Roux-en-Y gastric bypass (RYGB) is an effective treatment for weight loss in patients with morbid obesity. However, few studies have assessed its long-term efficacy in super-obese patients. The study objective was to analyse the long-term effectiveness of RYGB and its effect on improvement of comorbidities after 10 years of follow-up, and to compare the results depending on baseline BMI (<50kg/m2 vs ≥50kg/m2).
Patients and methodsA retrospective study was conducted in 63 patients referred for RYGB with a 10-year or longer follow-up period. Mean BMI before surgery was 55kg/m2.
ResultsMean BMI decreased to 38.1kg/m2 at 10 years of follow-up. The success rates according to Reinhold criteria modified by Christou and to Biron's criteria were 30.2% and 54% respectively. The corresponding rates in super-obese patients were 21.4% and 57.1%. Significant, stable improvement was seen in diabetes, dyslipidemia, hypertension, and sleep apnea.
ConclusionsSustained weight loss was achieved after gastric bypass, with a mean excess weight loss of 50.6% after 10 years despite the high prevalence of super-obesity. Comorbidity improvement was maintained.
El baipás gástrico en Y de Roux (RYGB) es un tratamiento efectivo para la pérdida de peso en pacientes con obesidad mórbida. Sin embargo, en pocos estudios se ha evaluado su eficacia a largo plazo en pacientes con superobesidad (IMC ≥ 50kg/m2). El objetivo es analizar la efectividad del RYGB, su efecto sobre la mejoría de las comorbilidades tras 10 años de seguimiento y comparar los resultados en función del IMC inicial (<50kg/m2 vs ≥ 50kg/m2).
Pacientes y métodosSe realizó un estudio retrospectivo sobre 63 pacientes remitidos a RYGB con periodo de seguimiento igual o superior a 10 años. El IMC medio precirugía fue 55kg/m2.
ResultadosEl IMC medio descendió a 38,1kg/m2 a los 10 años de seguimiento. Las tasas de éxito según los criterios de Reinhold modificados por Christou y según los criterios de Biron fueron 30,2 y 54%. En pacientes con superobesidad estas tasas fueron 21,4 y 57,1%. Se observó remisión estable y significativa de la diabetes, hipertensión y apnea del sueño.
ConclusionesTras la cirugía bariátrica se consiguió pérdida de peso sostenida, con un porcentaje de exceso de peso perdido de 50,6% a los 10 años a pesar de la alta prevalencia de superobesidad. La mejoría de las comorbilidades permaneció estable.
Obesity is associated with comorbidities such as type 2 diabetes mellitus (T2DM), hypertension, dyslipidemia, sleep apnoea, some types of cancer and osteoarthritis.1 Its treatment is based on intensive lifestyle intervention (including modifying eating habits and regular physical activity) and pharmacologic therapy. In morbid obesity (Body mass index (BMI)>40kg/m2) and patients with BMI>35kg/m2 with presence of major comorbidities bariatric surgery is the preferred treatment.2
Evidence suggests that bariatric surgery (Roux-en-Y gastric bypass – RYGB – foremost) is an effective long-term treatment compared to conventional treatment, with significant weight reduction and decreased mortality.3,4 Less evidence compared to morbidly obese patients is available regarding its effect on super-obese patients (SOb), defined as those with BMI≥50kg/m2.5
In this study, we analyse long-term outcomes after RYGB with respect to weight loss and its effect on metabolic comorbidities by examining our experience in a cohort with a high prevalence of super-obese subjects (66.7%). The aims of our study were to compare the effectiveness of RYGB between super-obese and morbidly obese patients after 5 and 10 year follow-up in the maintenance of percentage excess weight loss (%EWL) and the percentage excess BMI lost (%EBL) and to analyse the impact of RYGB on diabetes, dyslipidemia, hypertension and obstructive sleep apnoea (OSA) 10 years after the procedure in super-obese and morbidly obese patients.
