma. Of these, fibrosarcomas are the most common, but rhabdomyosarcomas and chondrosarcomas have also been reported. If patients who have undergone previous radiation therapy are excluded from scrutiny, the presence of these two types of tumor in the same patient becomes even rarer.1
This report describes the case of a 41-year-old male, without personal or hereditary antecedents of relevance, who was referred to our Neuroendocrinology Unit presenting insidious discomfort and paresthesia in both hands that had developed over the previous 6 months. The patient also reported reduced visual acuity and partial loss of lateral vision over the previous year, accompanied by recurring headaches, which were relieved by analgesic administration.
Confrontation visual field tests found bitemporal hemianopsia. Magnetic resonance imaging (MRI) of the sellar region detected a pituitary mass of heterogeneous signal intensity but with well-defined borders, measuring 28mm×39mm×22mm, pressing on the optic chiasm. Hormonal study found slight secondary panhypopituitarism due to tumoral compression (FT4: 0.79ng/dl [0.90–1.70ng/dl]; TSH: 2.09μIU/ml [0.4–4μIU/ml]; testosterone total 3.1nmol/L [10–28nmol/L]; FSH 5.2mIU/ml [2–8mIU/ml]; LH 3.2mUI/ml [2–12mIU/ml]; cortisol 49.8ng/ml [50–250ng/ml]; ACTH 12.8pg/ml [8.0–66.0pg/ml]; IGF-1 89.5ng/ml, with adequate suppression of GH levels after an oral glucose tolerance test). Diagnosis established a suspected pituitary macroadenoma.
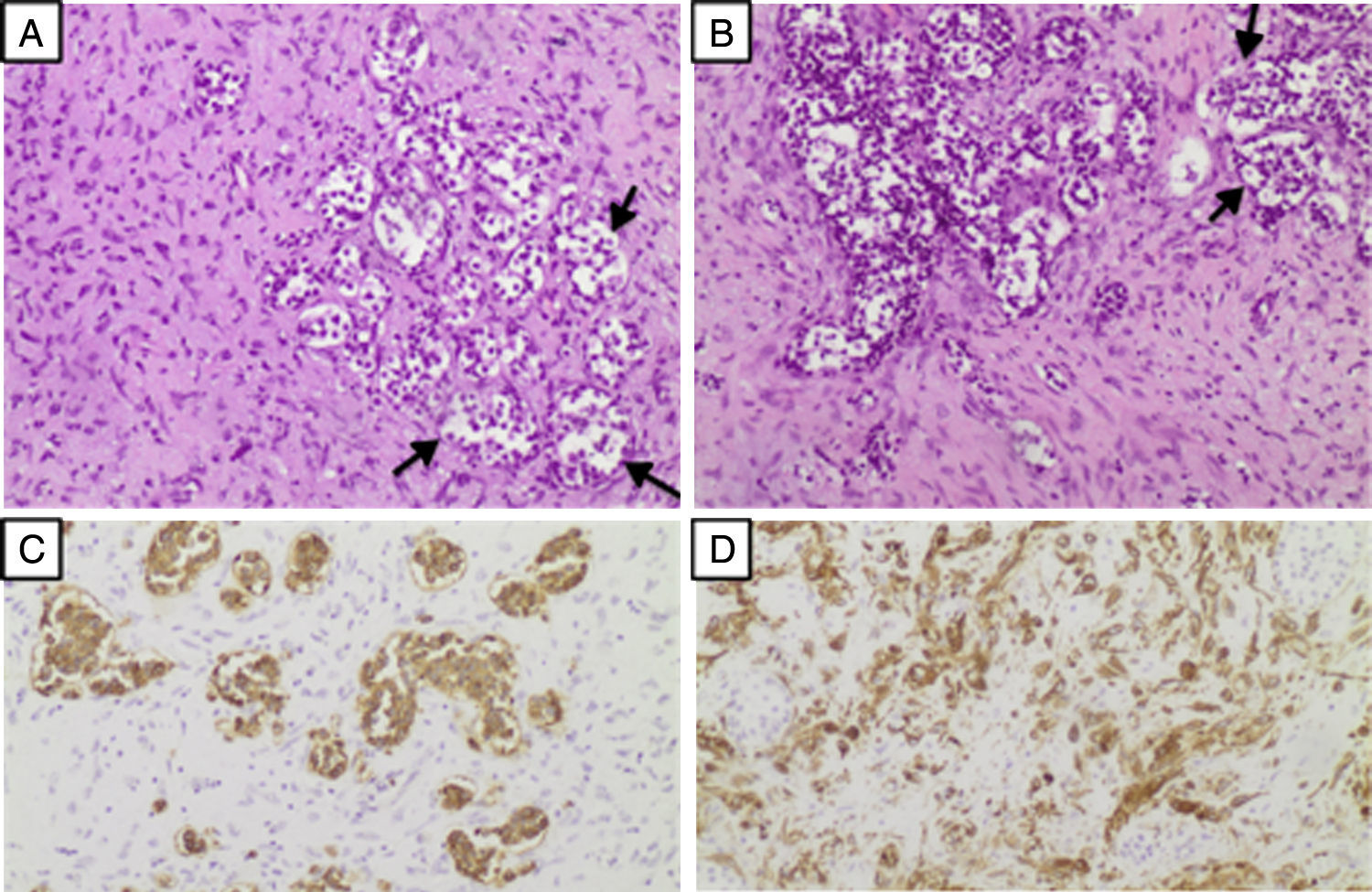
Endoscopic endonasal transsphenoidal resection of the pituitary tumor was performed. Post-operative histopathologic analysis revealed a proliferation of fusiform cells in a lax stroma, with moderate atypia and a proliferation index (Ki-67) of around 10%; vimentin and SMA (smooth muscle actin) were immunophenotype-positive, while other markers showed negative (CD31, CD34, EMA, S100, PGFA, CKAE1/AE3). Islands with an epithelial aspect of pituitary origin were mixed in with the neoplasia, which expressed chromogranin and showed negative for all pituitary hormones (ACTH, GH, PRL, TSH, FSH and LH) (Fig. 1). Histopathological diagnosis identified a collision tumor composed of low-grade mesenchymal spindle cell neoplasm and a non-secreting pituitary adenoma. Histopathologic features and the presence of a small residual tumor observed in post-operative MRI justified fractionated stereotactic radiotherapy, which was clinically well tolerated by the patient. After surgery and radiotherapy, the patient showed a notable clinical improvement, particularly in visual acuity and remained neurologically asymptomatic. In subsequent follow-up examinations, images showed no sign of remains or recurrence of the pituitary tumor. The patient continues to attend the clinic for regular check-ups.
Histopathology of collision sellar tumor. Hematoxylin-eosin stained sections (10×) show a proliferation of fusiform cells in a lax stroma, intermixed with islands of epithelial appearance (arrows) (A, B). Chromogranin expression by epithelial cells (C). Mesenchymal cells present vimentin immunophenotype and positive smooth muscle actin (SMA) (D).
