A 51-year-old woman was admitted to the emergency room for headache, paresis of the left upper limb and binocular diplopia. She had grade 1 obesity (body mass index [BMI], 32kg/m2) and high blood pressure, for which she was taking irbesartan at 150mg/day. Two months before to admission she had undergone multiple dental treatments for periodontitis.
Clinical examination revealed a Glasgow Coma Score of 15. There were no signs of meningeal syndrome, but a proprioceptive deficit was found in the left lower limb. The patients had no fever.
Laboratory tests revealed hyperleukocytosis at 10G/L with neutrophil polynuclear cells, but a normal C-reactive protein level (<5mg/L).
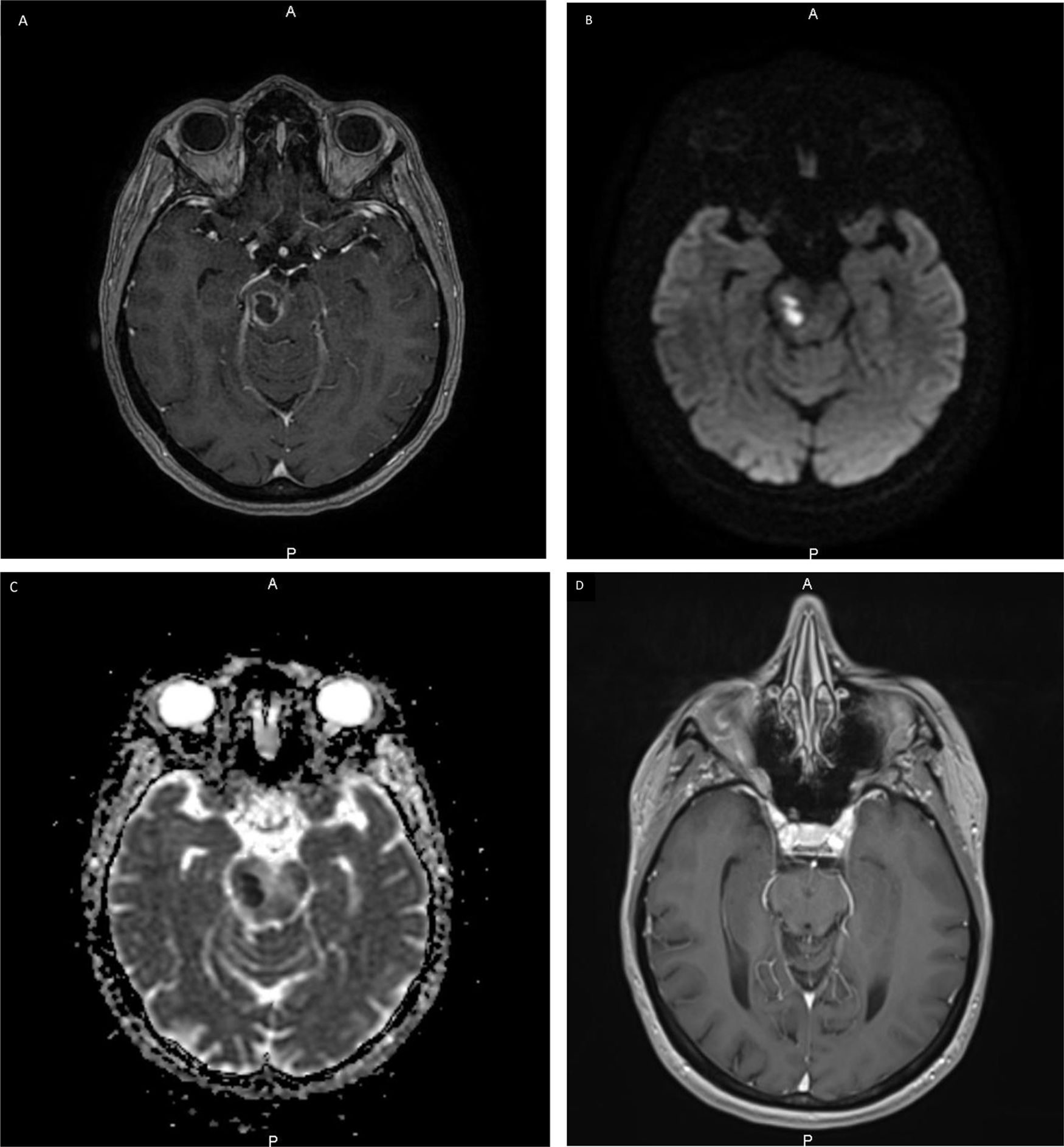
The results of lumbar puncture were inconsistent with meningitis. There was no evidence of endocarditis on transesophageal cardiac ultrasound. Cerebral magnetic resonance imaging (MRI) revealed a hypointense lesion with circumferential enhancement located in the right lateral midbrain. Similarly, the diffusion sequence disclosed a signal restriction in the central part of the lesion strongly suggesting a brainstem abscess (Fig. 1). Biopsy was performed for further work-up. Microbiological analysis revealed the presence of an oral bacterium, Aggregatibacter aphrophilus. The patient rapidly improved after treatment with amoxicillin 12g/day was started.
MRI shows a brainstem lesion. (A) Axial post-contrast T1-weighted MR image shows a right midbrain lesion with circumferential enhancement. (B) Axial diffusion MR image shows a high-signal-intensity area. (C) Axial diffusion with apparent diffusion coefficient (ADC) MR image shows a low-signal-intensity area. (D) Axial post-contrast T1-weighted MR image after 6 months showing a small residual hypointense sequela of the midbrain without contrast enhancement that correlated with the effectiveness of the antibiotic treatment.
A. aphrophilus is an obligate oral Gram-negative organism, a normal component of the commensal oral microbiota belonging to the HACEK group of bacteria. Bacteria may reach the brain by different routes, i.e. systemic hematogenous bacteremia, direct venous drainage, the lymphatic route or directly through the fascial spaces.1 Our patient had severe periodontitis and poor dental hygiene. The recent dental procedures were probably responsible for migration of the bacteria to the brain. Diabetes is a major risk factor for periodontitis, and the risk of periodontitis increases threefold in diabetic versus non-diabetic individuals. Our patient had no impaired blood glucose levels. However, obesity itself has been reported to be associated with periodontitis.2 Although the mechanisms underlying this association remain unclear, insulin resistance developing as a consequence of a chronic inflammatory state and oxidative stress may modulate the association between obesity and periodontitis.3 A Korean study reported a significant association between periodontal disease and waist circumference, but there was no correlation with BMI.4 Visceral adipose tissue is prone to secretion of proinflammatory adipokines, which induce low-grade inflammation and may lead to the development of insulin resistance. The roles of leptin, adiponectin and resistin, which are dysregulated in both periodontitis and obesity, must also be clarified. Although cerebral abscesses resulting from odontogenic foci remain relatively rare, especially at the brainstem area, the functional consequences may be serious, and the mortality rate may reach 30% in some series.5 The need for good dental hygiene and regular dental check-ups in obese subjects should be strongly emphasized.
Ethics approvalAll procedures performed in studies involving human participants were in accordance with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consentWritten informed consent for the study was obtained from the patient.
Availability of data and materialsNot applicable.
Code availabilityNot applicable.
FundingNone to declare.
Conflicts of interestThe authors declare no conflict of interest.