Subjects and methodsA retrospective study of all the patients undergoing a RYGB at our institution was performed. Although over 750 bariatric surgeries had been performed at our centre, only those with a 10-year or longer follow-up period were included in this study. 79 patients underwent open RYGB (laparoscopic technique was unavailable at the time the interventions were performed) by the same surgical team and 63 patients completed a 10-year follow-up at our Obesity Clinic: 21 morbidly obese and 42 super-obese subjects. The study was reviewed and approved by the Ethical Committee of our Institution. All patients signed an informed consent.
Patient selection was based on the recommendations from the National Institute of Health (NIH): BMI>40kg/m2 or above 35kg/m2 if significant comorbidities were associated, who had tried for over 5 years to control their obesity by lifestyle changes and who understood the risks and benefits of the procedure.
Preoperative (1 month prior to surgery) and every follow up visit (6 months, 1, 5 and 10 years after bariatric surgery) data acquisition was based on a research protocol at our Obesity Clinic. The protocol included a complete medical history (demographic, diet habits, complete dietetic history, physical activity, smoking habits, vascular risk factors, personal or family history of diseases), physical examination with anthropometry and blood pressure measurement (see below), biochemical (glucose, HbA1C, lipid profile, standard hepatic and renal function variables, nutritional biochemical parameters) and hormonal determinations. An oral glucose tolerance test was performed in all patients with no previous diagnosis of diabetes. In addition, a pulmonary function test and psychiatric evaluation was performed in all subjects prior to the surgery. The presence of fatty liver was defined by ultrasound criteria. OSA was defined by a pathological polysomnography.
After written informed consent, all patients underwent open-RYGB, with a gastric pouch of 20–30mL, an alimentary loop of 200cm and a biliopancreatic loop of 80cm.
Data sourceWe successfully acquired long-term data of at least 5 years’ time after RYGB for 69 patients (87.34%) and at 10 years’ time for 63 patients (79.75%), and these were included in the statistical analysis. Follow-up data for the first 5 years was accepted for patients who had the follow-up visit at exactly or plus/minus 2 months of the specific visit. After the fifth year a 6-month variability period was accepted. We defined loss to follow-up as absence for over 24 months from our clinic.
Outcome measuresThe main end point was weight loss referred to as the mean percentage of excess weight loss (%EWL).6 Changes in absolute weight (in kilograms), BMI, percentage total weight loss (%WL), and percentage excess BMI lost were also calculated when appropriate. %EWL was calculated as: %EWL=[preoperative weight–follow-up weight/preoperative weight–ideal weight]×100. The ideal body weight was calculated using a BMI of 25kg/m2. %EBMIL was calculated using the formula: [%EBMIL=(initial BMI–follow-up BMI/initial BMI–25)×100]. Regain of weight was calculated as follows: [Weight at 10 years after surgery–nadir weight].
We used three different weight criteria to evaluate follow up. The frequently cited 50% or above EWL was calculated to describe an effective result.7 The Reinhold classification modified by Christou was estimated to document results based on BMI, considering success of surgery when an excellent or good result was achieved (BMI≤35kg/m2).8 Biron et al.’s criteria was also applied, defining success as a final BMI<35kg/m2 when preoperative BMI<50kg/m2 or final BMI<40kg/m2 when preoperative BMI≥50kg/m2.9
Biochemical variables were measured with standard procedures at the matching examinations (1 month before RYGB, 6 months, 1, 5 and 10 years after). Criteria for health and disease were based on cut-off values or the use of medication for the condition considered. The criteria for diagnosing diabetes considered fasting plasma glucose level ≥126mg/dL, glucose level after glucose tolerance test >200mg/dL, HBA1C≥6.5%10 and/or personal history of diabetes or taking hypoglycemic drugs. Other criteria included: hypertension (personal history of hypertension11 and/or taking antihypertensive drugs), hypercholesterolemia or hypertriglyceridemia (total cholesterol above 200mg/dL and/or triglycerides above 150mg/dL or personal history of dyslipemia or taking hypolipidemic drugs).12 Blood pressure was measured using standard criteria (AHA recommendation)13 in every visit. The mean of three determinations was recorded. OSA was considered when documented sleep apnoea by polysomnography was observed at baseline.