This case presents several notable characteristics. Firstly, the coexistence of two pituitary tumors of different histogenesis. The presence of a collision sellar lesion is a very uncommon event. To date, the concomitance of two different pathologies within the sella have mainly been described in individual case reports; very few surgical series have been published that describe specific combinations of sellar lesions such as a double pituitary adenoma,2,3 a combination of an adenoma and Rathke's cleft cyst,4 or a gangliocytoma associated with a pituitary adenoma.5 In one of the very few case series published, Koutourousiou et al. reported an incidence of 1.46% of collision lesions among a group of 548 patients who underwent transsphenoidal surgery for pituitary adenoma resection. Among these pituitary adenomas with different features, the authors found one case of sarcoidosis, three cases of gangliocytoma, one schwannoma, one case of double pituitary adenoma, and two Rathke's cleft cysts.6
Secondly, the present case of a sellar collision tumor is of particular interest due to the discovery of a primary fibrosarcoma in a patient with no history of radiation exposure. This is an extremely rare event. To date, only 18 cases of primary sarcomas of the sellar region have been reported; of these, six were fibrosarcomas, with only one case of neoplasm with biphasic or collision pattern.7 To our knowledge, this case is only the second ever report of a collision pituitary tumor involving a primary fibrosarcoma. Moro et al. reported the first case, which consisted of combined sellar fibrosarcoma and prolactinoma in a patient who had not undergone previous radiotherapy. The patient presented a thymic carcinoma with metastatic disease, which was treated by administering etoposide, and a subsequent prolactinoma treated with bromocriptine without radiotherapy. Eight years later, radiological examination revealed a large pituitary mass, which on histological examination was compatible with fibrosarcoma in close association with a pituitary adenoma.8 Moro argues that etoposide tends to cause fibrosis in the pituitary stroma. In contrast to Moro's report, no adjuvant treatment was administered in the present case.
The low incidence of these tumors is largely conditioned by the difficulty of pre-operative diagnosis since most cases present clinically and radiologically as pituitary adenomas.6 This was true of the present case, in which clinical examination accompanied by a suggestive radiographic image led to an initial diagnosis of pituitary macroadenoma. The definitive diagnosis of a collision sellar lesion can only be determined by histological study because of the difficulty of distinguishing between these entities in clinical or radiological examination.
To date, no proven pathogenetic mechanism has been identified that might explain the relationship between a pituitary adenoma and a second sellar lesion. Regarding the etiology of the present case's fibrosarcomatous component, the literature hypothesizes two possibilities: metaplastic transformation from pituitary adenoma, or independent collision tumors.6,7 Unfortunately, distinguishing between these two possibilities on the basis of morphology alone is not possible.
Conflict of interestThe authors have no conflicts of interest to disclose.