Outcomes of the main comorbidities after 10-year follow-up were grouped into the categories of resolved (when the comorbid condition disappeared or no longer required treatment), improved or not modified; except for diabetes for which ADA remission criteria was used (remission [HbA1C<6%], partial remission [HA1C<6.5%] in both cases in the absence of hypoglycemic treatment or ongoing procedures, for at least one year; or no remission [previous criteria not met]).14
For OSA, improvement was considered after suppression of non-invasive assist respiratory devices.
Statistical analysesAll data and statistical analyses were processed using SPSS version 22 (SPSS, Inc., Chicago, IL). Mean values and standard deviations or 95% confidence intervals were used to define the baseline characteristics and changes over time. A result of p<0.05 was considered as significant. Quantitative variables were analysed using t-Student test. Qualitative variables were analysed by Chi square test. Simple correlation analysis was used for the association of comorbidities and baseline and 10 years BMI, age and gender. Multiple regression analysis was used to study predictors of BMI success after 10 years follow up.
For primary continuous outcome: Expected improvement of %EBL by intervention with RYGB>50%. We planned a study of a continuous response variable for the same individual pre-surgery and after 10 years follow up period. We need a minimum of 60 individual in the treatment arm to detect a 40% decrease in the geometric means of %EBL.
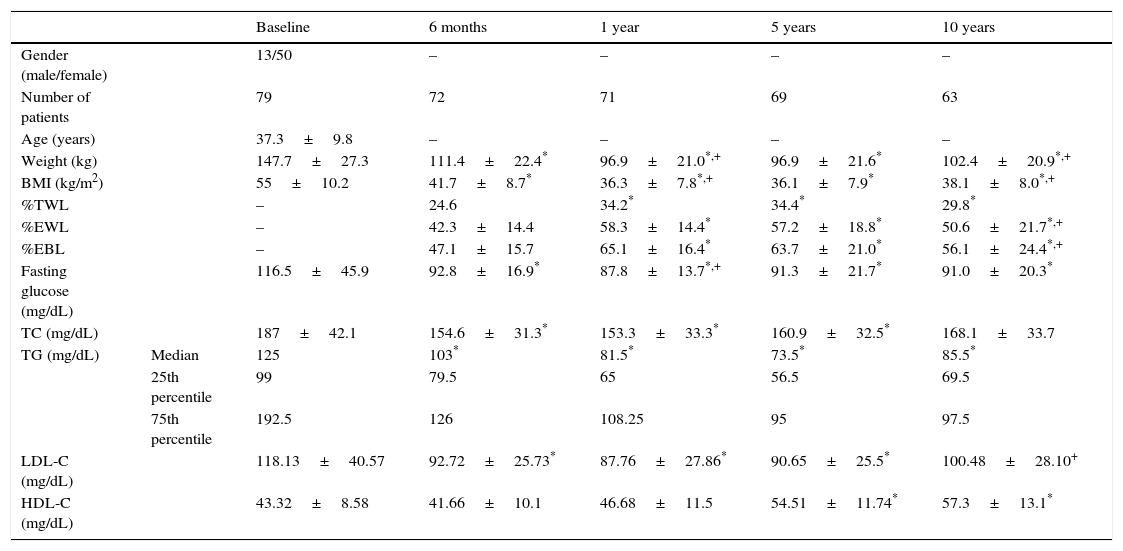
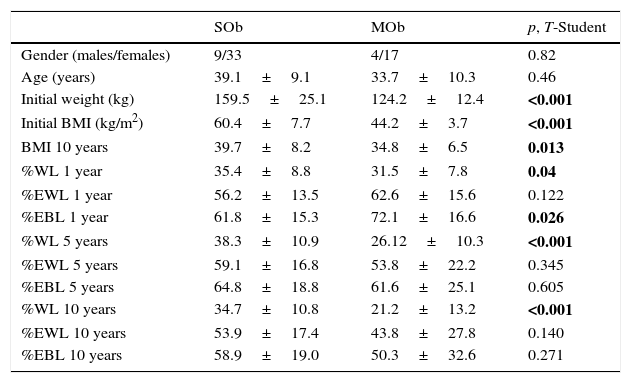
ResultsClinical, anthropometrical and biochemical characteristics over the 10-year period for all studied patients are shown in Table 1. Our study cohort included 63 patients who underwent gastric bypass, 50 women (79.4%) and 13 men (20.6%). The mean initial BMI was 55±10.2kg/m2. Despite the female-to-male ratio, BMI distribution was homogeneous between both genders. 66.7% of the patients had super-obesity, with a mean initial BMI of 60.4±7.7kg/m2 and a mean initial weight of 159.5±25.1kg (Table 2).
Clinical, anthropometrical and biochemical characteristics of the complete studied group during the 10 years follow-up period.
| Baseline | 6 months | 1 year | 5 years | 10 years | ||
|---|---|---|---|---|---|---|
| Gender (male/female) | 13/50 | – | – | – | – | |
| Number of patients | 79 | 72 | 71 | 69 | 63 | |
| Age (years) | 37.3±9.8 | – | – | – | – | |
| Weight (kg) | 147.7±27.3 | 111.4±22.4* | 96.9±21.0*,+ | 96.9±21.6* | 102.4±20.9*,+ | |
| BMI (kg/m2) | 55±10.2 | 41.7±8.7* | 36.3±7.8*,+ | 36.1±7.9* | 38.1±8.0*,+ | |
| %TWL | – | 24.6 | 34.2* | 34.4* | 29.8* | |
| %EWL | – | 42.3±14.4 | 58.3±14.4* | 57.2±18.8* | 50.6±21.7*,+ | |
| %EBL | – | 47.1±15.7 | 65.1±16.4* | 63.7±21.0* | 56.1±24.4*,+ | |
| Fasting glucose (mg/dL) | 116.5±45.9 | 92.8±16.9* | 87.8±13.7*,+ | 91.3±21.7* | 91.0±20.3* | |
| TC (mg/dL) | 187±42.1 | 154.6±31.3* | 153.3±33.3* | 160.9±32.5* | 168.1±33.7 | |
| TG (mg/dL) | Median | 125 | 103* | 81.5* | 73.5* | 85.5* |
| 25th percentile | 99 | 79.5 | 65 | 56.5 | 69.5 | |
| 75th percentile | 192.5 | 126 | 108.25 | 95 | 97.5 | |
| LDL-C (mg/dL) | 118.13±40.57 | 92.72±25.73* | 87.76±27.86* | 90.65±25.5* | 100.48±28.10+ | |
| HDL-C (mg/dL) | 43.32±8.58 | 41.66±10.1 | 46.68±11.5 | 54.51±11.74* | 57.3±13.1* |
All values are indicated as mean±SD, except for triglycerides, which are expressed as median, 25th percentile and 75th percentile.
Abbreviations: BMI: body mass index; %TWL: percentage total weight loss; %EWL: percentage excess weight loss; %EBL: percentage excess BMI loss; TC: total cholesterol, TG: triglycerides, LDL-C: low density lipoprotein cholesterol, HDL-C: high density lipoprotein cholesterol.
Initial anthropometric parameters and weight loss metrics in super obese (SOb) and morbid obese subjects (MOb).
| SOb | MOb | p, T-Student | |
|---|---|---|---|
| Gender (males/females) | 9/33 | 4/17 | 0.82 |
| Age (years) | 39.1±9.1 | 33.7±10.3 | 0.46 |
| Initial weight (kg) | 159.5±25.1 | 124.2±12.4 | <0.001 |
| Initial BMI (kg/m2) | 60.4±7.7 | 44.2±3.7 | <0.001 |
| BMI 10 years | 39.7±8.2 | 34.8±6.5 | 0.013 |
| %WL 1 year | 35.4±8.8 | 31.5±7.8 | 0.04 |
| %EWL 1 year | 56.2±13.5 | 62.6±15.6 | 0.122 |
| %EBL 1 year | 61.8±15.3 | 72.1±16.6 | 0.026 |
| %WL 5 years | 38.3±10.9 | 26.12±10.3 | <0.001 |
| %EWL 5 years | 59.1±16.8 | 53.8±22.2 | 0.345 |
| %EBL 5 years | 64.8±18.8 | 61.6±25.1 | 0.605 |
| %WL 10 years | 34.7±10.8 | 21.2±13.2 | <0.001 |
| %EWL 10 years | 53.9±17.4 | 43.8±27.8 | 0.140 |
| %EBL 10 years | 58.9±19.0 | 50.3±32.6 | 0.271 |
Results expressed as mean±SD. Bold indicates p<0.05.
Abbreviations: SOb: super obese; MOb: morbid obese; BMI: body mass index; %WL: percentage total weight loss; %EWL: percentage excess weight loss; %EBL: percentage excess BMI loss.
The greatest BMI reduction (%EBL 65.1±16.4) was achieved 1 year after surgery and the %EWL (58.3±14.4) topped out during that year. There was a 42.3% EWL at 6 months, 57.3% EWL at 5 years and 50.6% EWL after 10 years. MOb patients reached nadir or lowest BMI 1 year after RYGB (30.5kg/m2). In the SOb group BMI fell from 60.4kg/m2 to nadir BMI at 5 years (37.9kg/m2).
The maximal %TWL was observed at 1 year after surgery and was significantly higher in the SOb group compared to MOb group (31.5±7.8 vs 35.4±8.8; p=0.04). At 10-year follow-up %TWL fell to 21.2 in MOb group and maintained in 34.7 in the SOb group (p<0.001).
BMI after 10-year follow-up was independently predicted by baseline BMI. No independent effect of age or gender was observed on finally obtained BMI at 10 years. Using multiple regression analysis %EBL and %EWL at 10 years follow up was not independently predicted by age, gender or baseline BMI.
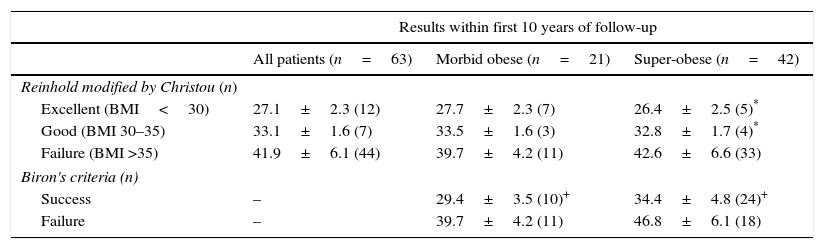
Table 3 illustrates Reinhold criteria modified by Christou and Biron's criteria for SOb and MOb patients at 10-year follow-up.
Gastric bypass results according to Reinhold classification modified by Christou and Biron's criteria at 10 years follow-up.
| Results within first 10 years of follow-up | |||
|---|---|---|---|
| All patients (n=63) | Morbid obese (n=21) | Super-obese (n=42) | |
| Reinhold modified by Christou (n) | |||
| Excellent (BMI<30) | 27.1±2.3 (12) | 27.7±2.3 (7) | 26.4±2.5 (5)* |
| Good (BMI 30–35) | 33.1±1.6 (7) | 33.5±1.6 (3) | 32.8±1.7 (4)* |
| Failure (BMI >35) | 41.9±6.1 (44) | 39.7±4.2 (11) | 42.6±6.6 (33) |
| Biron's criteria (n) | |||
| Success | – | 29.4±3.5 (10)+ | 34.4±4.8 (24)+ |
| Failure | – | 39.7±4.2 (11) | 46.8±6.1 (18) |
BMI results expressed as mean±SD.
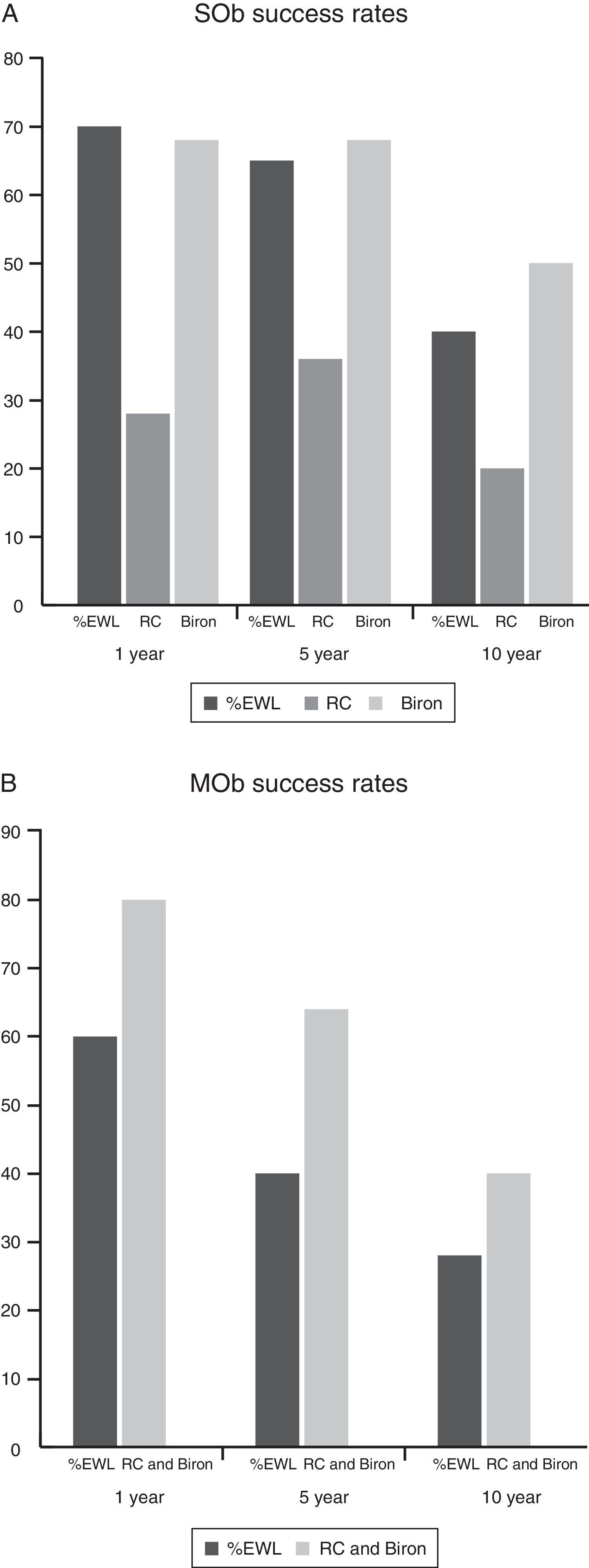
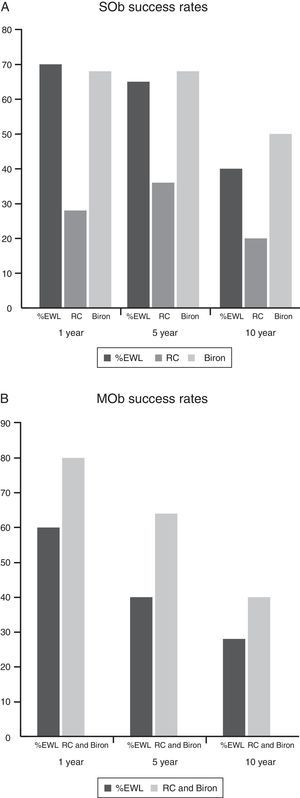
When comparing long-term success rate in MOb and SOb patients, better results were obtained in those with morbid obesity; obtaining a BMI<30kg/m2 in 33.3%, a good result (BMI 30–35kg/m2) was observed in 14.3% and treatment failure in 52.4%. Results for the SOb group widened markedly: 11.9% achieved a BMI<30kg/m2, 9.5% a good result (BMI 30–35kg/m2) and 78.6% had a final BMI>35kg/m2. Nevertheless, when considering initial BMI to define different goals (Biron's criteria) 57.1% success rate in super-obese patients was achieved (considering success if final BMI was below 40kg/m2) (Fig. 1).
Success rates 10-years after RYGB according to different criteria. (A) Success rates 10-year after RYGB in super-obese patients. (B) Success rates 10-year after RYGB in morbid-obese patients. %EWL: percentage excess weight loss; RC, Reinhold modified by Christou; Biron, Biron's criteria; SOb, super obese; MOb, morbid obese.
Regain of weight was observed in 79.4% of the patients after 10 years, with a mean weight gain of 14±9kg (range 1–40kg, median 12.1kg). It was considered after 5 and 10 years follow-up, affecting 65.7% and 79.4% of our patients, respectively. Significant differences between these two follow-up visits were found (%EBL 63.7 vs 55.8, p<0.001).
MortalityThree-month postoperative mortality rate in 79 consecutive RYGB was of 5.1% (n=4) due to acute peritonitis (1), enterocutaneous fistula (1), respiratory insufficiency (1) and one of unknown cause. During the follow-up, a patient died of renal carcinoma and another patient committed suicide. There are no available 10-year follow-up data of 10 patients, due to their referral to their local hospitals. The remaining 63 patients are the ones that have been subject of this study, and no deaths have been reported in the 10-year period.
ComorbiditiesAfter 10 years, marked reduction in the frequency of diabetes, dyslipidaemia, hypertension and obstructive sleep apnea was observed.
Diabetes and impaired fasting glucoseThe percentage of studied obese people with normal fasting glucose values at baseline (fasting plasma glucose <100mg/dL) was 54% and 46% showed impaired fasting glucose values (fasting glucose 101–125mg/dL at baseline). 10 years after surgery, the percentage of subjects with normal fasting glucose values significantly increased to 94% and only 6% of the subjects showed fasting glucose plasma values between 101 and 125mg/dL, p<0.0001.
A total of 21 (26.6%) obese people were diagnosed of diabetes at baseline. 39% of them (8 subjects) were detected after the glucose oral tolerance test.
Known diabetic patients were treated at baseline: 4 with diet, 6 with metformin, 1 with a combination of metformin with sulfonylurea, 1 with insulin therapy and 1 with a combination of insulin and metformin. None of the 8 detected patients after the oral glucose tolerance test at baseline needed pharmacological treatment for metabolic control.
15 people with diabetes could be followed after 10 years. Among them, 12 presented complete remission of the disease (80%), 2 presented partial remission and 1 continued with diabetes mellitus.
Persistence of diabetes was not associated with a %EWL or regained weight. The maximal decrease in fasting plasma glucose was observed at 1 year after surgery. Using multiple regression analysis and independent variables age, gender, baseline BMI, BMI, %EWL and %EBL at 10 years, only fasting glucose at baseline independently predicted glucose at 10 years follow up.
DyslipemiaDyslipidemia was observed in 11 (13.9%) of the patients prior to surgery. Pharmacological treatment of dyslipemia at baseline was: 6 patients with statins and 3 patients with a combination of statins and fibrates.
10 years after surgery, 7 patients showed improvement of total cholesterol (TC) levels and triglycerides plasma values (TG) and the condition was resolved in the remaining 4 (normal lipids levels an no hypolipidemic medication). Maximal decrease in TC was observed at 1 year and the maximal decrease in TG at 5 years after surgery. No significant independent effect of age, gender, baseline TC, baseline TG, baseline BMI, BMI, %EWL and %EBL at 10 years on total cholesterol or triglycerides was found.
From the total 79 subjects studied at baseline, 69% showed normal TC values (TC<200mg/dL). 10 years after surgery, a significant increase in the percentage was observed (79% p<0.001). 80% of the 79 obese subjects showed fasting TG values below 150mg/dL and a significant increase to 94% (p<0.001) was observed after 10 years follow up. No significant improvement in target value of LDLc was observed after 10 years follow up (target value: LDLc <130mg/dL).
Hypertension23 out of 79 (29.1%) patients had hypertension at baseline. The pharmacological treatment of the patients was: 8 patients were treated with an angiotensin converting enzyme inhibitor, 4 with diuretics, 2 with a calcium channel antagonist, 5 with a combination of angiotensin converting enzyme inhibitor and diuretics and 2 with a combination of diuretics and calcium channel antagonist. The remaining 2 were not taking antihypertensive treatment.
After the follow-up period, the condition resolved in 4 (normal blood pressure and no antihypertensive medication use), improved in 11 (reduction of drug number, drug dosage or better control) and remained unchanged in 8.
Obstructive sleep apneaFrom the 19 patients (24.1%) that had a diagnosis of obstructive sleep apnoea at baseline, this condition improved in 14 subjects. These 14 subjects did not need non-invasive assist respiratory devices 10 years after surgery. During follow-up period, a previously healthy patient was diagnosed of obstructive sleep apnoea.
DiscussionOur results show that super-obese and morbidly obese patients who underwent bariatric surgery presented a sustained absolute weight loss. However, compared to that observed in morbidly obese patients, the results in the super-obese group were significantly lower. When comparing different evaluation weight criteria, those criteria that consider the patient's initial weight are of greater utility in super-obese patients (Table 3). Independently of the success results in anthropometric parameters obtained and despite of non-achievement of normal weight a resolution of obesity related comorbidities was observed.
The effectiveness of the bariatric procedure is frequently defined by a 50% or above EWL maintained for 5 or more years. In our cohort this effect was achieved in 47.6% of the patients at 10 years follow-up. Recently, a %EWL of 58.9% at 10-year follow up was observed15 using laparoscopic procedure in 134 morbid obese subjects. However, in this study the prevalence of super obese subjects was 39%.
Our 10-year success rates analysed according to Reinhold modified by Christou8 and Biron9 criteria for the 63 patients were 30.2% and 54%, respectively.
Considering SOb patients’ success rates at 10 years, these were lower by Reinhold modified by Christou's criteria (21.4%) as seen in those reported previously involving patients with a high prevalence of super-obesity.16 However, when considering initial BMI to define an aimed BMI below 40kg/m2 (Biron's criteria) a 57.1% success rate was achieved after 10 years. Still and all, the purpose of bariatric surgery is to induce clinically important weight loss, enough to reduce obesity-related comorbidities to an acceptable level, decreasing mortality and enhancing quality of life. As Buchwald et al. found, weight loss after bariatric surgery (EWL 61.2% in their meta-analysis) is associated with metabolic improvements, ameliorating type 2 diabetes, hypertension, sleep apnoea and dyslipidemia.6 Our results, with a mean 50.6% EWL after 10 years, show similar improvements.
10 years after surgery, 80% of the patients with diabetes presented a complete remission of the disease. Among non diabetic subjects, 94% showed normoglycemia (fasting plasma glucose<100mg/dL) and only 6% showed impaired fasting plasma glucose values.
Different studies focused on morbidly obese patients after a postoperative 5-year follow-up have consistently documented sustained diabetes remission in 30–63% of patients, with a median disease-free period among individuals with Roux en- Y gastric bypass of 8.3 years.17 Our results are relevant due to the high remission rate of the disease in a group with high frequency of super-obese patients.
Beyond improving glycemia, bariatric surgery has showed additional health benefits, including greater reductions compared with medical/lifestyle interventions in other cardiovascular disease risk factors. In our study, 10 years after surgery 79% of obese subjects showed a TC plasma value below 200mg/dL and 94% a TG plasma value below 150mg/dL. Besides, in 15 of the 23 subjects with hypertension, the condition improved and 14 from the 19 patients with OSA do not need invasive assist respiratory devices 10 years after surgery.
Our main limitations were: (a) the loss of some of the initial cases – 63 out of the 79 patients completed the 10-year follow-up period. This was due to referral of some of the patients to their local hospitals after five-year follow-up; (b) that the included patients are a sub-set of the total treated patients; (c) the size of the sample is small and this is a limitation concerning the comparison of parameters between the two studied groups; (d) OSA: during the follow up period, polysomnography was not performed in all subjects.
Nevertheless, in this study we report that sustained weight loss is found both in morbid and super-obese patients, with improvement of comorbidities after long-term follow-up period. As the amount of weight loss was not associated with improvement of metabolic comorbidities, our results and others, support the use of compound success indexes that take into consideration metabolic improvements and the increase in quality of life, beside anthropometric changes.
ConclusionsIn conclusion, the present study of RYGB shows that at 10 years after gastric bypass, 50.6% of the excess weight remains lost and comorbidity improvement accompanies, despite the high quantity of super-obesity subjects treated (66.7%). Therefore, gastric bypass is an effective treatment for severe obesity at a long-term follow-up, even for patients with baseline BMI>50kg/m2.
FundingThis work has been supported by grants from Fondo de Investigaciones Sanitarias to Jose T. Real (FIS PI 12/01978).
Conflict of interestThe authors declare that they have no conflict of interest.